ABSTRACT
Systemic lupus erythematosus (SLE) is a chronic multi-systemic immune-mediated disease with confusing symptoms and delayed diagnosis. We report the case of a 32-year-old man with a persistent Venereal Disease Research Laboratory (VDRL)-positive reaction treated for syphilis 5 years previously, who was admitted for rash, weight loss, pancytopenia, inflammatory syndrome, and an important spontaneous prolongation of activated partial thromboplastin time (aPTT). Antiphospholipid antibodies were identified in the patient and he was diagnosed with SLE. The unrecognized false positive VDRL reaction and the delayed diagnosis of SLE were harmful as the patient had developed renal and cardiac complications by the time of diagnosis.
LEARNING POINTS
- VDRL positive reaction as a diagnostic tool for syphilis must be confirmed by other tests like TPHA and Western Blot reaction, especially in the absence of a clinical context, taking into account the possibility of false positive results.
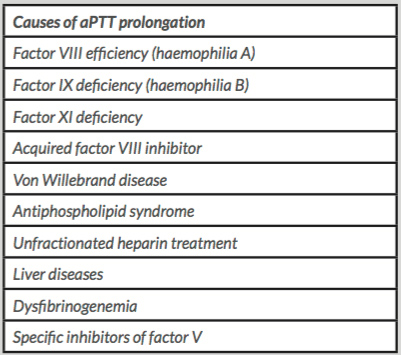
- Spontaneous prolongation of aPTT can be related to the presence of antiphospholipid antibodies.
- In medical practice, the clinician must always consider the uniqueness of a diagnosis that integrates all the clinical and laboratory data, even if the associations might seem confusing.
KEYWORDS
Systemic lupus erythematous, antiphospholipid antibodies, aPTT
CASE DESCRIPTION
A 32-year-old man was admitted for involuntary weight loss (9 kg in 3 months), a maculopapular rash on the feet, face and anterior thorax, and morning joint stiffness. He was a non-smoker. He had a history of (a) Venereal Disease Research Laboratory (VDRL) elevation, interpreted as Treponema pallidum infection and treated with penicillin 5 years previously, (b) moderate normocytic, normochromic anaemia diagnosed 6 months before admission and interpreted as a result of vitamin deficiency, and (c) inflammatory syndrome interpreted as a result of pneumonia treated with ciprofloxacin 2 months prior to admission.
The physical examination showed low-grade fever (37.5–38.0°C), skin pallor and a non-pruriginous cutaneous maculopapular rash on the thorax (Fig. 1) and fingertips (Fig. 2). There were no cardiovascular, respiratory or digestive pathological changes.
Figure 1. Macular erythematous cutaneous lesions on the thorax
Figure 2. Papular erythematous rash on the fingertip
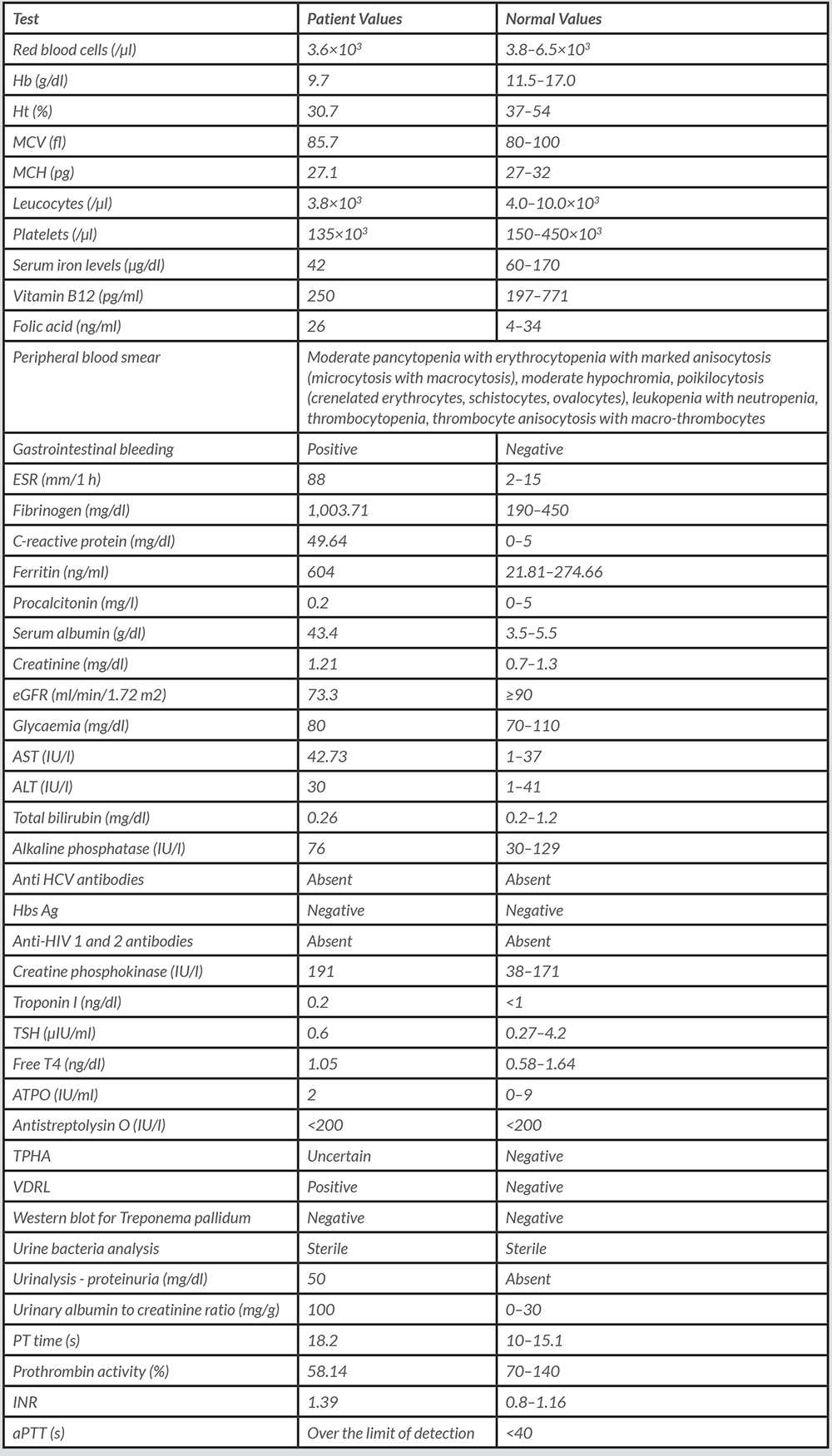
Laboratory tests revealed pancytopenia, low blood iron, high erythrocyte sedimentation rate (ESR) and C-reactive protein levels, a mildly reduced estimated glomerular filtration rate, a urinary albumin/creatinine ratio of 100 mg/g, mildly increased creatine phosphokinase and aspartate aminotransferase, and occult gastrointestinal bleeding. We noted a positive VDRL test, an uncertain Treponema pallidum haemagglutination assay (TPHA), and a negative protein immunoblot reaction (Western blot test) for Treponema pallidum. Coagulation tests showed spontaneous important prolongation of the activated partial thromboplastin time (aPTT) (Table 1). The patient had no familial or personal history of coagulation disorders, did not receive anticoagulants and had no liver disease. We tested the patient for antiphospholipid (AFL) antibodies and found lupus anticoagulant (LA) positive in the ratio 3.49, anticardiolipin Ig G antibodies (aCL) over 280 GPL and beta-2 glycoprotein IgG antibodies (aβ2-GPI) positive. Although AFL antibodies may be present without an identifiable cause, they are usually secondary to a primary disease. The patient’s medical history and clinical picture raised the suspicion of systemic lupus erythematosus (SLE). Double-stranded DNA (dsDNA) antibodies were positive (178 IU/ml) (Table 1).
Thoracic radiography, abdominal ultrasound examination and upper gastrointestinal endoscopy were normal, while colonoscopy revealed bleeding haemorrhoids.
We concluded the patient had SLE as he met several ACR EULAR 2018 criteria: musculoskeletal involvement, leukopenia, thrombocytopenia, renal involvement, positive AFL, and positive dsDNA antibodies.
During hospitalization, the patient developed thoracic pain, and increased NT-proBNP and troponin serum levels. A cardiac MRI was performed and showed a pattern of lupus myocarditis.
After a 3-month regimen of daily 32 mg methylprednisolone and 200 mg hydroxychloroquine, the patient’s coagulation tests and blood count normalized, proteinuria disappeared, and NT-proBNP levels normalized.
DISCUSSION
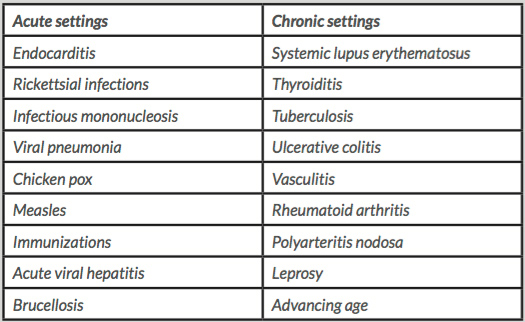
The case of a young man with a long-standing history of a positive VDRL reaction, recent cutaneous rash and low-grade fever raises many problems of differential diagnosis. The first supposed diagnosis is secondary syphilis, but there could be other causes of false VDRL positivity including acute infectious diseases (Table 2) [1,2]. The clinical picture in our patient did not match such a diagnosis. VDRL is a non-treponemal test for syphilis screening and the diagnosis must be confirmed by treponemal tests such as TPHA. However, the TPHA reaction can be uncertain in infectious mononucleosis and false positive in SLE[1]. The next confirmation tests are Western blotting or polymerase chain reaction[1]. In our case, the result of TPHA was uncertain but a Western blot test for Treponema pallidum was negative, excluding the diagnosis of syphilis. The association of a false VDRL and TPHA positivity, rash, fever, inflammation, pancytopenia and renal involvement are frequently found in SLE, particularly in women. This diagnosis was also supported by the confirmation of antiphospholipid syndrome suggested by the spontaneous very high prolongation of aPTT. There are other causes of high aPTT (Table 3) but the patient had none of them. Some 20–40% of patients with SLE have APL antibodies (aCL, anti-β2-GPI, LA). Half of them also have a positive VDRL test as had our patient. There is a high risk of (often recurrent) deep vein thrombosis, arterial thrombosis and pulmonary embolism, especially in patients with positive LA compared to those with aCL antibodies. In the study by Pengo et al. in 27 patients with SLE, the association of LA, aCL and anti-β2-GPI was an independent risk factor for thrombotic events[3].
Table 1. Laboratory test results
ALT, alanine transaminase; AST, aspartate transaminase; aPTT, activated partial thromboplastin time; ATPO, anti-thyroid peroxidase antibodies; eGFR, estimated glomerular filtration rate; ESR, erythrocyte sedimentation rate; free T4, free thyroxine; Hb, haemoglobin; Ht, haematocrit; INR, International Normalized Ratio; MCH, mean corpuscular haemoglobin; MCV, mean corpuscular volume; MPV, mean platelet volume; RDW, red cell distribution width; TPHA, Treponema pallidum haemagglutination assay; TSH, thyroid-stimulating hormone; VDRL, Venereal Disease Research Laboratory.
According to the Sapporo criteria, antiphospholipid syndrome also includes the presence of thrombosis. If there is no thrombosis, the patient is an antiphospholipid antibody carrier but has a higher risk of thrombosis in the future[4].
Our patient subsequently developed myocarditis. This occurs less frequently than pericarditis or coronary arteritis in association with SLE. The clinical prevalence of lupus myocarditis is 9%, but post-mortem examinations have shown that it is present in 57% of cases. The myocardial involvement in SLE is often difficult to interpret by endomyocardial biopsy due to myocardial focal involvement[5]. In our patient, the diagnosis was suggested by the clinical data, elevation of troponin and NT-proBNP, and cardiac MRI findings. The cardiac involvement was successfully treated with SLE medication and supportive treatment for heart failure.
CONCLUSION
Multi-systemic long-term symptoms must be integrated into a unique diagnosis. A positive non-treponemal VDRL test suggesting the diagnosis of syphilis must be confirmed by other treponemal tests, especially in the absence of a clinical context. In our patient, TPHA was uncertain but Western blot testing for syphilis was negative. The spontaneous high elevation of aPTT in a young patient with various long-standing symptoms raised the suspicion of antiphospholipid syndrome in the setting of SLE. In our patient, the long-standing disease explained the existing renal and myocardial complications at the time of SLE diagnosis.