ABSTRACT
Cystic lymphangioma mainly occurs in children and develops from the lymphatic vessels. The present study reports the case of a 36-year-old female patient with a giant cystic mediastinal lymphangioma. She was asymptomatic and the diagnosis was accidental. Imaging studies are important for referral to the Cardio-Thoracic Surgery Department for surgical intervention in order to remove the lesion. It is important that in the case of an enlargement of the mediastinum observed in a thoracic X-ray, the possible diagnosis takes into consideration various hypotheses. Early diagnosis may prevent further growth and infiltration of structures that hinder the surgical approach.
LEARNING POINTS
- Cystic lymphangioma corresponds to approximately 0.7 to 4% of all mediastinal tumours.
- They are usually asymptomatic and, in adults, the diagnosis is accidental.
- After an imaging study with computed tomography and nuclear magnetic resonance, patients are usually candidates for surgical excision.
KEYWORDS
Cystic lymphangioma, mediastinal tumour, surgical approach
INTRODUCTION
Cystic lymphangioma, also known as cystic hygroma, is a congenital malformation originating from lymphatic hyperplasia and is one of several mediastinal pathologies, corresponding to approximately 0.7 to 4% of all mediastinal tumours[1]. Its incidence is rare and the majority of lymphangiomas are observed in patients under the age of 5, with extremely few cases being reported in adulthood[1–3]. The differential diagnosis is made with all mediastinal cystic structures, mainly teratomas, thymic cysts, pericardial and pulmonary cysts[1,2,4,5].
They are usually asymptomatic and, in adults, the diagnosis is
accidental. In children, the compressive symptoms are more frequent due to the lower available space, with frequent alterations of the cervical anatomy[1]. When present, the most common symptoms are dyspnoea, respiratory insufficiency, hoarseness and superior vena cava syndrome[2]. In most situations, the diagnosis is made from an enlargement of the mediastinum detected on a chest X-ray performed routinely[1,2].
CASE DESCRIPTION
A 68-year-old Caucasian male was asymptomatic until two weeks before admission to the emergency department, when he developed nausea and vomiting, which persisted despite antiemetic medication. Other than a diagnosis of right-sided herpes zoster ophthalmicus (HZO), four months before admission, and type 2 diabetes, his past medical history was unremarkable. General examination on admission was normal but neurological examination revealed right ptosis, divergent strabismus and anisocoria.
Blood tests revealed normocytic normochromia anaemia with Hb 10.2, VGM 86 fl, leucocytes 5,100×109/l, thrombocytopenia with a platelet count of 91,000×109/l and a C-reactive protein level of 61.5 mg/l (normal <3 mg/l). A CT scan of the brain to rule out stroke surprisingly showed three round lesions, slightly hyperdense, with intra-axial and periventricular location (Fig.1).
Cerebrospinal fluid collected by lumbar puncture was acellular with normal protein and glucose levels, ruling out a CNS infection. Autoimmune study and serological tests, including tests for human immunodeficiency virus (HIV), hepatitis virus, syphilis and Epstein-Barr virus, were negative.
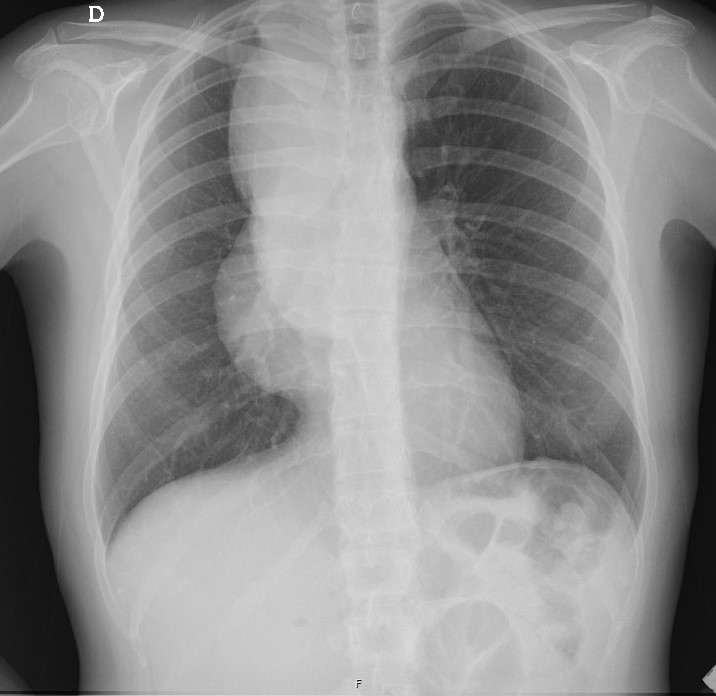
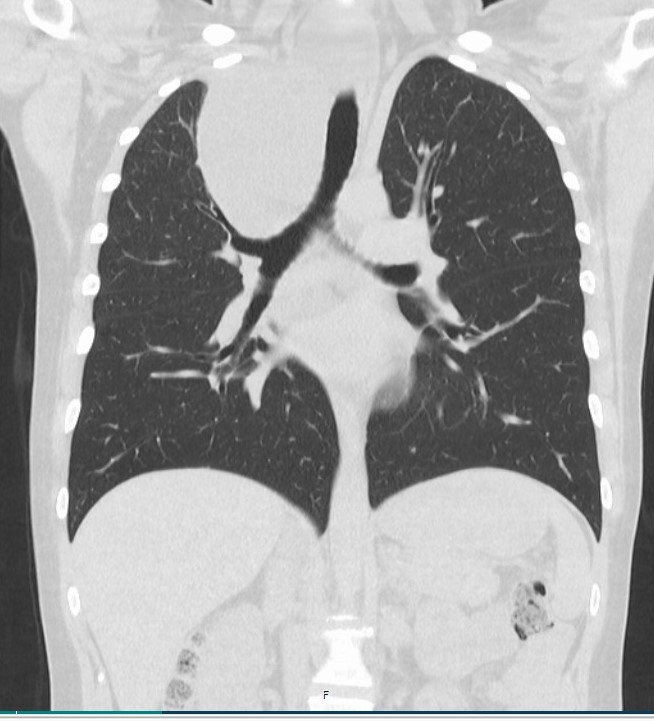
A computed tomography scan was requested to exclude a vascular cause, with a voluminous formation of liquid content in the mediastinum and the subcarinal region being evident, possibly revealing a pleuropericardial cyst/cystic lymphangioma (Figs. 2 and 3).
Figure 2. Thoracic CT scan with a voluminous formation of liquid in the mediastinum and the subcarinal region
Figure 3. Thoracic CT scan with a voluminous formation of liquid in the mediastinum and the subcarinal region
The patient was admitted to the Internal Medicine Department for complementary studies, having performed respiratory function tests with CO2 diffusion and plethysmography that revealed a normal respiratory function. A chest MRI scan was requested that confirmed an extensive lobulated, multilocular, cystic lesion centered on the right side of the mediastinum and mediastinal pleura, approximately 200 mm long, 130 mm large from side to side and 140 mm in the anteroposterior dimension. The lesion conditioned the deviation of the vascular structures and the mediastinum, without invasion criteria, suggesting a diagnosis of thoracic cystic lymphangioma, with cervical extension. The patient was referred to the Cardio-Thoracic Surgery Department for surgical intervention in order to remove the lesion.
DISCUSSION
Cystic mediastinal lymphangioma (CML) is an extremely rare vascular tumour originating from the lymphatic vessels. In total, 90% are discovered in individuals under 2 years of age[6]. After an imaging study with computed tomography and nuclear magnetic resonance, patients are usually candidates for surgical excision. The growth and infiltration of mediastinal structures make surgery difficult. Although other treatment methods, such as sclerotherapy and radiotherapy, have been reported in unresectable cases, they are generally ineffective and may result in haemorrhage and infection[7]. Therefore, surgery remains the superior method for treatment with curative intent. Complete surgical resection remains the treatment of choice for lymphangioma in order to eliminate symptoms and prevent recurrences[8]. Thus, it is important to study mediastinal enlargement seen in X-rays, considering the various hypotheses of possible diagnosis, and to investigate with complementary examinations, even when there is no associated symptomatology. Early diagnosis may prevent further growth and infiltration of structures that hinder the surgical approach. In summary, CML, particularly giant CML, is extremely rare in adults. Complete surgical resection provides a definitive histological diagnosis and prevents recurrence.