ABSTRACT
Systemic lupus erythematosus (SLE) often presents with cytopenia(s); however, pancytopenia is found less commonly, requiring the consideration of possible aetiologies other than the primary disease. The authors describe the case of a female patient with a recent diagnosis of SLE admitted through the Emergency Department with fever of unknown origin and severe pancytopenia. She was medicated with prednisolone, hydroxychloroquine, azathioprine, amlodipine and sildenafil. Extensive investigation suggested azathioprine-induced myelotoxicity. However, the patient was found to have a concomitant cytomegalovirus (CMV) infection, with oral lesions, positive CMV viral load as well as the previously described haematological findings. Pancytopenia is always a diagnostic challenge, with drug-induced myelotoxicity, especially secondary to azathioprine, being a rare aetiology. This report reiterates the importance of the differential diagnosis of pancytopenia, especially in immunosuppressed patients with increased risk for opportunistic infections.
LEARNING POINTS
- The possibility of multiple aetiologies for pancytopenia in the same patient should be considered.
- Azathioprine-induced myelotoxicity is dose-dependent and pancytopenia is a rare form of presentation.
- Opportunistic infections should always be considered as a cause of cytopenias when immunosuppression is present.
KEYWORDS
Pancytopenia, systemic lupus erythematosus, azathioprine, cytomegalovirus
INTRODUCTION
Systemic lupus erythematosus (SLE) is a chronic inflammatory disease affecting multiple organs and systems. Cytopenias are common, however pancytopenia is found less frequently, requiring the consideration of possible aetiologies other than the primary disease. Active disease and immunosuppressive treatment should be the first possible causes to be considered[1].
CASE DESCRIPTION
The authors report the case of a 40-year-old female patient, with Hashimoto hypothyroidism and recently diagnosed SLE, medicated with prednisolone 60 mg/daily, hydroxychloroquine 400 mg/daily and azathioprine 100 mg/daily. She was admitted through the Emergency Department reporting a 4-day course of fever (39ºC), odynophagia and multiple and painful oral ulcers. On examination, she was febrile (38ºC) with extensive leucoplakia.
The patient was found to have severe pancytopenia (normocytic normochromic anaemia with a haemoglobin of 6.3 g/dl, leukopenia 350×106/l with neutropenia 120×106/l, and thrombocytopaenia 110×109/l) and mildly elevated inflammatory markers (C-reactive protein 5.96 mg/dl). Blood smear showed moderate anisopoikilocytosis with platelet anisocytosis.
The patient was prescribed piperacillin/tazobactam and fluconazole as a diagnosis of pancytopenia with neutropenic fever syndrome and oropharyngeal candidiasis was made. Additionally, azathioprine was suspended, due to potential drug-induced myelotoxicity. After resolution of the oral leucoplakia, multiple ulcers became evident, suggestive of viral or pemphigoid aetiology (Figs. 1–4).
Figure 1. Tongue lesion (day 8) Figure 2. Hard palate lesion (day 8)
Figure 3. Tongue lesion (day 16) Figure 4. Hard palate lesion (day 16)
No clinical or biochemical signs of active SLE were found, with normal complement and anti-dsDNA antibody levels. Vitamin B12 and folic acid levels were within the normal range. The patient was found to have positive IgM and IgG cytomegalovirus (CMV) antibodies, with a viral load of 2,800 copies/ml; testing was negative for other viruses, such as EBV, parvovirus, herpes simplex 1/2 and HIV. Blood, urine and bone marrow cultures were negative. Bone marrow aspiration was compatible with drug-induced agranulocytosis. Thiopurine methyltransferase (TPMT) was 11.9 U/ml (normal >19 U/ml).
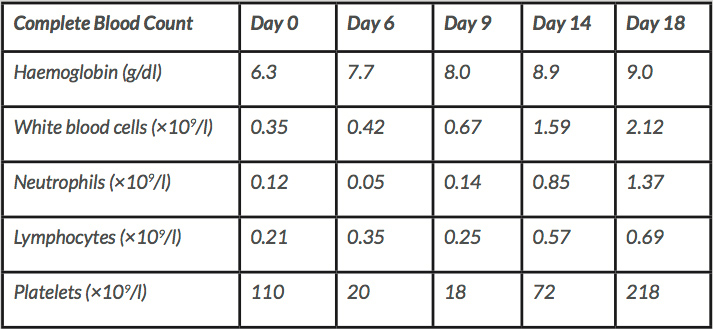
As previously stated, azathioprine was suspended, and the patient was prescribed valganciclovir 900 mg every 12 hours, with complete resolution of the oral ulcers and haematological improvement (Table 1).
DISCUSSION
Pancytopenia, defined as a reduction in all three peripheral blood lineages, can result from bone marrow infiltration, aplasia or increased cell destruction or sequestration. Disease severity is dependent on aetiology (for example, acute leukaemia) and clinical impact (for example, symptomatic anaemia or febrile neutropenia). It often represents a diagnostic challenge, mainly because patients are increasingly complex, often having multiple potential confounding (and contributing) comorbidities and medications.
In SLE patients, pancytopenia is often related to other causes, apart from the autoimmune condition, for example haemophagocytic lymphohistiocytosis, macrophage activation syndrome, septic or drug-induced myelotoxicity and haematological malignancies.
Azathioprine is often used as a steroid-sparing drug, interfering with purine and protein synthesis. TPMT is an important enzyme involved in azathioprine metabolization, with low blood activity being associated with increased risk for drug-related toxicity[2]. Azathioprine-induced myelotoxicity is dose-dependent and the most common effect is leukopenia (5–25%)[3]; pancytopenia is rare. SLE patients seem to be more susceptible to these adverse events[4], which tend to manifest in the first 3 weeks of treatment, and last for 3 weeks after drug suspension. Some patients may require colony-stimulating factors[5].
An additional remark regarding opportunistic infections and their contribution to myelosuppression is in order. CMV can remain latent after a primary infection and reactivate when allowed, especially in permissive immunological states, such as drug-induced immunosuppression. CMV infection can range from mild flu-like symptoms, to cytopenias, to severe acute (even life-threatening) syndromes, such as haemophagocytic lymphohistiocytosis. Recommended treatment is intravenous ganciclovir or oral valganciclovir.
CONCLUSION
This case report is extremely relevant since it illustrates the complexity of the differential diagnosis of pancytopenia, and how this disorder can result from a combination of multiple aetiologies (comorbidities, medication, acute infections) rather than just one: this patient had an autoimmune disease which often presents with cytopenias, she was medicated with a potentially myelotoxic drug and she had signs of ongoing CMV infection.