ABSTRACT
Heat stroke (HS) is a life-threatening condition characterized by hyperthermia and multiple organ failure. Mild to moderate hepatocellular injury is a well-documented complication but severe liver injury and acute liver failure are rare. There are neither established criteria nor optimal timing for liver transplantation and conservative management seems to be the cornerstone treatment. The authors report a case of a patient with severe liver injury related to HS who recovered completely under conservative treatment.
LEARNING POINTS
- Hyperthermia, neurologic dysfunction and recent exposure to hot weather or physical exertion should raise the suspicion of heat stroke (HS).
- Fast and effective cooling is the cornerstone of treatment, along with support of organ dysfunction. Antipyretics have no role in HS management.
- Conservative treatment has been described as being successful in the management of patients with HS that manifest severe acute liver injury (ALI) and acute liver failure (ALF). However, early referral to a liver transplantation centre is essential to guide treatment.
KEYWORDS
Heat stroke, acute liver injury, liver transplantation
CASE DESCRIPTION
A 53-year-old man, with dyslipidaemia and an alcohol consumption of 100 g per day, presented a progressive unspecific malaise which culminated in a witnessed loss of consciousness after 6 hours of physical work at a temperature of 33ºC. He was locally assisted by an emergency response team and was found comatose and hypotensive. He was intubated, fluid challenge was initiated and he was admitted half an hour later to the emergency room. He remained hypotensive (mean arterial pressure <65 mmHg), tachycardic (sinus rhythm) and was sweaty with a tympanic temperature of 39.9ºC. Fluid challenge was maintained and therapeutic cooling with intravenous cold saline and through gastric tube infusion was immediately undertaken.
Initial workup revealed: metabolic acidosis with hyperlactacidaemia (lactate 5.9 mmol/l, normal (N) <2), acute kidney injury (creatinine 6.8 mg/dl, N 0.7–1.2), rhabdomyolysis (myoglobin 3,670 ng/ml, N <116), mild elevated total bilirubin (1.7 mg/dl, N <1.0) and mild elevated alanine aminotransferase (ALT 177 U/l, N <78). The complete blood count, coagulation, glucose, troponin, remaining liver panel, drug testing and alcohol dosage were normal. An electrocardiogram, echocardiogram and brain and chest-abdomen-pelvis computed tomography with angiography showed no alterations.
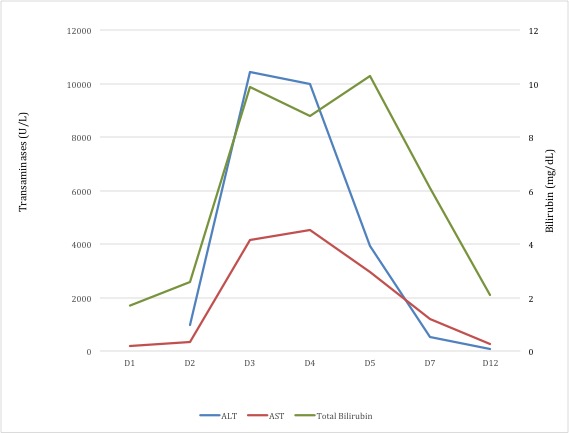
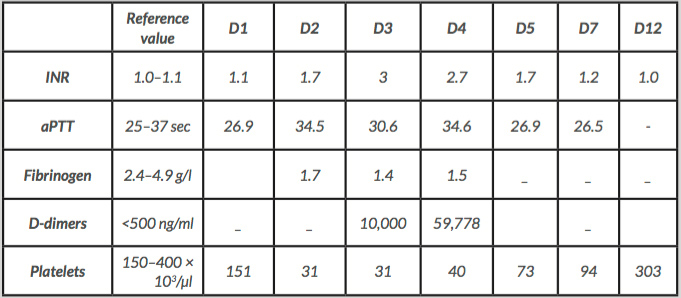
After 1 hour of cooling, the patient’s tympanic temperature was 37.9ºC. He was further monitored and supported in the Intensive Care Unit (ICU), with cold saline infusion and application of ice packs maintained. The maximal core temperature in the following 12 hours was 38.2ºC. Despite the improvement in cardiocirculatory, renal and neurological dysfunction allowing early extubation on the next day, there was worsening of the liver injury (Fig. 1), without signs of encephalopathy, and evolution to disseminated intravascular coagulation (DIC) (Table 1). Early referral and transfer to a Liver Transplant Unit was made at day 3 due to the possible progression to acute liver failure (ALF). In addition, other causes of liver disease were excluded: abdominal ultrasound with Doppler imaging , virus screening and general and hepatic-specific autoimmune, immunological and metabolic studies were normal. From the 5th day on, there was a progressive improvement of the liver panel and coagulation without specific treatment. The patient remained without encephalopathy and evolved without the need for hepatic clearance techniques or liver transplantation (LT).
Figure 1. Evolution of liver analysis until recovery
ALT: alanine aminotransferase; AST: aspartate aminotransferase; D1–D12: days.
Table 1. Evolution of coagulation tests until recovery
INR: international normalized ratio; aPTT: activated partial thromboplastin time; D1–D12: days.
DISCUSSION
Heat stroke (HS) is the most severe form of heat-induced illness and a potentially fatal condition that occurs when the body’s capacity to dissipate heat is overwhelmed by excessive heat production. It can result from exposure to high environmental temperatures (classic HS), affecting chronically ill patients or those who cannot care for themselves (for example, the elderly), or from strenuous physical activity, especially in hot environments (exertional HS), as presented in the clinical case here. The diagnosis is based on clinical history, the presence of hyperthermia (usually >40.5ºC) and central nervous system dysfunction[1–6]. A high index of suspicion is needed, as it can rapidly progress to multiple organ dysfunction. There are many predisposing factors to HS: underlying cardiovascular, cerebrovascular and pulmonary illnesses, medication (beta-blockers, diuretics, calcium channel blockers, laxatives, antidepressants), drug abuse (amphetamines, cocaine) and alcoholism[1]. In addition to strenuous activity performed under severe heat conditions, our patient’s alcoholism history could have increased the risk and raised the suspicion of HS.
Prompt cooling is the cornerstone of treatment and seems to be the most important prognostic measure[1–5]. The majority of authors defend a “golden half-hour in the realm of HS”, independent of the exact initial temperature of the patient[1,2]. Recently, Epstein and Yanovich proposed a target core temperature below 39ºC, with a cooling rate faster than 0.10°C per minute being safe for exertional HS[1]. Cooling measures include cold fluids (4°C, 1,000 ml/30 min)[1], cold water immersion and application of ice packs, cold packs or wet gauze sheets. Antipyretics are ineffective since hyperthermia and fever have different physiological pathways[1–3] and they can even aggravate coagulopathy and liver injury[1]. Core temperature monitoring and admission to the ICU is essential. In our case, survival may have been improved by effective cooling, with a peripheral temperature of less than 38ºC achieved in approximately 1 hour.
Hepatic injury is relatively common and reversible in exertional HS but severe ALI and ALF are rare, with a bad prognosis and may require LT[1,4–6]. It mainly occurs in athletes or soldiers undergoing extreme physical exertion[4]. The underlying physiological process is not fully understood but it may be related to multiple factors: direct thermal damage to the endothelium and hepatocytes and ischaemic hepatitis due to hypoperfusion (shunting of blood from the splanchnic circulation to the skin in order to dissipate heat) and microthrombosis[5,6]. Hepatocellular injury may be of late onset as seen in our patient who presented with non-suspicious liver chemistry on admission[5]. Patients with worsening coagulopathy or encephalopathy should be monitored in centres with expertise in LT. It is important to maintain a high index of suspicion for ALF as hepatic encephalopathy may become superimposed on HS-related neurologic dysfunction, with these being difficult to distinguish from each another, especially in patients requiring mechanical ventilation[5,6]. In these cases, determination of arterial ammonia levels or electroencephalogram monitoring may be helpful[6]. Patients with HS and encephalopathy due to ALF deteriorate very rapidly. Therefore, despite the fact that no criteria for an emergency liver transplant were met, we decided on early referral based on worsening of liver function and DIC.
DIC can develop during the first 3 days of HS and may lead to overestimation of the emergent need for LT. Ichai et al. identified some cases with a good outcome that did not undergo transplantation despite being listed too early for LT[6]. Replacement of clotting factors and platelets may be necessary. According to Epstein and Yanovich, in patients with hepatic failure, prothrombin complex concentrate to achieve a target INR ≤1.5 should be considered[1]. However, this procedure conceals trends in the INR, which is an important marker of prognosis.
Despite being a therapeutic strategy for patients with HS and ALF who fail to improve with supportive measures, currently there are no validated tools to predict the need for or survival with LT. The KCH (non-paracetamol) and Clichy-Villejuif criteria appear to be poorly adapted to HS-related ALF[5]. In the multicentre retrospective study of Ichai et al., HS involving severe ALI with or without other organ dysfunction, improved in more than 80% of the cases with medical therapy alone. LT also achieved a good survival rate[6]. The decision to transplant is complex and should take into account the evolving dynamics of the patient, the likelihood of recovery and post-transplant issues such as the impact of life-long immunosuppression. Liver biopsy is not recommended to help in the selection of a patient who would require LT, unless other aetiologies are suspected[6]. The reasons why watchful waiting for our patient after referral was decided upon were related to the good initial evolution of neurologic and renal dysfunction, the possible overestimation of impaired coagulation due to DIC and the limited outcome related to LT in HS in previous case studies. Further clinical experience is needed to establish a scoring system for stratification of severity and to weigh the potential risks and benefits of conservative therapy versus organ transplantation to treat ALF associated with HS.
- Epstein Y, Yanovich R. Heatstroke. N Engl J Med 2019;380(25):2449–2459.
- Casa DJ, Armstrong LE, Kenny GP, O’Connor FG, Huggins RA. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep 2012;11(3):115–123.
- Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician 2005;71(11):2133–2140.
- Insfran LAM, Gago FA, Romero PR, Campos PC, Carbonell G, Barona L, et al. Liver transplantation for fulminant hepatic failure due to heat stroke: a case report. Transplant Proc 2019;51(1):87–89.
- Davis BC, Tillman H, Chung RT, Stravitz RT, Reddy R, Fontana RJ, et al. Heat stroke leading to acute liver injury & failure: a case series from the Acute Liver Failure Study Group. Liver Int 2017;37(4):509–513.
- Ichai P, Laurent-Bellue A, Camus C, Moreau D, Boutonnet M, Saliba F et al. Liver transplantation in patients with liver failure related to exertional heatstroke. J Hepatol 2019;70(3):431–439.