ABSTRACT
Posterior reversible encephalopathy syndrome (PRES) is a rare syndrome that presents with neurological manifestations, often associated with arterial hypertension. Magnetic resonance imaging (MRI) shows bilateral white matter oedema in the posterior vascular territories. Immunosuppression, (pre) eclampsia and autoimmune diseases can be implicated. A 27-year-old woman, with mixed connective tissue disease under azathioprine, was admitted in the emergency room in status epilepticus and with severe hypertension. The MRI showed bilateral oedema in a pattern compatible with PRES. There was clinical improvement after azathioprine suspension. PRES is typically reversible with prompt recognition of the syndrome and its trigger. The association with azathioprine is rare.
LEARNING POINTS
- Posterior reversible encephalopathy syndrome should be considered in patients with sudden onset of headache, altered consciousness and seizures.
- Recognition of this entity and identification of the trigger are essential for reversal of the clinical picture.
- Autoimmune diseases and some immunosuppressive drugs have been identified as causative, but reports of an association with azathioprine are very rare.
KEYWORDS
Posterior reversible encephalopathy syndrome, seizures, azathioprine
CASE PRESENTATION
We present the case of a 27-year-old woman with a history of mixed connective tissue disease, medicated with azathioprine 125 mg/day, with controlled disease. Within 1 month of azathioprine initiation, she complained of headache and palinopsia of 1 weeks’ duration. After a generalized tonic–clonic seizure, she was admitted to the emergency department in status epilepticus, presenting with high blood pressure (200/100 mm Hg), but without focal neurological signs. The laboratory findings were otherwise normal, with no inflammatory parameters or other relevant changes. The lumbar puncture was not suggestive of central nervous system infection.
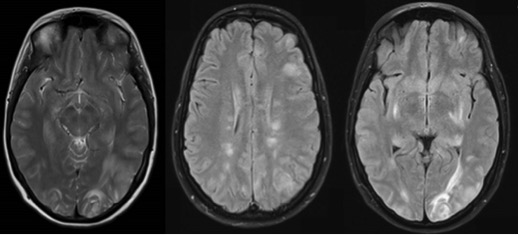
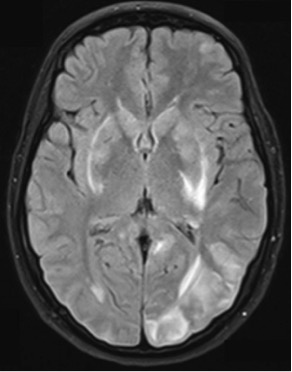
Magnetic resonance imaging (MRI) showed bilateral vasogenic oedema in the frontal, temporal, parietal and occipital cortico-subcortical regions compatible with reversible posterior encephalopathy (PRES) (Fig. 1) and a left occipital haemorrhagic lesion (Fig. 2).
The arterial study did not reveal any changes in the circle of Willis or neck vessels. Due to the refractory status epilepticus, the patient was intubated and ventilated. Azathioprine was suspended and, based on the suspicion that the autoimmune disease was the trigger, pulses of methylprednisolone were administered. The patient remained sedated for 48 hours, followed by neurological recovery and progressive regression of the MRI lesions.
Figure 1. Hyperintense bilateral heterogeneous T2 sign involving the frontal, temporal, occipital and parietal cortico-subcortical regions (diffusion-weighted), suggestive of vasogenic oedema and compatible with reverse posterior encephalopathy
Figure 2. Left occipital haemorrhagic lesion
With clinical improvement, after multidisciplinary discussion, it was decided to cease anticonvulsant therapy, resume previous medication with azathioprine and initiate steroid tapering. The patient was discharged after 26 days of hospitalization with no symptoms. However, 1 week after reintroduction of azathioprine at the previous dose, there was recurrence of the fronto-temporal headache, which was intense and pulsatile, and similar to that described before the diagnosis of PRES. A new MRI was performed and the result was similar to the previous findings: there was no clinical or analytical evidence of an autoimmune flare. Given the similarity of the complaints, it was assumed that the cause of PRES was azathioprine. There was complete resolution of the clinical picture with discontinuation of the drug.
DISCUSSION
PRES is a rare and possibly underdiagnosed syndrome, with no specific well-defined diagnostic criteria. Due to the lack of randomized studies, actual knowledge of this condition comes from case reports and retrospective studies[1].
PRES is characterized by several neurological signs and symptoms associated with typical imaging findings, corresponding to areas of vasogenic cerebral oedema[1]. It is defined as a clinical-radiological entity, with acute/sub-acute onset of headache, visual disturbances, nausea/vomiting, altered mental status, seizures and focal signs, usually associated with arterial hypertension[1,2].
Neuroimaging, in particular magnetic resonance findings, most often shows bilateral white matter oedema in the posterior vascular territories (parietal and occipital lobes)[2–4].
Its pathophysiology is still not fully understood, but an association with pre-eclampsia/eclampsia, immunosuppression and autoimmune diseases is documented[1,3]. PRES is typically a reversible condition if there is prompt recognition of the syndrome and its triggering factor. Treatment is mainly supportive and symptomatic, but it is essential to eliminate the precipitating cause and control elevated blood pressure[3,5]. Anticonvulsant therapy is recommended in patients with seizures, and can be discontinued when patients are asymptomatic and imaging abnormalities have resolved[1].
The association with autoimmune diseases and immunosuppressive therapy has been described, although the responsible mechanism is not fully understood. Reports have implicated different drugs, but the association with azathioprine is extremely rare[6]. In our case, the recurrence following reintroduction of the drug and clinical improvement with complete reversal of the clinical status following drug suspension/discontinuation is strongly suggestive of this association.