ABSTRACT
The presence of different autoimmune disorders in the same individual is called multiple autoimmune syndrome (MAS). One of these co-occurring conditions is autoimmune haemolytic anaemia (AIHA), which is characterized by the production of autoantibodies against red blood cells due to immune system malfunction and which results in severe tissue oxygenation disturbance. AIHA is not uncommon but occurs rarely in MAS; if it does, MAS is then classified as MAS type III. Herein, we describe a case of MAS type III including AIHA which was successfully treated with hydrocortisone with gradual resolution of symptoms.
LEARNING POINTS
- The co-occurrence of multiple autoimmune disorders in the same individual is called multiple autoimmune syndrome (MAS).
- Autoimmune haemolytic anaemia is not uncommon but rarely occurs in MAS.
- The presence of one autoimmune disease should alert the physician to the possible presence of others.
KEYWORDS
Haemolytic anaemia, autoimmune syndrome, Addison's disease
INTRODUCTION
Different autoimmune disorders occurring in the same individual is called multiple autoimmune syndrome (MAS) which is seen in approximately 25% of individuals with a single autoimmune disease[1]. The most frequent autoimmune diseases in such patients include dermatological conditions like alopecia areata or vitiligo[2]. The main aetiology of MAS is unclear, but a combination of genetic susceptibility and environmental triggers may be involved[3]. MAS is categorized as types I to III depending on the underlying autoimmune disorders. MAS type III includes autoimmune dermatological (vitiligo, dermatitis herpetiformis), thyroidal (thyroid autoimmune disease), neurological (myasthenia gravis), haematological (pernicious anaemia, autoimmune haemolytic anaemia (AIHA), idiopathic thrombopenic purpura), rheumatological (Sjogren's syndrome, systemic lupus erythematosus) and metabolic disturbances (type 1 diabetes mellitus, Addison's disease)[4]. AIHA is characterized by the production of autoantibodies against red blood cells due to immune system malfunction which leads to severe tissue oxygenation disturbance[5]. Although AIHA is not uncommon, it is rare in MAS. Here we describe a case of MAS that manifested with AIHA.
CASE PRESENTATION
A 30-year-old woman presented to hospital with a 1-week history of acute weakness, exertional dyspnoea and icterus. Her medical history revealed hypothyroidism for the last 12 years. A combination of weight loss, anorexia and hyperpigmentation had led to a diagnosis of Addison’s disease approximately 4 years previously. Her family history included both hypothyroidism and rheumatoid arthritis in her mother. She was taking various medications including fludrocortisone 0.1 mg daily, hydrocortisone 10 mg three times a day, levothyroxine 0.1 mg daily and folic acid 5 mg twice a day. The patient was alert and oriented, and had no difficulty in obeying commands.
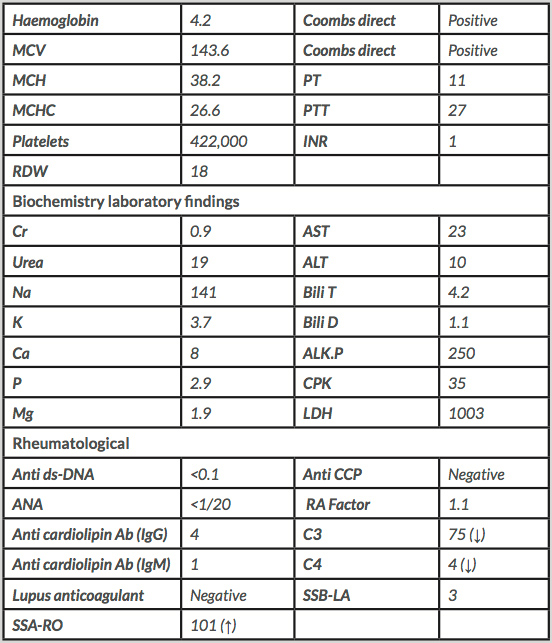
On physical examination, her vital signs were in the normal range as follows: temperature of 36.3ºC, systolic/diastolic blood pressure of 90/60 mmHg, pulse rate of 104 per minute, and respiratory rate of 22 per minute. However, she was pale and the conjunctiva was mildly icteric despite the absence of hepatosplenomegaly or lymphadenopathy. The neurological examination was normal. Laboratory tests (Table 1) revealed a serum haemoglobin level of 4.2 g/dl, serum LDH level of 1003 IU/l, total bilirubin of 4.2 mg/dl and direct bilirubin of 1.1 mg/dl. A direct Coombs test was normal. The co-occurrence of hypothyroidism, Addison's disease and haemolytic anaemia led to the diagnosis of MAS type III. Intravenous hydrocortisone 100 mg three times a day was therefore started and resulted in significantly increased haemoglobin levels. A week after treatment initiation, dyspnoea and other symptoms had diminished and the anaemia had responded well. The patient was discharged in a good general condition on oral azathioprine 50 mg daily and oral prednisolone 60 mg daily. Laboratory tests 1 week later were normal with a serum haemoglobin level of 13.8 g/dl, haematocrit of 41.7%, reticulocyte count of 2.4%, platelet count of 542,000/mm3 and ESR of 11 mm/hour.
DISCUSSION
It has been suggested, but not definitely demonstrated, that different infectious, genetic, immunological and even psychological factors can trigger MAS: genetic susceptibility and environmental triggers may interact to cause the condition. The predominant role of immunological responses is supported by a report that autoantibodies affect multiple organs in MAS[6]. The case described here is a typical form of MAS type III caused by three autoimmune disorders including hypothyroidism, Addison's disease and AIHA. The patient was successfully treated with hydrocortisone and then prednisolone, with treatment gradually having an effect over 2 weeks.
A study conducted in 2016 by Harpreet et al.[7] described a 32-year-old woman who presented with multiple symmetrical articular pains and stiffness accompanied by hypothyroidism and microcytic hypochromic anaemia as shown by a serum haemoglobin level of 8.2 mg/dl. MAS with coeliac disease has also been described. In 2011, Topal et al.[8] reported the co-occurrence of an autoimmune thyroid disorder, vitiligo (with multiple depigmented macules and patches) and ulcerative colitis (characterized by haemorrhagic oedematous mucosa of the colon) finally diagnosed as MAS in a 47-year-old woman. in 2014, Masood et al.[9] described a 42-year-old female patient with MAS with AIHA, systemic lupus erythematosus, psoriasis and type 1 diabetes mellitus. Similarly to our case, that diagnosis of AIHA was based on positive IgG findings on a disturbed immune response background. Likewise, treatment with immunosuppressant medication resulted in full resolution of symptoms.
A few cases of primary AIHA have been reported, but secondary causes, especially autoimmune diseases and lymphoproliferative disorders, are demonstrated in up to 80% of patients with AIHA[10]. In our case, a direct antiglobulin test (DAT) and Coombs test revealed warm-type IgG autoantibodies in serum. The majority of warm-form AIHAs are idiopathic or associated with another autoimmune disease[11]
In conclusion, the presence of one autoimmune disease should alert the physician to be watchful for the presence of another. The occurrence of AIHA in a patient with a positive family history for other autoimmune diseases may be suggestive of MAS and indicates the need for continued surveillance for the development of autoimmune disease in predisposed patients.