ABSTRACT
Methamphetamine is a substance of abuse that is most commonly smoked. Both regular and non-regular use can cause toxic injury to the lung parenchyma, the signs and symptoms of which are non-specific. Clinical scenarios include non-cardiac pulmonary oedema, acute respiratory distress syndrome, alveolar haemorrhage, pneumonia and pneumoconiosis. As radiological imaging is often non-specific, a positive history of methamphetamine use is the only way to reach a definite diagnosis. The use of methamphetamine is now increasing in Europe, so it is important as physicians to be aware of this differential diagnosis in patients in respiratory distress with risk factors for illicit drug use.
LEARNING POINTS
- A case of methamphetamine-induced lung injury with non-specific findings is described.
- In those presenting with respiratory symptoms and no obvious cause identified, consideration must be given to a diagnosis of drug-induced lung injury.
- Treatment for methamphetamine-induced lung injury is supportive, for example with oxygen supplementation, and symptoms should resolve after cessation of use; there is no evidence that steroids are of benefit.
KEYWORDS
Methamphetamine-induced lung injury
INTRODUCTION
We describe a case of methamphetamine-induced lung injury in a patient presenting in acute respiratory distress with no obvious cause. Radiology findings were non-specific. On further history taking during his admission, the patient divulged that he had, in fact, been regularly smoking methamphetamine prior to admission. Symptoms resolved with supportive care and cessation of drug use.
CASE DESCRIPTION
A 44-year-old man presented to the emergency department with shortness of breath, a cough productive of pink, frothy sputum and palpitations. These symptoms had been progressively worsening over the previous 4 weeks. He was an active smoker, smoking 10 cigarettes per day since the age of 18 and also regularly smoked cannabis. He had no other past medical history or family history of note. On admission, he denied alcohol and other illicit drug use.
On examination, there was widespread polyphonic wheeze on chest auscultation with decreased air entry bilaterally. His chest x-ray (Fig. 1) showed patchy bilateral infiltrates, suggestive of atypical infection. On admission, he required 4 litres oxygen via nasal cannulae to maintain an oxygen saturation above 94% and his respiratory rate was 30 breaths per minute. His ECG showed sinus tachycardia. His C-reactive protein was 14 and white cell count was 13. All other blood results were within the normal range.
Figure 1. AP view chest X-ray showing bilateral patchy airspace opacification
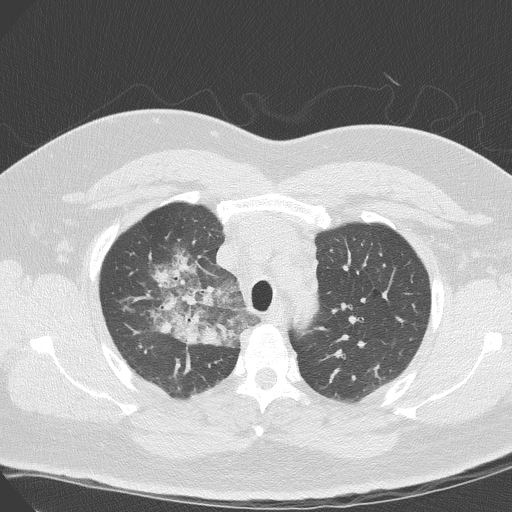
He was treated with regular bronchodilator nebulisers, nasal CPAP, IV co-amoxiclav (to treat suspected infection) and oral prednisolone. A CT of the thorax was done to further assess his lung fields. This showed an area of diffuse ground-glass change in the right upper lobe (Fig. 2). This was non-specific, and differential diagnoses at the time included pulmonary haemorrhage or interstitial/alveolar infiltration with inflammatory cells. There was no evidence of significant alveolar damage or air trapping. Minor scattered tree-in-bud changes were also demonstrated within the lung bases bilaterally.
Figure 2. CT of the thorax showing an area of diffuse ground-glass change within the right upper lobe
On further questioning, the patient admitted to smoking methamphetamine regularly during the previous 8 weeks and had last smoked the drug on the night prior to admission. The non-specific CT findings correlated with methamphetamine-induced lung injury. Antibiotics were stopped and the patient recovered over 5 days with supportive oxygen therapy and was discharged feeling well with a follow-up chest x-ray scheduled in 6 weeks.
DISCUSSION
Methamphetamine is an amphetamine-type drug that is most commonly smoked and causes the release of dopamine. It is neurotoxic to dopaminergic neurons in the midbrain. It was first synthesized from ephedrine in 1893 by a Japanese chemist and was originally used by German World War II soldiers for its performance-enhancing stimulation and effects of prolonged wakefulness. It is most commonly used in Australia and New Zealand, where it is manufactured in underground ‘meth labs’. Its use is now increasing in Europe, with the Czech Republic being the major European producer of the drug with 1,057 seizures of methamphetamine in 2015, compared with 306 a decade earlier[1]. Its popularity is increasing in the UK and Ireland, with 37 seizures in Ireland in 2013 and 27 in the UK in 2015; both countries had no seizures 10 years previously[1].
The clinical relationship between inhalation and lung injury is unclear and the pathogenesis of lung injury is unknown. Studies show that acute inhalation may be associated with increased free radical formation[2]. Reported cases of methamphetamine-induced lung injury include pulmonary oedema, eosinophilic pneumonia and pulmonary hypertension[3]. Pneumonia occurs as a result of contaminated drug use, changes in normal bacterial flora and aspiration. Typically, the chest x-ray shows bilateral increased opacities with or without pleural effusions and/or cardiomegaly, while CT of the thorax generally shows ground-glass changes. Symptoms clear rapidly with cessation of use and supportive therapy.