ABSTRACT
Introduction: Diabetic myonecrosis is an uncommon complication of diabetes mellitus, most often occurring in patients with poorly controlled, insulin-dependent diabetes. Its etiology is poorly understood, with many suggesting microvascular occlusion to be a key factor resulting in necrosis of skeletal muscle.
Case presentation: A 28-year-old male with a history of poorly controlled type I diabetes mellitus and end-stage renal disease requiring dialysis presented to the emergency department with severe pain of the lower extremities bilaterally.
Results: Work-up included an x-ray, which demonstrated no acute fractures but extensive vascular calcification of the lower extremities, and Doppler ultrasonography, which showed no DVT. MRI demonstrated severe muscular edema with patchy, geographic areas of sparing, which, in conjunction with the patient’s clinical presentation, allowed for a diagnosis of diabetic myonecrosis. He underwent conservative treatment, consisting of rest and pain management, leading to resolution of symptoms.
Discussion: Diabetic myonecrosis, although uncommon, can be easily diagnosed with a high degree of clinical suspicion. It typically presents in a patient with poorly controlled diabetes, and will commonly involve the proximal muscles of the lower extremity unilaterally, but may present bilaterally and involve the distal muscles, as demonstrated in this case. Diagnosis is made via MRI, and it is treated conservatively with pain management and rest. Most cases resolve with conservative management but recurrence is common.
LEARNING POINTS
- Diabetic myonecrosis is an uncommon complication of diabetes mellitus, most often occurring in patients with poorly controlled, insulin-dependent diabetes presenting with significant unilateral lower extremity pain, although bilateral presentation is also possible.
- A diagnosis of diabetic myonecrosis can be easily made with MRI, which demonstrates highly characteristic muscular edema with patchy areas of geographic sparing, but a high degree of clinical suspicion is necessary to reach a diagnosis.
- Recurrence of diabetic myonecrosis is common, and should be suspected in patients who have a history of this condition presenting with recurrent musculoskeletal pain, even if this pain is localized to a different muscle group.
KEYWORDS
Diabetes mellitus, myonecrosis
CASE DESCRIPTION
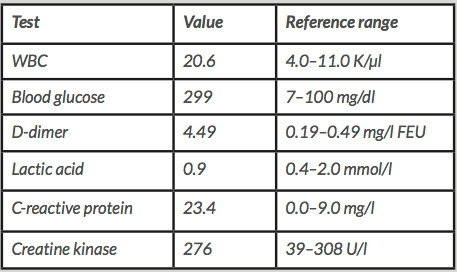
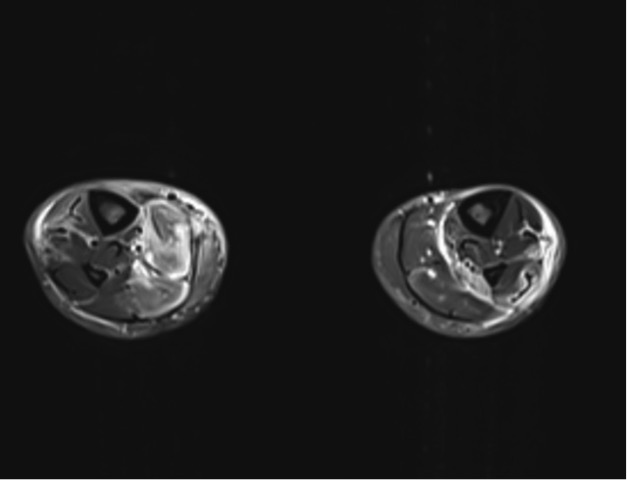
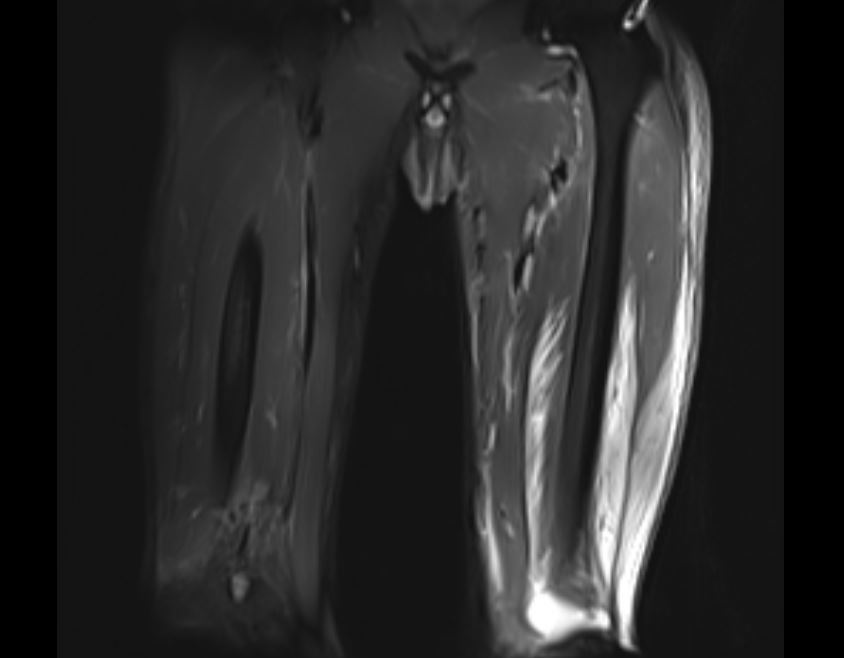
A 28-year-old male with a history of poorly controlled type I diabetes mellitus with end-stage renal disease requiring dialysis presented to the emergency department with severe pain of the lower extremities bilaterally, associated with weakness, inability to bear weight and loss of sensation. The pain initially occurred in the right lower extremity 2 days prior to presentation and progressed to involve the left lower extremity, with pain most prominent in the calf muscles. The physical examination was remarkable for erythema and edema of the lower extremities, without crepitus. At the time of admission, the patient’s blood glucose was 299 mg/dl and his most recent HbA1c measurement from 6 months prior was 7.7. Initial work-up included an x-ray, which demonstrated no acute fractures but extensive vascular calcification of the lower extremities (Fig. 1), and Doppler ultrasonography, which showed no DVT. Laboratory studies (Table 1) demonstrated leucocytosis, elevated D-dimer levels and normal lactate levels. MRI demonstrated severe muscular edema with patchy, geographic areas of sparing (Figs. 2 and 3), which, in conjunction with the patient’s clinical presentation and evidence of extensive vascular calcification, allowed for a diagnosis of diabetic myonecrosis.
Figure 1. Right lower extremity x-ray demonstrating extensive vascular calcification and no acute fracture
Table 1. Laboratory test values at time of presentation to the emergency department
Figure 2. MRI demonstrating diabetic myonecrosis (muscular edema with patchy, geographic areas of sparing)
Figure 3. MRI demonstrating diabetic myonecrosis
The patient was started on scheduled oxycodone in addition to already scheduled gabapentin and acetaminophen for symptomatic treatment. No drainable fluid collection was identified. The remainder of the patient’s hospital course consisted of pain control and management of his diabetes mellitus. He was discharged on hospital day 10 and continues to work to manage his diabetes and end-stage renal disease.
Methods and Procedures
A diagnosis was reached via MRI of the lower extremities, which demonstrated severe muscular edema with patchy, geographic areas of sparing, which is highly characteristic of diabetic myonecrosis. Tissue biopsy was not obtained due to the high risk of infection and concern for poor wound healing. MRI, in addition to the patient’s history of poorly controlled diabetes and his clinical presentation, allowed for a diagnosis of diabetic myonecrosis. The patient underwent conservative management consisting of rest and pain control, which led to resolution of symptoms.
DISCUSSION
Diabetic myonecrosis is a rare complication of diabetes mellitus, but is readily identifiable with a high degree of clinical suspicion. Its etiology is poorly understood and thought to involve microvascular occlusion, resulting in necrosis of skeletal muscle[1]. It typically presents in the proximal muscles of the lower extremities, and less commonly presents bilaterally, or in the distal muscle groups[2,3]. Patients who develop myonecrosis typically have other diabetes-related complications, including retinopathy, nephropathy and neuropathy[2]. The mean age of development is 44 years and, on average, patients have been insulin-dependent for 14 years prior to presentation[4]. MRI is the best technique for diagnosis, as it is minimally invasive and myonecrosis is noted to have a very distinctive, easily recognizable appearance via this scan[4,5]. This complication is treated conservatively with bed rest, analgesia and glycemic control, but recurrence is common, occurring in as many as 45% of patients treated conservatively[2]. The presented case demonstrates an uncommon presentation of diabetic myonecrosis, in that the patient presented with myonecrosis bilaterally, and in the calf muscles. However, with his history of poorly controlled diabetes complicated by diabetic nephropathy, clinical suspicion was present for further evaluation via MRI, which was able to demonstrate the characteristic findings seen with myonecrosis.