ABSTRACT
A woman in her early 40s, with a history of excessive alcohol intake, presented with purpuric, ulcerative lesions on the lower limbs. On examination, hirsutism and generalized stiffening and thickening of the skin were noted. Laboratory investigations revealed hyperbilirubinemia, hypergammaglobulinemia and positive anti-smooth muscle antibodies. Histologic examination of the skin was compatible with scleroderma. Histologic examination of the liver was suggestive of autoimmune and alcoholic hepatitis.
LEARNING POINTS
- Alcohol intake is a main cause of hepatic disease but it is mandatory to exclude other causes.
- Autoimmune hepatitis and systemic sclerosis may be associated, therefore patients with these diseases should be monitored closely.
- There exist scores that can be helpful in the diagnosis of both autoimmune hepatitis and systemic sclerosis.
KEYWORDS
Autoimmune hepatitis, systemic sclerosis, alcoholic hepatitis
CASE DESCRIPTION
A woman in her early 40s presented with purpuric, ulcerative lesions on the lower limbs. These started as papules, which then became blisters and turned to ulcers within 4 days. She also complained of 15 days of dry cough and a couple of months of abdominal swelling.
She reported an excessive alcohol intake (at least 45g/day). Her family history was notable for systemic lupus erythematous (in a sister, who died in her 20s).
On examination, we noted the ulcerative lesions on the lower limbs, with serous drainage and pronounced inflammatory signs (Fig. 1). She also presented evident stiffening and increased thickness of the skin, associated with hirsutism and scattered telangiectasia. Raynaud’s phenomenon was also visible (Fig. 2). The patient also presented ascites, as well as symmetric lower limb edema. Thorax auscultation revealed a diminished murmur on both pulmonary bases. Her general examination was otherwise unremarkable.
Methods and procedures
Laboratory investigations showed hyperbilirubinemia (1.81 mg/dL) with increased direct bilirubin (0.57 mg/dL), elevated alkaline phosphatase (AF) (157 U/L) and gamma-glutamyltransferase (GGT) (219 U/L), with normal transaminases. Other findings were elevated lactic dehydrogenase (273 U/L),hypoalbuminemia (3.3 g/dL), and raised C-reactive protein (11 g/dL). Other biochemical and hematologic evaluations were normal.
Serologic evaluation revealed hypergammaglobulinemia (1790 mg/dL) and positive (1/40) anti-smooth muscle (SM) antibodies. Other serologic markers, namely antinuclear and anti-double strand-DNA antibodies, were negative. Viral and metabolic causes of hepatic disease were also excluded.
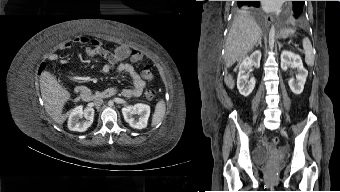
Computerized tomography scan showed chronic liver disease, thickening of lipomatous tissue, as well as ascites; marked edema of subcutaneous tissue and thickened skin were also paramount features (Fig. 3).
Histologic examination of the skin was compatible with scleroderma.
Figure 1. Ulcerative lesions on the lower limbs, with serous drainage and prominent inflammatory signs
Figure 2. Raynaud’s phenomenon
Figure 3. Computerized tomography images (sagittal and horizontal). Marked edema of subcutaneous tissue and thickened skin
Histologic examination of the liver revealed cirrhosis, Mallory bodies as well as inflammatory lymphoplasmacytic infiltrate in portal spaces with interface hepatitis. These features were suggestive of alcoholic hepatitis and autoimmune hepatitis (AIH).
In-hospital treatment, with antibiotics and diuretics, led to full recovery of the lower limb lesions and major improvement of the edema.
After discharge, the patient was referred for both autoimmune and gastroenterology consultations. At these appointments, she was asymptomatic, with no further lesions. Laboratory tests still revealed slight increases in total bilirubin (1,41 mg/dL), AF (164 U/L) and GGT (185 U/L) levels, and even more pronounced hypergammaglobulinemia (2150 mg/dL).
She underwent several examinations to assess organ involvement related to systemic sclerosis (SS). Spirometry showed a mixed ventilatory syndrome with a severe obstructive component. Cardiac assessment revealed non-ischemic dilated myocardiopathy with severe biventricular systolic dysfunction. Pulmonary hypertension was also documented (estimated pulmonary systolic blood pressure of 50mmHg). Endoscopic investigation demonstrated atrophic gastritis, with no further alterations. X-rays of the hands and feet showed no signs of calcinosis.
DISCUSSION
AIH is frequently associated with other immune diseases[1,2]. However, reports of cases of AIH related to SS are few in number, most of them describing patients with a previous diagnosis of limited SS[3,4].
In this report, we describe a patient with a simultaneous diagnosis of AIH and diffuse SS.
AIH is an inflammatory chronic liver disease of unknown cause. It has prominent extrahepatic features of autoimmunity, such as the presence of autoantibodies and hypergammaglobulinemia. Its histological hallmark is interface hepatitis[5]. AIH is associated with a wide range of other autoimmune diseases, like diabetes mellitus type 1, thyroiditis, autoimmune haemolytic anemia and autoimmune thrombocytopenia[1,2]. Systemic connective tissue diseases, such as SS, have occasionally been reported in association with AIH[3]. In most of these cases, SS has a limited organ involvement and, with only a few exceptions, AIH occurs after the diagnosis of SS[3,4,7].
SS is a chronic fibrotic immune-mediated systemic disease that targets the skin, lungs, heart, gastrointestinal tract, kidneys and musculoskeletal system[8]. Although most patients with SS have gastrointestinal involvement, liver disease is reported only rarely, most frequently consisting of primary biliary cirrhosis[9].
The pathological mechanisms underlying the development of AIH and SS remain unclear, which raises the question of whether the association has a causal basis or occurs by chance. However, the activation of a humoral and cellular immune response, seen in both diseases, may be a common mechanism[3].
High suspicion indexes were needed in order to make both diagnoses. The stiffness and thickening of the skin, as well as the presence of Raynaud’s phenomenon, were important features supporting the diagnosis of SS. The ulcerative lesions were probably related to microvascular phenomena due to SS.
There were several clues indicating the presence of liver disease, namely the ascites, hirsutism and peripheral edema, together with the laboratory findings. Alcohol intake was a confounding factor that could not be eliminated; however, liver biopsy was compatible with chronic hepatitis due to both alcohol and AIH.
There exist scores that are useful for diagnosing both these conditions. The simplified diagnostic criteria for AIH by Hennes et al.[10] offer a data-driven, consensus-based pathway to help guide treatment; this is likely better than relying on clinical judgment alone. Our patient’s score, using these criteria, was 7 points (anti-SM antibodies, hypergammaglobulinemia, typical liver histology and absence of viral agents), corresponding to a definitive diagnosis of AIH. The American College of Rheumatology and the European League Against Rheumatism (ACR/EULAR) have provided criteria for the diagnosis of SS[8]; in this case, our patient scored 16 points, confirming the diagnosis of SS.
This patient had only partial indications for immunosuppressive treatment for AIH (hypergammaglobulinemia and interface hepatitis), so it was not initiated. As for SS, since there are no approved disease-modifying drugs, treatment is only symptomatic.
The prognosis of AIH depends on whether there is hepatic inflammation and progression to cirrhosis, and on the complications that arise. Without treatment, about half of affected patients die within 10 years; however, the survival rate of patients achieving clinical remission is comparable to that of the general population[5]. The prognosis of SS depends mostly on the organic involvement; the condition has an overall survival rate of 80% at 5 years[8]. The prognosis of the association, AIH and SS, is unknown.
In conclusion, AIH may be considered a liver manifestation of diffuse SS. Patients with these conditions should be monitored closely because they are at increased risk of developing other associated diseases. Clinician awareness is of major importance, contributing to an early diagnosis and effective treatment.