ABSTRACT
Varicella infection is caused by varicella-zoster virus (VZV) and commonly presents as a self-limiting skin manifestation in children. VZV also causes cerebral arterial vasculopathy and antibody-mediated hypercoagulable states leading to thrombotic complications in children, although there are very few such reports in adults. Postulated causal factors include vasculitis, direct endothelial damage, or acquired protein S deficiency secondary to molecular mimicry. These induced autoantibodies to protein S could lead to acquired protein S deficiency and produce a hypercoagulable state causing venous sinus thrombosis. Here we report the case of a 26-year-old man who presented with cortical venous sinus thrombosis and acute pulmonary embolism following varicella infection. Both conditions responded to anticoagulation treatment.
LEARNING POINTS
- Varicella infection caused by varicella-zoster virus (VZV) can rarely present with thrombotic complications after a period of latency.
- Postulated causal factors include vasculitis, direct endothelial damage, and acquired protein S deficiency secondary to molecular mimicry.
- The prognosis of post-varicella thrombosis is good, but a prothrombotic screen after recovery to diagnose hereditary prothrombotic states is advisable.
KEYWORDS
Venous thrombosis, pulmonary embolism, varicella infection, protein S deficiency, hypercoagulable state
INTRODUCTION
Varicella infection is caused by varicella-zoster virus (VZV) and commonly presents as a self-limiting skin manifestation in children. VZV is known to cause antibody-mediated hypercoagulable states leading to thrombotic complications in children[1]. Such complications are very rare in adults but there are a few isolated case reports of thrombosis of either the cortical venous sinus or deep veins of the lower limbs in adults[2,3]. The exact mechanism of the pathogenesis of venous thrombosis following varicella is not known, but postulated causal factors include vasculitis, direct endothelial damage, and acquired protein S deficiency secondary to the development of antibodies to protein S[4]. These induced autoantibodies to protein S could lead to acquired protein S deficiency and produce a hypercoagulable state causing venous sinus thrombosis. We report the case of a young patient who presented with cortical venous sinus thrombosis, intracerebral haemorrhage and acute pulmonary embolism following varicella infection. Early diagnosis and management helped to prevent associated morbidity and mortality.
CASE DESCRIPTION
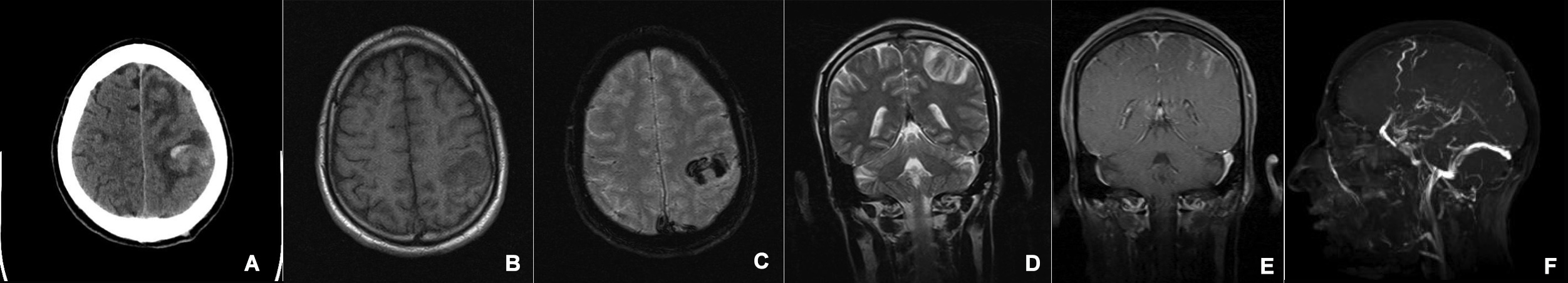
A 26-year-old Indian man presented with a history of seizures for the last 2 days and weakness of the left side of the body. He had history of chicken pox 2 weeks previously for which he had received oral acyclovir. He had no history of ear discharge, drug addiction, seizures, illness or surgical procedures. On examination, he was tachypnoeic, febrile (39.2°C) and had crusted chicken pox lesions all over his body. He was drowsy, but fully conscious with a GCS score of 5/15 with no cranial nerve deficits. Motor examination revealed right hemiparesis (power of 4/5 on the MRC scale), with a right plantar extensor response. The sensory system was normal and there were no meningeal signs. On examination, the patient had healed varicella scars. CSF analysis, complete blood counts, a renal function test, a liver function test, blood sugar, serum electrolytes, prothrombin time and activated partial thromboplastin time were normal. CT and MRI of the brain revealed multiple areas of haemorrhage with perilesional oedema involving the bilateral parietal and left frontal region (Fig. 1a–d). Post-contrast coronal T1WI showed a filling defect in the superior sagittal sinus suggesting sinus thrombosis, and mild gyriform enhancement in the region of haematoma (Fig. 1e). 2D Time of flight (TOF) magnetic resonance venography (MRV) of the brain confirmed thrombosis in the superior sagittal vein extending into the left transverse sinus (Fig. 1f).
Figure 1. CT and MRI images showing superior sagittal venous sinus thrombosis with left fronto-parietal haematoma. (a) Axial plain CT image shows acute-subacute parenchymal haematoma in the left high fronto-parietal region with surrounding white matter oedema. (b) Axial plain T1WI shows an iso- to hypointense lesion in the left high fronto-parietal white matter. (c) Axial GRE image shows profound hypointensity in the left high fronto-parietal white matter indicating haematoma. (d) Coronal T2WI shows a left fronto-parietal haematoma with surrounding oedema. The superior sagittal sinus shows an isointense signal raising concern for thrombosis. (e) Post-contrast coronal T1WI shows a filling defect in the superior sagittal sinus confirming sinus thrombosis. Mild gyriform enhancement is seen in the region of the haematoma. (f) MIP image from 2D TOF MR venography confirms thrombosis of the superior sagittal sinus.
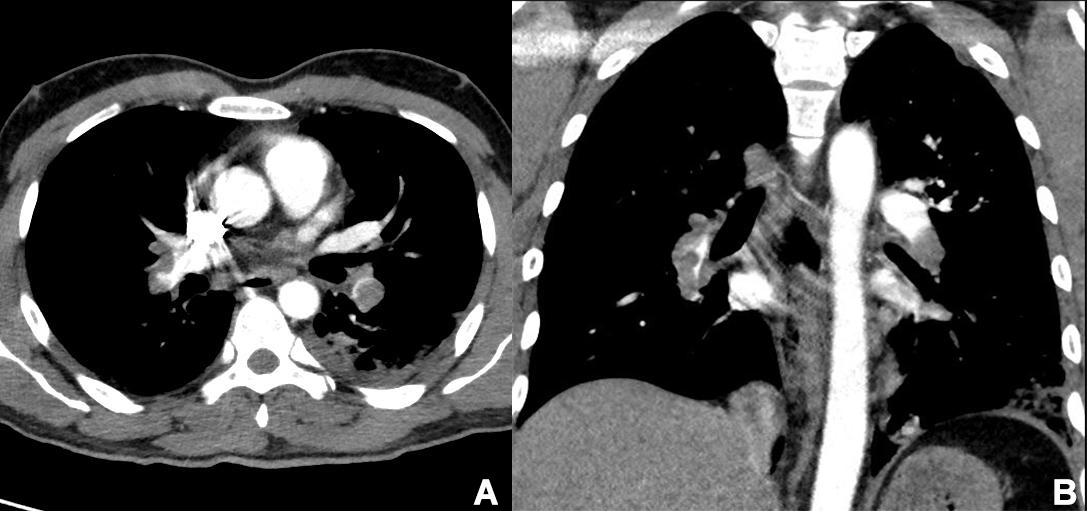
The patient was positive for varicella IgM antibodies, suggesting the diagnosis of varicella infection. He was started on oral anticoagulation with apixaban. However, after 2 days he developed haemoptysis, following which he developed progressive shortness of breath with systemic oxygen desaturation. ECG showed sinus tachycardia and D-dimer was markedly elevated to 23.2 mg/l (normal <0.3 mg/l). The patient underwent urgent CT pulmonary angiography (CTPA) which showed bilateral extensive pulmonary emboli with evidence of right ventricular strain (Fig. 2a,b).
He was started on low-molecular-weight heparin at a therapeutic dose. Oxygen saturation gradually improved over 5 days, and echocardiography showed resolution of the right ventricular strain and normalisation of right ventricle cavity size and pulmonary artery pressures. He continued to take enoxaparin 1 mg/kg twice daily until he improved, and was discharged on oral anticoagulation with apixaban, anticonvulsants and oral anticoagulants (NOAC). Lower limb venous Doppler ultrasonography was negative. A prothrombotic screen (protein S, protein C levels, factor V Leiden mutation, anti-thrombin III levels and anti-cardiolipin antibodies) was planned but not performed as the patient did not return for follow-up.
Figure 2. CT pulmonary angiography images showing bilateral extensive pulmonary emboli. (a) Axial CT pulmonary angiography (CTPA) image shows emboli in bilateral inferior lobar pulmonary arteries. (b) Coronal CTPA showing similar findings
DISCUSSION
The incidence of serious complications after varicella infection is 8.5/100,000 population[5]. Thrombotic complications have been reported after a latency period of 2 weeks in patients with varicella infection. Post-viral thromboembolism resulting in cerebral venous thrombosis, deep vein thrombosis or pulmonary embolism is a rare presentation even in children. Only a few isolated cases of thrombosis of either the cortical venous sinus or deep veins of the lower limbs have been reported in adults. Paul et al.[6] reported three cases in adults presenting with extensive thrombosis simultaneously involving the cortical venous sinus, deep veins of the leg and atrial thrombus with pulmonary embolism following varicella infection.
Siddiqi and colleagues[7] described two cases of cerebral venous sinus thrombosis associated with varicella-zoster. Protein C and S levels were deficient. MRA and MRV revealed filling defects in the superior sagittal, straight, bilateral transverse and sigmoid sinuses, extending into both jugular veins. The patient improved with intravenous acyclovir, adequate hydration and oral levetiracetam.
Eidelberg et al.[8] suggested virus-mediated endothelial injury promoted local thrombosis, but transient deficiency of protein S activity due to induction of anti-protein S autoantibodies has also been suggested as a causal factor. The frequency with which antibodies to proteins S are induced is unknown. Thrombosis is more common in individuals with the factor V Leiden mutation which increases the risk for thrombosis as it confers resistance to activated protein C.
That varicella causes neurological manifestations is evidenced by the temporal association between the development of skin lesions and thrombotic complications. The latency period of 2–3 weeks signifies the time during which direct venous endothelium damage occurs or autoantibodies to natural anticoagulants develop leading to a widespread thrombotic process. VZV has been shown to replicate in cerebral arteries. It travels transaxonally to the adventitia of arteries, followed by transmural migration to the arterial media and intima and pathological vascular remodelling[9]. The prognosis in patients with post-varicella thrombosis is good. However, a prothrombotic screen after recovery to diagnose hereditary prothrombotic states that need lifelong anticoagulants is advisable.