ABSTRACT
We report a case of brainstem infarction following a C5–C6 cervical transforaminal injection, a rare and serious neurological complication of this procedure. Cervical transforaminal steroid injection is a common therapy for patients with persistent cervical radiculopathy not relieved by conservative treatment, and is effective in 65–70% of cases. Unfortunately, this procedure may lead to serious complications such as neurological damage. These complications are rare but potentially fatal, as reported in our case. Complications could be due to three mechanisms: the technique itself, the cervical vascular anatomy and the properties of the product (corticoids). The neurological complications can be diagnosed through brain MRI. This case report focuses on the importance of a risk/benefit evaluation when performing this medical procedure.
LEARNING POINTS
- Physicians should be better informed about severe complications following cervical transforaminal epidural steroid injections and their strict indications.
- Severe adverse events are rare but they can be disastrous.
- Non-particulate corticosteroid should be used.
KEYWORDS
Cervical epidural steroid injection, ischaemic stroke, MRI
INTRODUCTION
Cervical transforaminal epidural steroid injections (CTFESIs) are widely performed as a non-surgical approach for the management of cervical radiculopathy. Usually, minor adverse events are reported (neck pain, headache, facial flush), but severe complications have been described in the literature[1]. Therefore, patients should be aware of the potential complications of this procedure. These are mainly infectious (abscess, meningitis), haemorrhagic (epidural haematoma) and ischaemic (brainstem or spinal cord infarction)[2].
We report a case where a CTFESI procedure resulted in a fatal brainstem stroke with tetraplegia.
CASE PRESENTATION
A 72-year-old woman presented with a 6-month history of cervical pain radiating to the left arm. Her past medical history was not relevant. Clinical examination was consistent with C6 radiculopathy but without sensory or motor involvement. MRI and a cervical scan confirmed cervical disc protrusion and narrowing of the left foramina at the C5–C6 spinal segment.
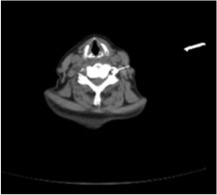
The patient was first unsuccessfully treated with analgesics and non-steroidal anti-inflammatory drugs, so a CT-guided transforaminal cervical injection was discussed. This procedure was performed according to the current medical guidelines (Fig. 1). Immediately after the procedure the patient complained of general weakness followed by loss of consciousness and stiffness of the four extremities. She was immediately transferred to the emergency department.
Figure 1. Foraminal infiltration of the cervical spine. The tip of the spinal needle is located in the transverse foramen. Extravascular diffusion of the contrast agent, no enhancement of the vertebral artery appear (washing).
Upon her arrival at the emergency department, her blood pressure was 230 mmHg, heart rate was 100 bpm, oxygen saturation was 90% on room air and body temperature was 37.5°C.
The initial neurological examination showed a Glasgow coma score of 3/15 (E1V1M1), total quadriplegia and spasticity of the four extremities. Cranial nerve examination showed oculomotor palsy and skew deviation. The rest of the examination was normal. A complete blood count, electrolytes, blood gases and renal function tests were normal. The patient was intubated to protect the airway and further imaging tests were performed to rule out a cerebrovascular accident.
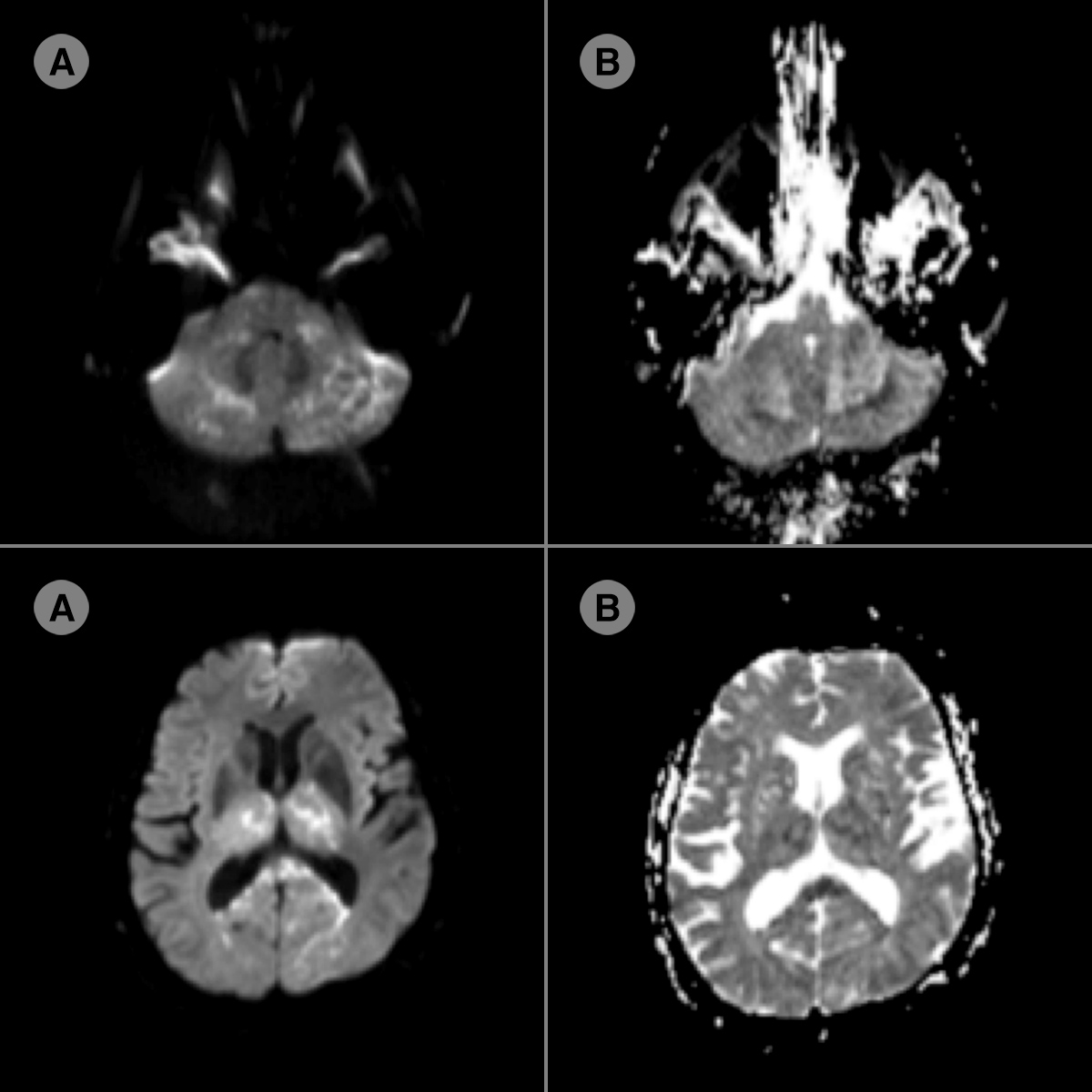
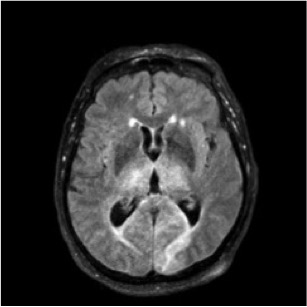
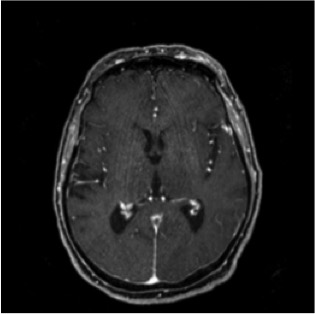
CT angiography including the supra-aortic trunks was normal, but MRI showed acute bilateral ischaemic lesions in the thalamic nuclei, microlesions in the two posterior cerebral territories and bilateral lesions in the brainstem and cerebellar hemispheres (Fig. 2). These lesions as well as perilesional oedema were noted on the FLAIR sequence (Figs. 3 and 4). The electroencephalogram (EEG) showed slowing of the baseline rhythm and absence of epileptic activity.
Figure 2. Diffusion MRI (A) with ADC mapping (B) sequences: in the basilar and posterior cerebral artery territories, multiple foci of diffusion restriction (hyperintensity) with a dropped bilateral ADC signal (hypointensity) are seen
Figure 3. FLAIR sequence on MRI showing hyperintense foci on bilateral thalamic and occipital lobes (posterior cerebral artery territories)
Figure 4. Angio-MRI showing no rupture of the blood–brain barrier. The vertebral arteries, the basilar trunk and Willis polygon are free of occlusion
The presence of ischaemic stroke was confirmed. The patient was transferred to the intensive care unit where transoesophageal echocardiography was performed. The suspicion of cardioembolic stroke was formally excluded and cardiac monitoring showed no arrhythmias. No clinical improvement was observed after 72 hours of hospitalization so life-sustaining treatment was stopped, leading to the death of the patient.
DISCUSSION
Epidural glucocorticoid injections (CFTESIs) are usually performed for the management of persistent radicular pain syndromes. They are considered to improve the clinical picture in 65–70% of patients.
Complications of cervical epidural glucocorticoid injections are rare and mostly minor: headache, increased radicular pain, facial erythema and vasovagal reaction[1,2]. The development of tetraplegia as described in our case is very rare. However, other serious complications of cervical transforaminal injection have been recently reported in the literature. These include a wide range of conditions such as spinal cord infarction due to trauma of the anterior spinal artery, cerebellum or brainstem infarction, or even death[3].
A study by Scanlon et al. identified 54 neurological complications out of 78 complications recorded: 30 spinal, brainstem or cerebellum infarctions and 24 other neurological complications including 13 deaths[4]. Data on the incidence of these complications are unavailable due to the lack of information in the scientific literature. The current estimated risk of complications from transforaminal injection ranges from 1/100,000 to 1/1,000,000.
The aetiology of brain and spinal cord infarctions after a transforaminal injection is uncertain but a few mechanisms have been described[5,6]. Previous spinal surgery is often cited as a risk factor but without any objective evidence. The infarctions are considered to be the result of vascular mechanisms related to clinical presentation and lesions described on imaging.
Occlusion of a vertebral or radicular artery leading to infarction can be caused by artery trauma, vasospasm and extrinsic compression by the injected product, arterial dissection, or particulate steroid embolism via intra-arterial injection[7,8]. The majority of severe cases described after cervical injection are the result of a vertebral artery lesion.
Some reports described anastomoses between the vertebral and cervical arteries in the posterior part of the intervertebral foramina of some patients. This could present another risk factor for complications as particles could enter the vertebral artery via the anastomoses and cause distal infarction.
The rate of inadvertent intravascular injection instead of foraminal injection is about 10.8%, and in 74% of cases reflux manoeuvres are falsely negative. These manoeuvres have a very low sensitivity and must be routinely performed even though the risk of intravascular injection is not completely excluded[9,10].
As described, foraminal injection can result in a vascular lesion or intra-arterial injection. The presence of acute stroke in a specific vascular territory of the brain, the spinal cord or the cauda equina (diffusion hyperintensity and hypo signal on the ADC map) supports the vascular mechanism of these complications[9,10]. In addition, corticosteroid solutions are preferred for infiltration as injectable steroids in suspension contain microcrystals capable of clogging arterioles 5–10 μm in diameter.
The choice of glucocorticoid injected is important as the injection of particulate glucocorticoids (Solu Medrol, Depo Medrol) is more likely to cause embolism in arteries 5–10 µm in diameter, and is associated with distal infarcts. This association has not been demonstrated with non-particulate glucocorticoid (dexamethasone)[10], which is therefore recommended and widely used.
In the case presented, the brain MRI suggested direct embolism after intravascular injection rather than arterial spasm or direct arterial trauma. In addition, the corticosteroid used reinforces our hypothesis for the reasons mentioned above.
CONCLUSION
Transforaminal injection is a non-surgical treatment for radiculopathy but may result in complications. Severe adverse events are rare but they can be as disastrous as the tetraplegia described in this case. Epidural corticosteroid injections should be considered in appropriate cases but performed cautiously. Ideally, a non-particulate corticosteroid should be used.