ABSTRACT
Introduction: Extramedullary plasmacytomas are present in 13% of multiple myeloma (MM) patients. Less than 5% of MM cases are non-secretory. The orbital location is uncommon and a minority of orbital tumours are plasmacytomas.
Description: The patient was a 71-year-old man, with right proptosis, retro-ocular pain and epistaxis with visual acuity 2/10, limitation of upper eye movement and scattered ecchymosis. Blood tests revealed severe anaemia, coagulopathy, increased serum creatinine, LDH and C-RP without improvement after antimicrobial treatment. Peripheral immunophenotyping showed 9.4% of plasma cells with intracytoplasmic clonal κ chains. IgG and λ chains were decreased with normal plasma and urine immunofixation. Orbital CT: retro-orbital superomedial tumour with bone destruction. Histology of the tumour and bone biopsy was consistent with plasmacytoma. The patient was deceased in 2 weeks.
Discussion: MM accounts for 10% of haematopoietic tumours; 7% of cases present with plasmacytomas at diagnosis. Orbital locations are rarely reported (frequently in the temporal region). Proptosis, ptosis and reduced visual acuity are common symptoms. However, orbital pain is less frequent. Most cases of MM demonstrate hypergammaglobulinaemia. Only 5% of MM cases are non-secretory.
The uncommon location, topography, symptom peculiarities and absence of monoclonality led to the diagnostic challenge of this fatal case of MM.
LEARNING POINTS
- Multiple myeloma (MM) represents 10% of malignant haematologic disease, 13% of which presents plasmacytomas (mostly in the axial skeleton).
- Orbital plasmacytoma is an uncommon presentation of MM and only 1% of orbital tumours are plasmacytomas. Proptosis is the most common symptom.
- Although the majority of MM cases demonstrate hypergammaglobulinaemia, non-secretory MM is described as constituting less than 5% of cases.
KEYWORDS
Multiple myeloma, orbital tumour, plasmacytoma
CASE DESCRIPTION
A 71-year-old man presented to the emergency department with right progressive proptosis, retro-ocular and headache pain, reduced visual acuity, and epistaxis over the previous 4–6 weeks, with healthcare status deterioration in the previous 2 weeks. He denied fever, diplopia, ocular trauma or weight loss. He had a Gleason 6 prostatic tumour (diagnosed 2 months previously), glaucoma and ankylosing spondylitis (diagnosed 10 years previously) medicated with prednisolone and salazopyrin. There was no other personal or family history of thyroid or malignant diseases. The ophthalmologic examination revealed conjunctival exudate and hyperaemia (without cellulitis), and exuberant proptosis with inferior and temporal dystonia and overdraft limitation. Visual acuity of the right eye was 2/10. Biomicroscopy revealed right ocular nummular keratitis with a normal anterior chamber and left ocular aphakia. The ocular fundus did not show optic nerve compression, macular alterations or papilloedema. Bilateral intraocular tension was normal. The patient had no fever; however, he was hypotensive, tachycardic, with active epistaxis and scattered ecchymosis. He had no palpable thyroid and the thoracic and abdominal examinations were normal, without adenopathies.
Methods and Procedures
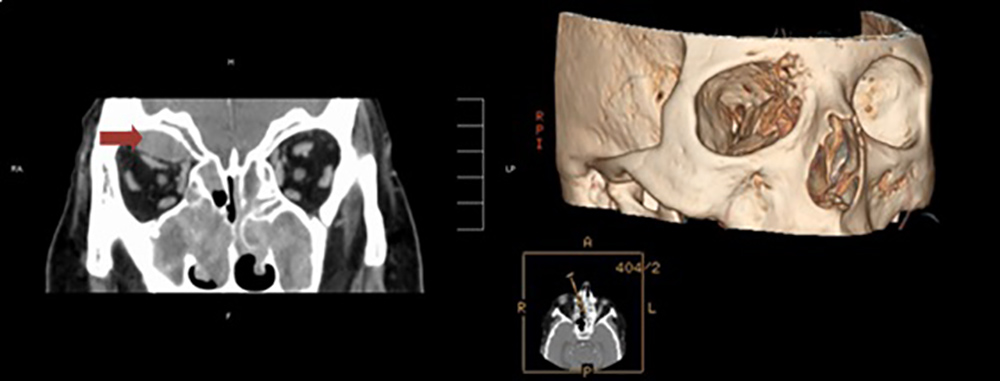
After multidisciplinary discussion and orbital computerized tomography (CT) suspicion of sinusitis with periorbital abscess, broad-spectrum antimicrobial and liposomal amphotericin B therapy was initiated and the patient was admitted to the intensive care unit. Orbital CT (Fig. 1) revealed an extraconic, with a peripheral cotton wool-like appearance, retro-orbital and superomedial tumour (2.2 cm), with frontal and ethmoidal bone (right orbital lamina) destruction, mass effect on the superior rectus muscle, exuberant filling of the ethmoidal sinus, reactive osteitis and nasal polyposis, without intracranial invasion.
Figure 1. The arrow shows the posterior orbital tumour (superior and medial in the orbit), with mass effect on the superior rectus muscle. 3D reconstruction reveals frontal and orbital lamina destruction
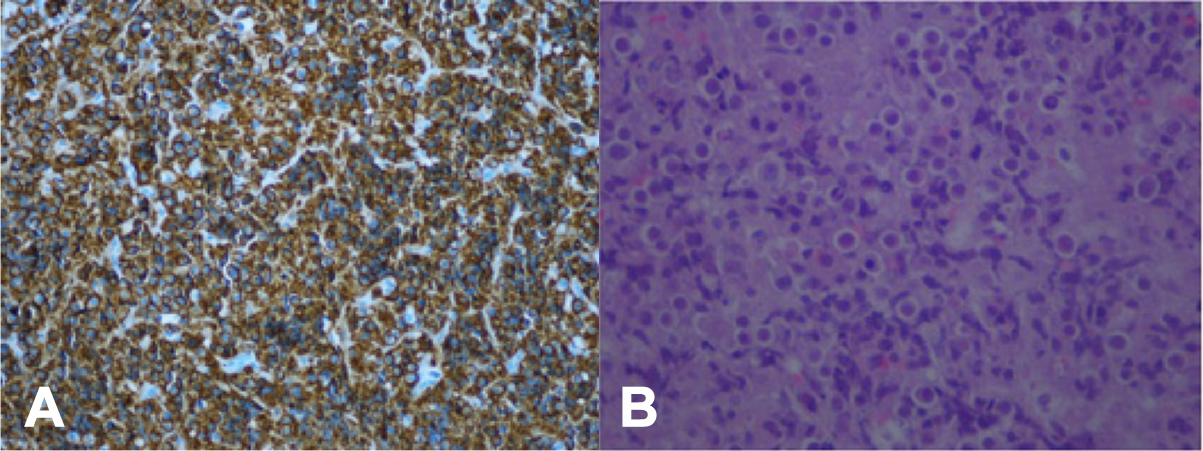
Blood tests disclosed severe normocytic, normochromic anaemia (the lowest value was 4.0 g/dl), severe thrombocytopenia (the lowest value was 21 G/l), increased aPTT and PT (prothrombin 27%), acute kidney injury (KDIGO stage 2) with metabolic acidosis and hyperkalaemia (6.5 mmol/l), reduced albumin (2.7 g/dl), elevated C-RP (15 mg/dl, normal <0.5), LDH (1,631 U/l, reference 125–220) and uric acid (13.3 mg/dl, reference 3.5–7.2). Calcium and the ESR were normal. Blood flow cytometry with immunophenotyping showed 9.4% of plasma cells with intracytoplasmic clonal κ chains. Immunoglobulin (Ig) G and λ chains were decreased with a normal κ/λ ratio, IgM and IgA. β2-microglobulin was increased: 13.8 mg/l (1.09–2.53). Plasma and urine immunofixation was normal. Blood, urine and respiratory cultures were negative. Supraciliary orbitotomy with biopsy of the tumour (Fig. 2) was performed, revealing a friable subperiosteum tumour with invasion of the frontal sinus; histological examination unveiled CD138+ plasma cells, consistent with plasmacytoma.
Figure 2. Orbital tumour biopsy: (A) CD138+ mature plasma cells: 10 × 20, with (B) pronounced pleomorphism, H&E: 10 × 40. Image provided by Maria José Julião (PhD)
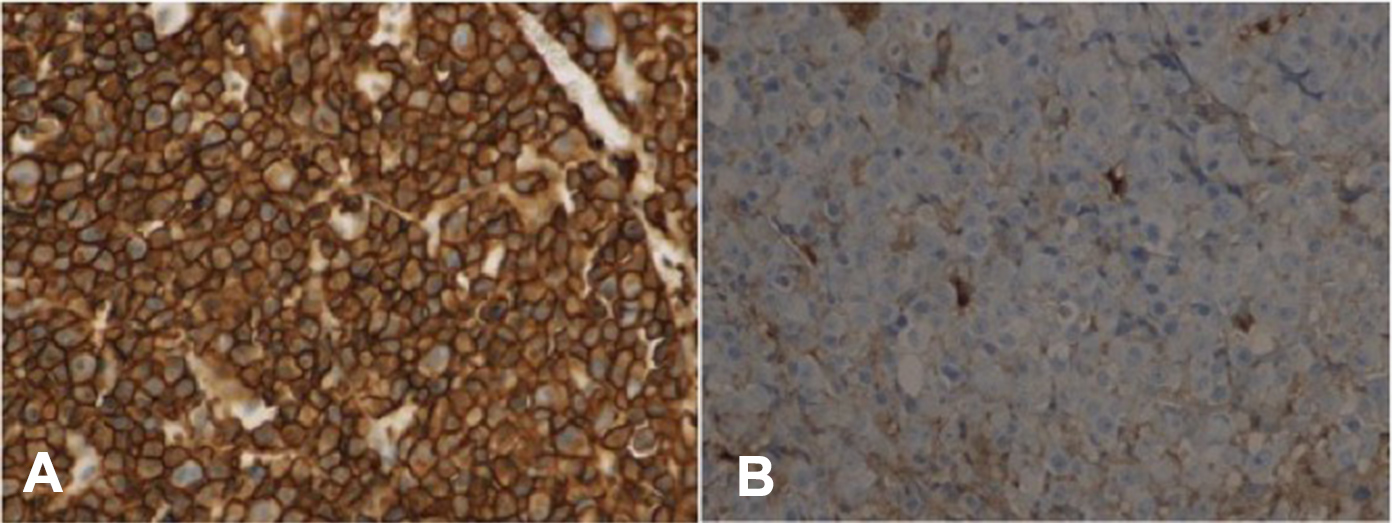
Bone biopsy (Fig. 3) confirmed multiple myeloma (MM) with extensive fibrosis, residual haematopoiesis and κ light chain focal expression.
Figure 3. Bone marrow biopsy: multiple myeloma – (A) MUM-1 cells, CD3, CD20 and cytokeratins were negative. Extensive fibrosis with residual haematopoiesis and (B) κ light chain focal expression (λ light chain negative): 10 × 40. Image provided by Raquel Seiça (PhD)
Due to the patient’s status, therapy with dexamethasone and cyclophosphamide was proposed but he was deceased a few days after admission.
DISCUSSION
MM represents 10% of all haematologic malignant neoplasms, with peak incidence between the fifth and eighth decades of life, without sex preference[2]. In the report from Varettoni et al. looking at 1,003 cases[1], extramedullary disease occurred in 13% of cases, and 7% (approximately half) presented with plasmacytoma at the time of diagnosis, mostly in the axial region. When considering head locations only, 80% occurred in the upper respiratory tract and oral cavity. Orbital involvement is uncommon and in more than half of cases it is only discovered after MM diagnosis[2].
Moreover, in a review of 2,480 cases[3], most orbital tumours were benign; 317 (13%) were lymphoproliferative lesions but only 1% of them were plasmacytomas. These authors even presented a patient with an atypical plasmacytoma location, without previous haematologic neoplasm, which initially simulated sinusitis with subperiosteum abscess.
Proptosis is the most common (81%) symptom[1], with ptosis, reduced visual acuity, oedema and diplopia also being frequently reported[2]. However, ocular pain is rarely described.
Most orbital tumours are superior and laterally located, 90% extraconic. The tumour medial extension and knowledge that most cases report bone destruction[3] explains the patient’s epistaxis.
This case presented decreased immunoglobulins and normal plasma and urine immunofixation, reported in less than 15% of cases, although most MM cases demonstrate hypergammaglobulinaemia, mostly IgG[2]/sup>.
The authors report a rare case of an inaugural MM that presented as an atypical orbital plasmacytoma, the uncommon topography, symptom particularities and monoclonality absence of which led to a challenging diagnosis of an advanced and fatal malignant tumour: MM.