ABSTRACT
Cardiopulmonary resuscitation-induced consciousness is a rarely described and often misunderstood phenomenon, although it can be encountered. High quality cardiopulmonary resuscitation (CPR) may lead a patient to recover consciousness while in cardiac arrest. The authors present the case of an 89-year-old male patient who received CPR after a cardiac arrest. Spontaneous movements during CPR were noted and prompted several CPR interruptions. These movements immediately stopped during chest compression pauses. Physical restraint was used in order to be able to continue with the CPR algorithm, but sedation may be the best approach. Guidelines on how to identify and manage these cases need to be developed.
LEARNING POINTS
- Although rare, cardiopulmonary resuscitation-induced consciousness is a phenomenon that physicians should be aware of, given the implications it may have during resuscitation manoeuvres.
- Cardiopulmonary resuscitation-induced consciousness can readily be recognised by the presence during cardiac arrest of spontaneous and purposeful patient movements that immediately cease after stopping chest compressions.
- The use of sedative and analgesic drugs such as ketamine may be the best choice to manage cardiopulmonary resuscitation-induced consciousness, as an alternative to physical restraint.
KEYWORDS
Cardiopulmonary resuscitation, consciousness, cardiac arrest
INTRODUCTION
Cardiac arrest is characterised as a state of unconsciousness associated with the absence of vital signs. The main objective of cardiopulmonary resuscitation (CPR) is to ensure maintenance of cerebral and coronary perfusion, with the aim of limiting cell damage caused by anoxia until recovery of spontaneous circulation (ROSC).
Enhanced techniques and devices used during CPR, together with the focus on minimal interruption of chest compressions (CCs) and on their quality, have improved cerebral and coronary perfusion, which still does not exceed 30-40% and 10-30%, respectively[1]. There are several reports of patients who, although far from physiological perfusion values, have shown signs of CPR-induced consciousness (CPRIC). Although there is no globally recognised definition, CPRIC may be characterised by the presence of spontaneous eye opening, arm, leg or trunk movements, speaking, following orders, pain perception and even resistance to CPR during cardiac arrest (CA). All these manifestations immediately cease during CC interruptions. There are no data explaining why and under what conditions CPRIC may occur. Some authors suggest that several variables are involved, such as self-regulation, comorbidities and different cerebral ischaemic thresholds[2]. The apparent increasing incidence of this phenomenon creates new challenges for CPR providers and may even compromise the outcome of CPR in combative patients. In addition, there is a growing number of reports of patients who remember what happened during CPR[3], which may have serious psychological consequences for survivors. Currently, there are no guidelines on CPRIC management, and the decision on analgesia and sedation is therefore made based on the basis of the resuscitation team’s experience and clinical perception.
.
CASE REPORT
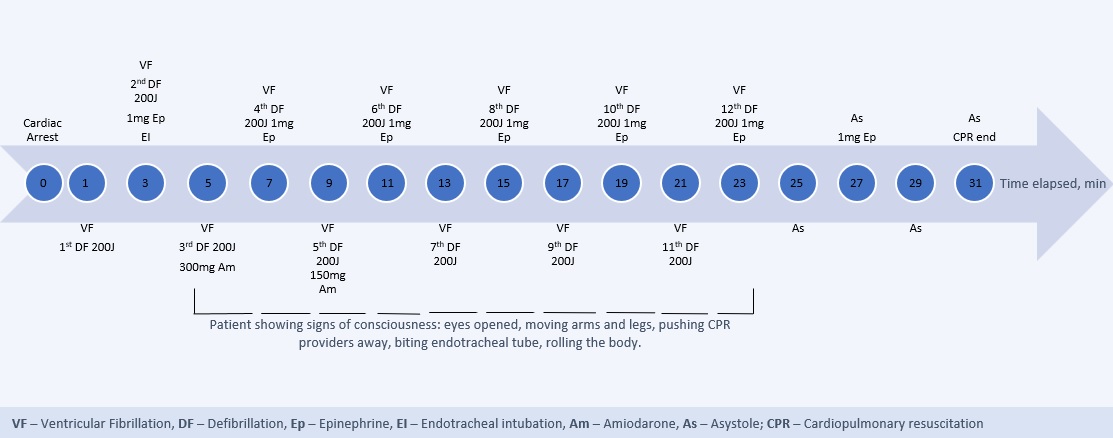
An 89-year-old male patient with a history of acute myocardial infarction 20 years earlier was admitted to the emergency department complaining of chest pain. A few minutes after arrival he became unresponsive and pulseless. CPR was immediately initiated and, on monitoring, ventricular fibrillation (VF) was noted, for which a first 200 J shock was delivered. CPR was continued, but the VF rhythm was still present after 2 minutes. A second shock of 200 J was administered, followed by 1 mg of epinephrine and endotracheal intubation. About 5 minutes after his CA, the patient presented lower limb movements. After CC interruption, those movements ceased, with the documented rhythm still being VF. CCs were restarted and a third shock was given, as well as 300 mg of amiodarone. Capnography showed an end-tidal carbon dioxide value of 14-16 mmHg and shortly after CC resumption, the patient resumed the lower limb movements. CPR was interrupted a further time for rhythm confirmation, and during this interruption all movements stopped again. An advanced life support protocol was maintained for a further 20 minutes (Fig. 1). Several CPR interruptions were necessary during this period, as the patient tried to push away the CPR provider with his hands, bit endotracheal tube, showed facial signs of pain, and tried to move sideways. Physical restraint was necessary in order to continue the CPR. Patient sedation was considered, but due to uncertainty over its possible implications for the success of the resuscitation, it was not performed. After 24 minutes of CPR, the patient's signs of consciousness progressively decreased. The following rhythm assessment revealed asystole. CPR was maintained for a further 5 minutes, without any additional signs of consciousness being noted. Asystole rhythm persisted and, taking into account the patient's age and CA duration time, all the team members agreed to suspend CPR.
DISCUSSION
We present the case of a patient who presented clinical signs consistent with CPRIC. His movements interfered with the resuscitation efforts and led to an increased number of CPR interruptions, either for rhythm confirmation or because it was impossible to continue applying CCs. There is a gap in the literature regarding not only how to identify CPRIC, but also how to manage it. This phenomenon appears to be more likely to appear in young male patients who are quickly assisted after CA and in patients with VF or pulseless ventricular tachycardia. Some previously reported cases present certain similarities with our patient[2,3], but we found no other reports of CPRIC in such an elderly patient. Although either manual or mechanical compressions may lead to CPRIC; the latter appear to enhance its occurrence, which may be partly explained by greater effectiveness of the CCs and shorter interruption times. High quality CCs, as we documented by capnography, may lead to improved cerebral perfusion and, as a consequence, potentiate the occurrence of CPRIC. However, there are few cases in which the quality of CPR was documented in any way.
Although it carries a risk of injury if the patient remains combative, physical restraint may be necessary in order to be able to continue delivering CPR[4]. We now believe that patient sedation and analgesia would have been the most suitable management. Nevertheless, in an attempt to minimise CPR interruptions and increase the likelihood of ROSC, if no other options are available, physical restraint may be a choice to consider. The use of sedative and analgesic drugs has greater potential to provide better quality care, although evidence on their safety is lacking. The choice of drug used must take into account not only its sedative and analgesic effect but also its haemodynamic properties. Ketamine may be an ideal agent given its rapid onset, mixed sedative and analgesic effect and haemodynamic properties. Its use has previously been documented and several doses have been suggested, but to date there is no published evidence able to support its use. We only found one Dutch guideline regarding the management of patients who were agitated or in pain during CCs, which suggested the use of fentanyl and midazolam[5].
With this report, the authors underline the need to establish a globally accepted definition of CPRIC. It is crucial to establish clear algorithms focusing not only on the recognition of this phenomenon, but also on the best way to manage it.