ABSTRACT
Secondary Parkinson’s disease or subacute Parkinson’s may occur after stroke, drug overdose carbon monoxide or manganese toxicity, and rarely owing to a brain tumor. Loss of dopaminergic neurons in the substansia negra pars compacta (SNc), or presence of the proteinaceous inclusions called Lewy bodies are thought to be the cause of Parkinson’s disease. Notwithstanding, in the past few decades, many case reports have been published describing Parkinson’s symptoms following either stroke, ischemia, toxicity, brain hemorrhage or rarely neoplasm.
LEARNING POINTS
- Brain tumours can cause secondary parkinsonism.
- This type of secondary parkinsonism improves when the tumour is removed.
KEYWORDS
Subacute Parkinson’s disease, meningioma
INTRODUCTION
Hitherto, only a handful of studies of case series have described the development of new onset Parkinson’s disease (PD) caused by a focal brain lesion, and report that the site of the lesion has no relationship with the nigrostriatal pathway[1–3]. In addition, the few case reports that have been published in peer-reviewed journals have shown that the location of the brain lesion varies[4].
Iatrogenic or drug-induced symptoms usually emerge as subacute PD, may cause significant disability (especially in older adults), and are difficult to treat. Iatrogenic subacute PD can take weeks or even months to resolve completely[5,6].
Joutsa et al. found that stroke and neoplasia in the medial frontal lobe, thalamus and midbrain tegmentum are by far the most common causes of subacute PD. Only 38% of such patients had unilateral Parkinson’s symptoms, and over 85% had received anti-Parkinson’s medication[3]. We present an interesting case of a large anterior cranial fossa meningioma with mass effect on the caudate presenting with secondary parkinsonism. There was mechanical compression of the basal ganglia without direct basal ganglia involvement.
CASE REPORT
A 65-year-old right-handed African American woman with no significant medical history presented with a 3-month history of progressive resting tremor of the right hand. The patient reported no headache or visual disturbance. On examination, she showed mild features of early PD, including bradykinesia and slight cogwheel rigidity at the elbows. Given the history of subacute onset of symptoms with progressive worsening, magnetic resonance imaging (MRI) of the brain with and without contrast was ordered. The MRI showed a mass measuring 5.7×4.2×5.6 cm in the anterior cranial fossa. This mass had a moderate mass effect with edema which was greater in the right than in the left lobe. The frontal horns were somewhat distorted and posteriorly displaced.
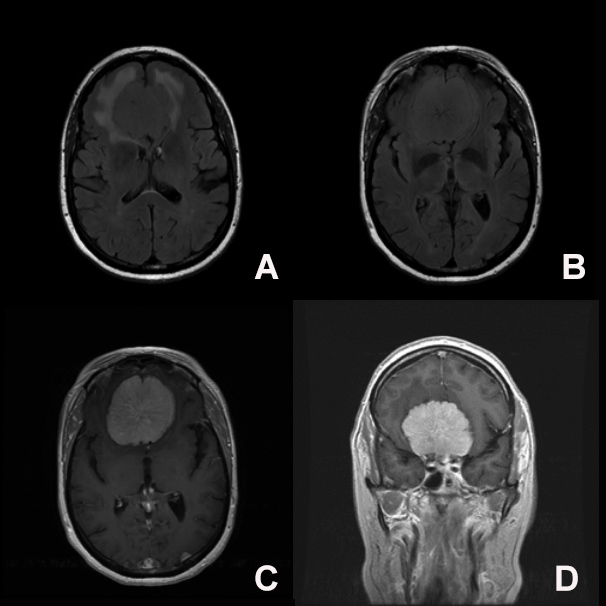
The mass extended into the anterior margin of the suprasellar cistern and was abutting the anterior margin of the optic chiasm. The mass was a dural-based lesion and avidly enhancing, which was consistent with a meningioma (Fig. 1).
Figure 1. T2 FLAIR axial images show a large anterior cranial fossa mass (bifrontal) with surrounding vasogenic edema with a mass effect upon the overlying medial frontal lobes bilaterally with downward compression and mass effect on the caudate (A, B). A large, avidly enhancing midline anterior cranial fossa mass with a maximum size of 5.7×4.2×5.6 cm is seen on axial and coronal sections (C, D)
The patient underwent tumor resection within 2 weeks. Following surgery, she noticed a gradual and continuous improvement in her tremor. The cogwheel rigidity improved after resection, but she continued to have stable mild right-hand resting tremor without further progression of the disease. Anti-Parkinson’s medication (carbidopa-levodopa) for mild residual parkinsonian features was discussed with the patient, but she chose to be observed only as symptoms did not affect her quality of life.
DISCUSSION
Intracranial mass lesions can cause parkinsonism and resting tremor. This is an uncommon cause of parkinsonism and should be considered in the differential diagnosis in patients with an acute or subacute presentation of symptoms[7]. Removal of the mass can improve the parkinsonian symptoms, although chronic compression of the basal ganglia from tumor mass effects may cause residual parkinsonian features[7]. Acute or subacute movement disorders may prompt patients to seek urgent medical attention, but movement disorders caused by a basal ganglia lesion usually progress only slowly[1–4]. Parkinson’s symptoms can be caused by tumors in different brain locations outside the nigrostriatal pathway, including the midbrain, thalamus, and cingulate cortex, as reported in some case reports[8-14]. Response to anti-Parkinson’s medications is often good, although complete remission may take weeks or months[8-14]. A thorough history should focus on medications, while a physical examination will help the correct diagnosis to be made promptly[5-8]. An accurate diagnosis is essential for successful management[4,13]. Symptoms in patients with slowly growing or benign brain tumors may mimic those of idiopathic Parkinson’s disease and can be misdiagnosed. However, an early diagnosis can be reached in these patients by obtaining neuroimaging studies such as computed tomography or MRI of the brain, thus reducing progression and facilitating early intervention[7].
CONCLUSION
We present an interesting case of a large anterior cranial fossa meningioma with mass effect on the caudate and presenting with secondary parkinsonism. Mechanical compression of the basal ganglia without direct basal ganglia involvement caused the patient to develop residual right-hand resting tremor despite surgical resection, which suggests chronic damage to the basal ganglia from the mass effect. Such patients can be challenged with dopamine agonists to monitor their response to treatment and assess future outcome.