ABSTRACT
Introduction: Various agents can lead to an acquired methaemoglobinaemia (MHB) with potentially fatal consequences. There is a lack of literature on the formation of methaemoglobin (MH) in the blood after the intake of poppers (amyl nitrite). Poppers are a popular aphrodisiac agent.
Case description: A 56-year-old diabetic called an ambulance after using poppers in a brothel with subsequent associated acrocyanosis, confusion and headache. The paramedics reported tachycardia and blood glucose of 3.8 mmol/l. The arterial blood gas analysis in the Emergency Department (ED) revealed a MHB of 23.1%. MH levels decreased rapidly without antidotal therapy. The patient was discharged the next day free of symptoms.
Discussion: This case illustrates the potential risks of taking poppers. A wide spectrum of symptoms were present in our patient. For the differential diagnosis of acquired MHB, poppers should be considered.
LEARNING POINTS
- In rare cases, using poppers can cause MHB and should be considered when taking a history.
- Cyanosis that does not respond to oxygen supplementation should raise the suspicion of MHB.
KEYWORDS
Methaemoglobinaemia, poppers, amyl nitrite hypoglycaemia
INTRODCTION
Methaemoglobin (MH) is the oxidized haemoglobin molecule. The accumulation of ferric ion (Fe3+) impairs the ability to bind and transport oxygen and leads to tissue hypoxaemia. Methaemoglobinaemia (MHB), defined as an MH level over 1%, can be the result of many causes, most commonly antimicrobials such as dapsone and sulphonamide or local anaesthetics like benzocaine and lidocaine[1]. The symptoms can vary from mild nonspecific symptoms to death[2-5].
Poppers, short-acting potent vasodilators (amyl nitrite), were used therapeutically in the past for angina pectoris. Since the 1960s, they have become a popular aphrodisiac. Their use supposedly leads to increased sexual pleasure and prolonged orgasm and is legal in Switzerland. Only a few cases of MHB induced by poppers are documented[6-8].
CASE HISTORY
A 56-year-old-white man with a history of hypertension, epilepsy and diabetes type I called an ambulance after the intake of inhalative poppers in a brothel. He presented to the paramedics with acrocyanosis, tachycardia, dizziness, coordination problems and headache. His medical treatment included a daily dose of valsartan/amlodipine (80/5 mg), levetiracetam (250 mg), aspirin (100 mg), long-acting insulin (18 IU) and short-acting insulin in accordance with an intensified insulin therapy.
On admission, the patient was disoriented. He was normotensive (128/68 mmHg), and his heart rate was 100 bpm. Initial oxygen saturation was 90% on 15 l/min of oxygen with a non-rebreather mask. Acrocyanosis that did not respond to oxygen administration was noted on physical examination. Further, a 2 mm anisocoria with non-light-reacting pupils was found. The remaining physical examination was unremarkable. Laboratory examinations revealed an increased creatinine level (127 µmol/l). Arterial blood gas analysis showed mild non-anion gap metabolic acidosis with inadequate respiratory compensation (pH 7.361, bicarbonate 18.3 mmol/l, PCO2 33.2 mmHg, PO2 222.7 mmHg, base excess –5.7 mmol/l), and MH of 23.1%. Glucose was slightly lower (3.3 mmol/l) than that measured by the paramedics. Electrocardiogram was normal. Due to an observed anisocoria, a neurological consultation and a cranial computed tomography angiogram were performed. No signs of stroke or bleeding were found.
The patient was admitted to our observation unit. Glucose (20 g) was given i.v. push since glucose levels had further decreased to 3.0 mmol/l. The patient's mental status normalized within 60 min, as well as oxygen saturation and glucose levels.
MH levels declined to 1% without antidotal therapy and acrocyanosis disappeared. Subsequently, the patient was discharged in good condition 12 h after presentation.
DISCUSSION
An association between poppers use and sexually transmitted disease in homosexual men was noted in previous studies[9-11]. The link between inhaling poppers and MHB was first recognized by Machabert et al. in 1994[12].
Symptoms of MHB depend on MH levels, which are reported as percentages of total haemoglobin. Percentages of 70% and higher can be deadly; a percentage higher than 50% may cause cardiac arrhythmias, seizures and severe lactic acidosis. In the range of 15%–50%, the symptom spectrum can be wide and range from confusion, dyspnoea, tachycardia or dizziness to headache. A level under 15% rarely leads to symptoms[1]. None of these symptoms are specific to MHB.
Moos et al. described the challenges for the physician regarding correct diagnosis and adequate treatment[13]. Standard pulse oximetry does not identify MH levels and MHB affects measurement of oxygen partial pressure (PO2) by showing falsely high values: 222.7 mmHg in our patient[14]. PO2 reflects only a small fraction of total oxygen that is dissolved in blood plasma. The diffusion of oxygen from the alveoli to blood plasma mostly determines the PO2 value and is not impaired by MHB. Therefore, oxygen administration leads to a high PO2 but does not improve oxygen saturation, because oxygen is not able to bind to haemoglobin in MHB[15]. Consequently, cyanosis and low oxygen saturation persist despite oxygen supplementation.
Therapeutic measures like methylene blue administration may lead to severe adverse drug reactions[16]. In particular, a glucose-6-phosphate dehydrogenase deficiency should ideally be excluded before antidote administration to prevent Heinz body anaemia; this is impossible in an acute care setting. Antidotal therapy with methylene blue is usually recommended at MHB levels of 20%–30%[13]. In our case, no antidotal therapy was initiated due to the fast decrease of MH levels and the prompt clinical improvement.
However, the patient presented with an MHB of 23.1%, which was high considering a single inhaled dose of poppers.
An incorrect history or a particular vulnerability due to a cytochrome b5 deficiency are possible explanations. The patient was a regular consumer of poppers and had never reported any complaints associated with their use.
Wright et al. emphasize the importance of glucose supplementation in patients with acquired MHB[1]. Glucose is an important substrate for the endogenous reducing enzyme cytochrome b5 reductase.
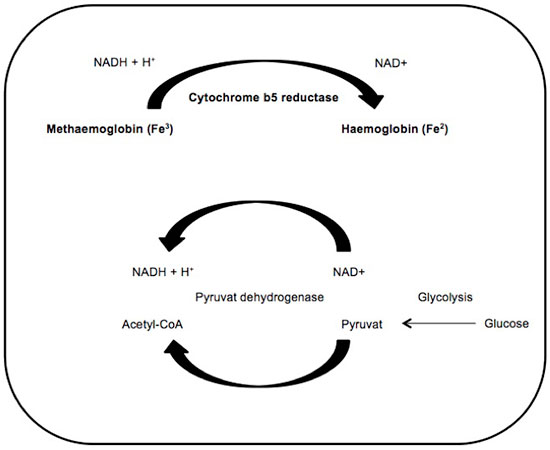
The inset of Fig. 1 depicts MH reduction through cytochrome b5 reductase and glycolysis as the main sources for the cofactor NADH (Nicotinamide adenine dinucleotide).
Figure 1: MB reduction. The cytochrome b5 reductase system is the predominant system for MH reduction and NADH supply through glycolysis
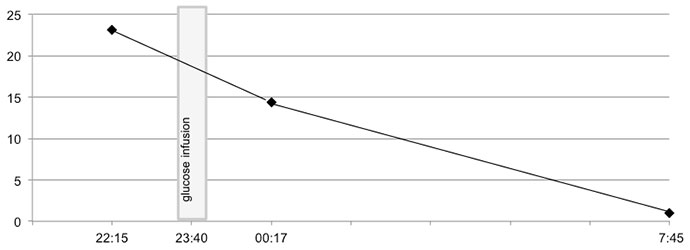
The normal reconversion rate of MH into haemoglobin is about 15% per hour[1]. In the first arterial blood gas analysis, an MH value of 23.1% was obtained (Table 1 and Fig. 2).
| Parameter | Measured value | Unit | Normal values |
|---|---|---|---|
| Temperature | 310.15 | kelvin | 309.15-310.15 |
| pH value | 7.361** | 7.38-7.42 | |
| Bicarbonate | 18.3** | mmol/l | 21-26 |
| Base excess | -5.7** | mmol/l | -2.0-3.0 |
| PCO2 | 33.2** | mmHg | 35-45 |
| PO2 | 222.7* | mmHg | 80-100 |
| Sodium | 139 | mmol/l | 135-145 |
| Potassium | 4.7 | mmol/l | 3.6-4.8 |
| Chloride | 114* | mmol/l | 95.0-105.0 |
| Anion gap | 6.7** | mmol/l | 8.0-16.0 |
| Glucose | 3.3** | mmol/l | 4.3-6.4 |
| Lactate | 1.8 | mmol/l | <1.8 |
| O2 saturation | 99.0 | % | |
| Oxyhaemoglobin | 77.0** | % | 90-95 |
| Methaemoglobin | 23.1* | % | <1.0 |
*upper reference range
**lower reference range
Table 1 - Arterial blood gas analysis on admission
Approximately half an hour later, glucose supplementation was started. Two hours after the first arterial blood gas analysis, the MH level was 14.4%. The MHB reconversion rate was approximately 38% in 2 hours and is higher than the expected reconversion rate of 30%[1]. Therefore, one might speculate that glucose substitution accelerated therapeutic success in our patient. Nevertheless, the higher reduction rate could have occurred by chance. Anisocoria in our patient remains unexplained and has never been described in the literature associated with the use of poppers.
In summary, the intake of poppers can lead to various adverse events, which might be misinterpreted in an emergency situation. Poppers should be considered as a potential trigger of acquired MHB.