ABSTRACT
Cerebral venous air embolism (CVAE) is an extremely rare phenomenon. Most reports of cerebral air embolism focus on the arterial territory, and consequently CVAE has remained poorly understood, especially regarding its pathophysiology and treatment. The authors describe an elderly male patient who was admitted through the Emergency Department with subacute confusion. A brain computed tomography (CT) showed multiple cerebral venous gas emboli. No potential causes were found apart from previous peripheral vein cannulation and intravenous medication administration. The patient received supportive treatment, with complete radiological resolution of the gas emboli, while maintaining his previous confusional state. The aim of this report is to highlight a rare and understudied entity, and discuss its causes, proposed pathophysiology and appropriate management.
LEARNING POINTS
- Cerebral venous air embolism (CVAE) is a very rare phenomenon, assumed to result from retrograde progression of air bubbles introduced into the venous circulation through central venous catheter manipulation or, less often, peripheral vein cannulation, although its precise pathophysiology remains to be completely understood.
- CVAE’s clinical presentation can be varied, often mimicking acute stroke, and diagnosis can easily be established through a conventional brain-CT scan.
- Treatment must be initiated promptly by placing the patient in the Trendelenburg position and providing high concentration oxygen, intravascular volume expansion and other supportive measures as needed; hyperbaric oxygen therapy may be considered for selected patients.
KEYWORDS
Cerebral venous air embolism, aetiology, treatment
CASE PRESENTATION
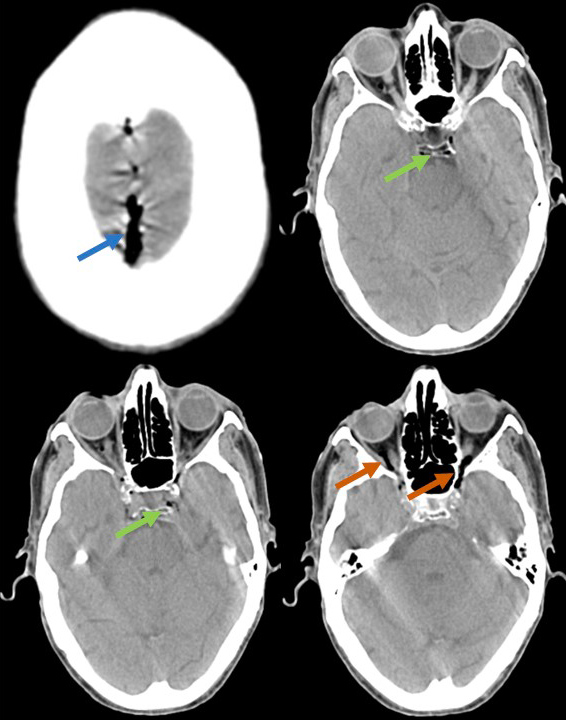
The authors describe the case of an 87-year old male patient, with known congestive heart failure secondary to ischaemic heart disease and parkinsonism. He presented at the Emergency Department with subacute confusion, resting dyspnoea and peripheral oedema, having been examined 6 days previously in the same department, due to similar complaints, and discharged after receiving intravenous diuretics. On examination, the patient was awake, although globally disoriented, without other neurological deficits; he was haemodynamically stable, with clear heart sounds and chest auscultation. He had a brain computed tomography (CT) which showed air bubbles in the cavernous sinuses, superior sagittal sinus, straight sinus and ophthalmic veins (Fig. 1). The patient received supportive treatment with cautious intravenous hydration (due to his known congestive status) and 100% oxygen therapy.
Figure 1. Conventional brain-CT scan showing air in the superior sagittal and cavernous sinuses (blue and green arrows, respectively), as well as in the ophthalmic veins (red arrows)
Subsequent brain-CT scans showed complete reabsorption of the gas emboli, as the patient maintained his previous confusional state, without new deficits. Other than the previous history of peripheral vein cannulation and intravenous medication administration, no additional aetiology or risk factors were evident to explain our findings. Unfortunately, the patient’s clinical status deteriorated, and he died due to sepsis secondary to nosocomial pneumonia.
DISCUSSION
Cerebral air embolism (CAE) is a rare phenomenon, although its true incidence is unknown, often with high morbidity and mortality. The term refers to the presence of air in the arterial (cerebral arterial air embolism, CAAE) or venous (cerebral venous air embolism, CVAE) vasculature, the latter being much less frequent than the former (and often underestimated), and, as such, less understood.
Most reviews and case reports focus on the more straightforward pathophysiology of the more common CAAE, which can result from paradoxical embolisation or direct entry of air into the arteries or pulmonary veins, as a consequence of cardiac or neurosurgical interventions, high pressure mechanical ventilation, thoracocentesis, central vein manipulation, peripheral vein cannulation and contrast injection, tissue biopsies or endoscopic procedures[1,2].
In contrast, the exact pathophysiology of CVAE remains to be clarified. Most authors agree that it is a result of retrograde (cranial) progression, through the jugular veins, of small low-weight air bubbles, able to overcome the opposing blood flow, in an upright patient. The entry of air into the venous circulation occurs after manipulation of a central or peripheral vessel (the latter case is less commonly described). Jugular vein insufficiency due to lack of valves and increased intrathoracic pressure have been proposed as factors contributing to CVAE[3,4].
CVAE’s symptoms are non-specific, with dizziness, vertigo, headache, confusion/disorientation, altered mental state, syncope, seizures, speech impairment, blurred vision, motor or sensory deficits and ataxia, mimicking other neurological disorders, such as acute stroke[4]. Diagnosis can easily be made by brain-CT scan.
CVAE can be fatal, with mortality dependent on the volume of air within the vessels, rate of accumulation and the affected territory. Since most reports focus on CAAE, treatment protocols have been assessed in these situations rather than in CVAE. Most authors recommend placing the patient in the Trendelenburg position, to promote the return of air bubbles into the central venous circulation. Otherwise, treatment is largely supportive, with high concentration (100%) oxygen administration (which contributes to bubble volume reduction) and intravascular volume expansion, to prevent further entry of air into the circulation. Hyperbaric oxygen therapy may be considered for more severe cases, although mortality benefits have only been studied in CAAE (by compressing existing air bubbles, creating high diffusion gradients and systemic hyperoxia and decreasing intracranial pressure, reducing brain vessel permeability, cerebral oedema and leukocyte adherence to the endothelium)[1,4].