ABSTRACT
Polyarteritis nodosa is a systemic necrotizing vasculitis that typically affects medium-sized muscular arteries, with occasional involvement of small muscular arteries. Most cases of polyarteritis nodosa are idiopathic but multiple infectious agents have been associated with this disease. We present a clinical case of a 72-year-old male with fever, diarrhoea and haemodynamic instability, diagnosed with a bacterial infection caused by Salmonella Typhi. One week after clinical resolution of the infection, the patient developed purpuric lesions with ulcers, pustules and necrotic areas accompanied by testicular pain and weight loss of 5 kg over the previous 15 days. A skin biopsy was performed and it revealed typical histologic signs of polyarteritis nodosa. The aetiologic association between bacteria of the genus Salmonella and polyarteritis nodosa has been previously described in the scientific literature but seldom meeting classification criteria and with histologic confirmation.
LEARNING POINTS
- Polyarteritis nodosa is a systemic necrotizing vasculitis associated with a multitude of aetiologic agents.
- Salmonella infection might be a possible trigger for the development of polyarteritis nodosa.
- A high index of suspicion and awareness is essential for a swift diagnosis and treatment of this disease.
KEYWORDS
Polyarteritis nodosa, Salmonella, Salmonella Typhi, vasculitis
CASE DESCRIPTION
The authors present a case of a 72-year-old male, with a past medical history of diabetes mellitus and arterial hypertension, who was admitted to the emergency department due to fever and diarrhoea with 4-day evolution. On the physical evaluation, the patient was hypotensive (blood pressure of 84/44 mmHg) and dehydrated, without any other significant findings. Blood analysis revealed leucocytosis (12,200/mm3) with neutrophilia (10,800/mm3), elevated C-reactive protein (9.5 mg/dl) and an acute kidney injury (creatinine 7.34 mg/dl). Due to haemodynamic instability, the patient needed aminergic support and renal replacement therapy. Blood cultures isolated Salmonella Typhi. The patient was treated with ciprofloxacin, in accordance with bacterial antibiotic susceptibility tests. With a positive clinical evolution he was discharged after completing antibiotic treatment, clinically asymptomatic.
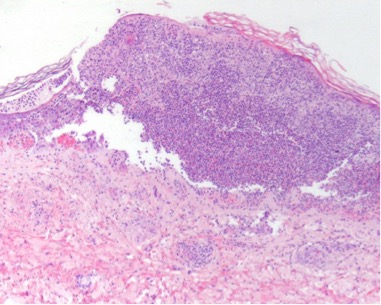
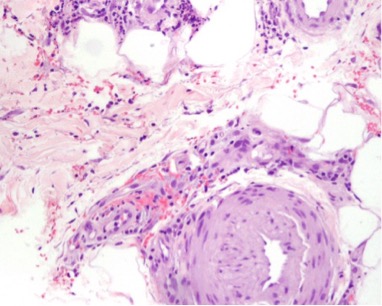
Three weeks after discharge, the patient was evaluated on a follow-up consult and complained of testicular pain and weight loss of 5 kg over the previous 15 days. On the physical evaluation, he presented multiple purpuric lesions with ulcers, pustules and necrotic tissue on his legs (Figs. 1 and 2) and petechiae on his arms. A cutaneous biopsy was performed, showing areas with detachment of the corneal layer with keratinocyte necrosis and abundant polymorphonuclear cells (Fig. 3) and polymorphonuclear infiltration of the arteries of the deep dermis and hypodermis with focal signs of vasculitis (Fig. 4), compatible with polyarteritis nodosa. The patient was treated with prednisolone, starting with 60 mg followed by progressive dose reduction, with complete remission of the skin lesions.
Figure 1. Purpuric lesions with pustules and necrotic tissue
Figure 2. Purpuric lesions with ulcers
Figure 3. Haematoxylin and eosin staining showing areas with detachment of the corneal layer with keratinocyte necrosis
Figure 4. Haematoxylin and eosin staining showing polymorphonuclear infiltration of the arteries with focal signs of vasculitis
DISCUSSION
Polyarteritis nodosa is a systemic necrotizing vasculitis that typically affects medium-sized muscular arteries, with occasional involvement of small muscular arteries[1]. Most cases of polyarteritis nodosa are idiopathic but some neoplastic diseases, genetic mutations and multiple infectious agents have been associated with this entity. The most extensively described in the literature are hepatitis B and hepatitis C but bacterial infections have also been linked to polyarteritis nodosa. The most frequently described bacterial infection is caused by the genus Streptococcus[2] but infections caused by Klebsiella, Pseudomonas and Yersinia[3], among others, have also been described.
The aetiology of polyarteritis nodosa is unknown, but T-cell mediation[4] and immune complex involvement (as evidenced by C3 and IgM deposits in the arterial walls)[5] have been implicated in the pathologic process.
There is biologic plausibility to the association of bacterial infection by the genus Salmonella and the development of polyarteritis nodosa. The interaction of bacteria of the genus Salmonella and Peyer’s patches leads to the induction of a T-cell response and production of IgM, IgG and IgA by B cells. This patient meets the American College of Rheumatology classification criteria for polyarteritis nodosa[6] and the clinical signs of the disease appearing 3 weeks after the Salmonella infection suggests a temporal association.
The aetiologic association between bacteria of the genus Salmonella and polyarteritis nodosa has been described previously in the scientific literature but seldom with histologic and clinical confirmation.