ABSTRACT
A 40-year-old man presented to the emergency department with dyspnoea and fatigue after bupropion and popper consumption. Clinical examination was remarkable for central cyanosis not responding to supplementary oxygen. Arterial blood gas analysis showed a methaemoglobin value of 30.3%. Methaemoglobinemia was diagnosed and the patient was treated with methylene blue. However, during methylene blue administration, the patient developed a generalized tonic-clonic seizure that was successfully managed with diazepam. Combined intoxications can be a critical problem in the emergency department. Early recognition and treatment of poisoning are key for good patient outcome.
LEARNING POINTS
- Distinguishing toxidromes is critical for adequate treatment of patients with drug intoxication; the most common side effect of bupropion consumption is dose-dependent seizures.
- The diagnosis of methaemoglobinemia requires a high index of suspicion, particularly in a patient presenting with central cyanosis not responding to supplementary oxygen.
- Treatment with methylene blue is recommended when the percentage of methaemoglobin is above 30% or when the patient has symptoms related to methaemoglobinemia.
KEYWORDS
Methaemoglobinemia, drug intoxication, bupropion
CASE PRESENTATION
A 40-year-old man medicated with bupropion 300 mg/day for opioid dependency and valproate acid 500 mg/day as a mood stabilizer was brought to the emergency department (ED) with dyspnoea and fatigue after ingesting 16 bupropion 300 mg tablets. At admission, the patient denied other therapeutic or illicit drug use.
On examination, the patient was confused and disorientated. Central cyanosis was present and peripheral oxygen saturation was 90%, despite administration of 100% oxygen through a non-rebreather mask. Heart rate was 127 beats/min and blood pressure was 134/84 mmHg. The airway was clear and pulmonary auscultation was normal. Arterial blood was brownish in colour and arterial blood gas (ABG) analysis showed a methaemoglobin level of 30.3%. Blood tests were otherwise normal, with a valproic acid level of 20 µg/ml (therapeutic level: 50–100 µg/ml).
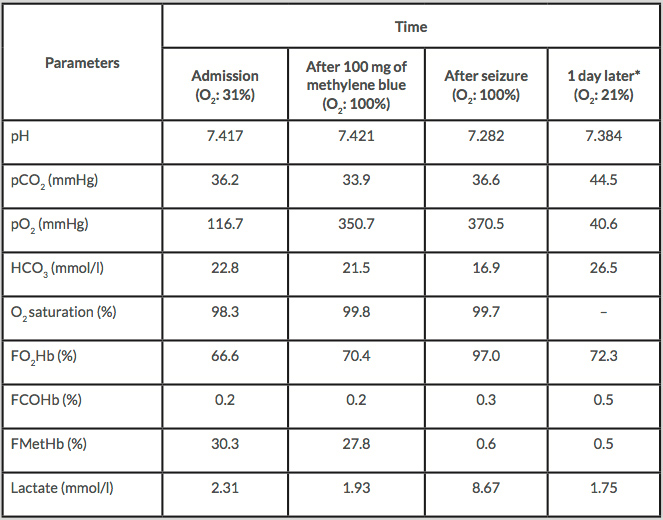
The diagnosis of methaemoglobinemia was made and the patient was administered 100 mg (1 mg/kg) of methylene blue in a 1% solution. As the methaemoglobin level was still high after the first infusion (Table 1), a second infusion of 100 mg was started (aiming at a total dose of 2 mg/kg). However, the infusion was discontinued due to a generalized tonic-clonic seizure after the administration of 50 mg. The seizure was successfully managed with diazepam 5 mg given intravenously. The methaemoglobin level was 0.6% when the seizure occurred. After recovering from the seizure, the patient acknowledged consumption of illegal poppers (alkyl nitrites) concomitantly with bupropion.
During hospital admission there was no secondary rise in methaemoglobin and no recurrence of seizures. The patient was discharged 3 days later.
DISCUSSION
In the ED, 1–3% of patients are diagnosed with intoxication due to therapeutic and/or illicit drug consumption[1,2]. Early recognition of different toxicological syndromes (toxidromes) is extremely important for the identification of specific classes of poison, particularly in large mixed drug overdoses[3,4]. Supportive care, appropriate decontamination, antidote administration and elimination enhancement are fundamental for the successful management of acute poisoning or drug overdose[3]. In cases of combined intoxication, medical emergencies such as methaemoglobinemia require prompt diagnosis and treatment[5–7].
We present a case of combined intoxication with alkyl nitrites and bupropion. Combined drug consumption can be complex to treat and represents up to 42% of drug intoxications in some centres[8]. The severity of the toxidrome depends on dose, exposure time, co-morbidities and coingestants[3].
Methaemoglobinemia is a rare condition and its diagnosis is difficult unless there is a high index of suspicion. It is an important differential diagnosis for patients presenting with central cyanosis that does not respond to oxygen therapy[5–7,9]. The condition is characterized by increased quantities of oxidized haemoglobin (with iron in its ferric form) which is useless as an oxygen transporter.
Methaemoglobinemia can be due to genetic conditions or acquired following exposure to drugs or toxins responsible for the oxidation of haemoglobin. Such drugs include dapsone, local anaesthetic agents and volatile nitrates[5]. Alkyl nitrites are used as recreational drugs and can cause methaemoglobinemia[10].
Levels of methaemoglobin below 2% are not harmful[5,6], levels above 20% are associated with dyspnoea, tachycardia, headache and lethargy, and levels above 55% are life-threatening. Treatment is recommended in symptomatic patients or patients with levels above 30%[5]. Methylene blue is the first line of treatment for this condition and reduces the level of methaemoglobin via nicotinamide adenine dinucleotide phosphate (NADPH) methaemoglobin reductase. The recommended dose is 1–2 mg/kg administered intravenously over 5 minutes that can be repeated with 1-hour intervals up to the maximum of 7 mg/kg[5,7]. Treatment with methylene blue is not effective in cases of low NADPH[11]. If treatment with methylene blue fails, the second line treatment is exchange transfusion[6].
Bupropion is a norepinephrine-dopamine reuptake inhibitor and a nicotinic acetylcholine receptor non-competitive antagonist used to treat depression and nicotine addiction[12]. It enhances both dopaminergic and noradrenergic neurotransmission, which is the mechanism responsible for its adverse effects of restlessness, tremors, insomnia, tachycardia, conduction defects and seizures. Seizures are the most important side effect of this drug and are dose-dependent. The reported incidence is 5% in patients on a daily dose of 600 mg and 33% in cases of overdose[12–14].
Methylene blue inhibits the action of monoamine oxidase A and is contraindicated in patients medicated with serotoninergic drugs because it can induce serotonin syndrome[15]. Methylene blue can lower the seizure threshold in patients medicated with bupropion and enhance aminergic synaptic neurotransmission[16].
In our patient, although the seizure was most likely caused by bupropion intoxication, methylene blue was stopped due to concerns about the possible development of a serotonin syndrome.
CONCLUSION
This case highlights the complexity of combined intoxication in the ED and the importance of a prompt diagnosis of methaemoglobinemia with ABG analysis. Nowadays, as more complex recreational drugs such as alkyl nitrites are easily available, ED staff should be able to recognize and treat intoxication by these drugs. In combined drug intoxication, it is critical to recognize toxidromes, treat them accordingly and be aware of possible interactions between substances and treatments.