ABSTRACT
Cystic mesotheliomas (also called mesothelial inclusion cysts) are rare benign neoplasms that occur more often in young women. Symptoms are usually non-specific, demanding a thorough work-up. We report a case of a 40-year-old female patient with 2 prior caesarean sections presenting with a 3-month history of abdominal pain. Laboratory tests revealed microcytic hypochromic anaemia and an elevated tumour marker CA-125. An investigation identified a large cystic abdominal mass, mostly in the left side of the abdomen. A laparotomy was performed with total resection of the lesion. Histological assessment resulted in a diagnosis of a mesothelial inclusion cyst. The patient had no recurrence after 3 years.
LEARNING POINTS
- Peritoneal mesotheliomas are rare conditions, and with benign features are even rarer.
- Mesothelial inclusion cysts, also known as benign cystic mesothelioma, occur more often in young to middle-aged women with excellent prognosis, although there are high rates of local recurrence.
- Investigation unmasks large abdominal lesions. A timely diagnosis is of the utmost importance, to prevent a dramatic change in outcome if severe complications develop.
KEYWORDS
Mesothelial inclusion cyst, benign mesothelioma, mesenteric cyst, peritoneal mesothelioma, neoplasm
CASE DESCRIPTION
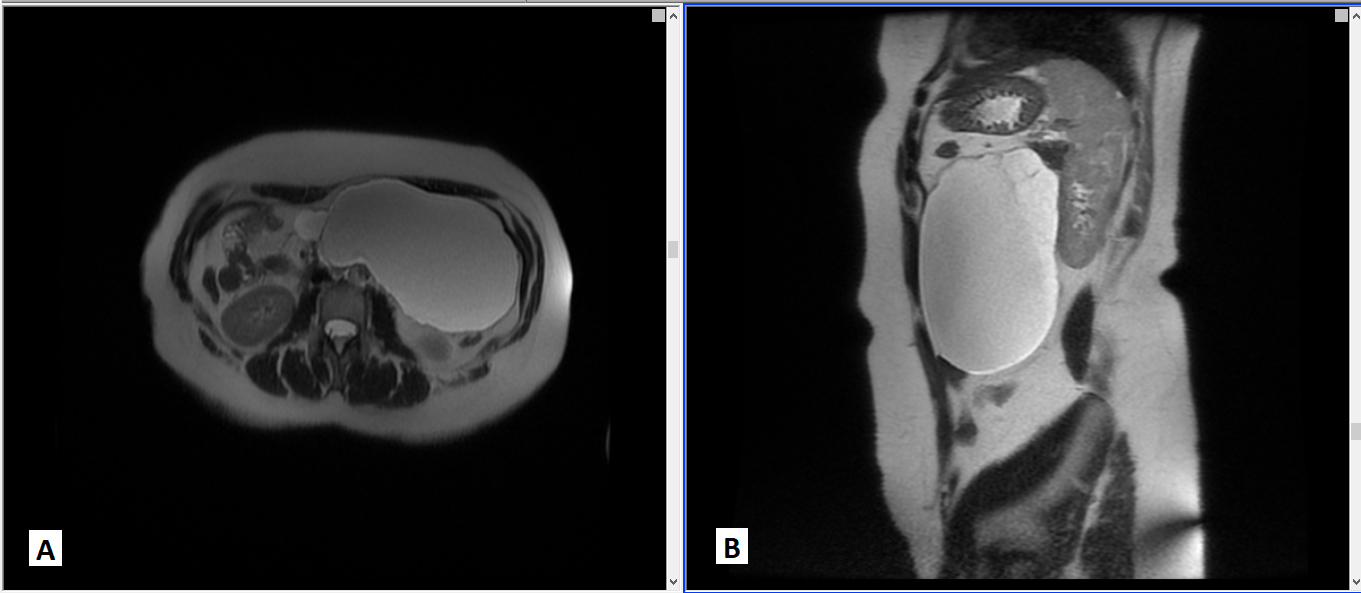
A 40-year-old Caucasian woman with a past medical history of grade 1 obesity, hypothyroidism, idiopathic hyperprolactinaemia and two caesarean deliveries presented with diffuse abdominal pain and abdominal bloating, over the previous 3 months. There were no constitutional symptoms. On physical examination, there was no palpable mass and the remainder of the physical examination was unremarkable. Laboratory investigation revealed microcytic hypochromic anaemia and an elevated tumour marker CA-125. As we initially suspected a malignant disease, a thoraco-abdomino-pelvic computed tomography (CT) scan was required (non-contrast-enhanced, patient option). This examination found a well-defined, large, hypodense mass, localized to the left side of the abdomen. The remaining examination was normal. Owing to the limitation of the CT scan (lack of contrast), abdomino-pelvic magnetic resonance imaging (MRI) was performed and confirmed a 16 cm abdominal cystic neoplasm, with thin internal septa, T1 hypointense and T2 hyperintense, with the signal intensity of water (Fig. 1). Posterior displacement of the left kidney was noted and it seemed to be pancreas-related. Due to the large size and the uncertainty of the aetiology, a laparotomy was performed with total resection.
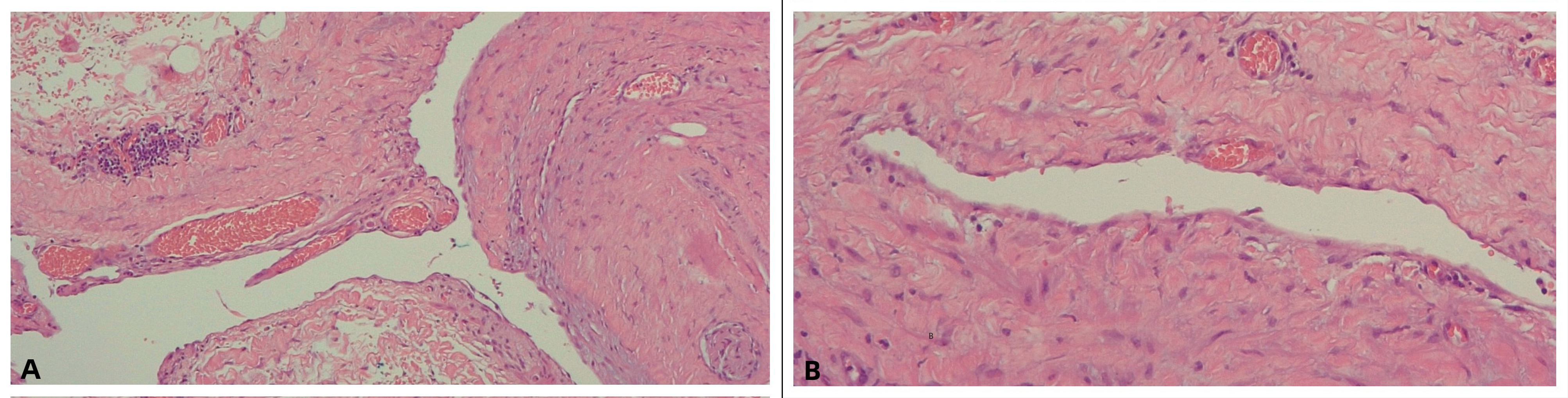
A mesenteric cystic neoplasm, near the root of the mesentery, was found. Histological assessment revealed a cavitated lesion lined by a single layer of flattened cells with a fibrous wall, thereby classified as a peritoneal mesothelial inclusion cyst or benign cystic mesothelioma (BCM) (Fig. 2). After 3 years of close follow-up of the patient, there is no evidence of recurrence.
Figure 1. Abdominal MRI. Axial (A) and sagittal (B) T2-weighted images showing the extension of a fluid-filled cystic lesion in the left hypochondrium
Figure 2. Photograph of histological findings showing a cystic lesion lined by a single layer of flattened mesothelial cells with a fibrous cyst wall. (A) H&E staining x100; (B) x200
DISCUSSION
Mesenteric cysts are rare intra-abdominal lesions with an estimated incidence of 1 in 100,000 for adults and 1 in 20,000 for children. The exact aetiology is unknown, and although diverse classifications have been described, the histopathologic classification has the greatest acceptance, as defined by the cells of the inner layer of the cyst wall and the cyst origin. Therefore, mesenteric cysts can be lymphatic, mesothelial, enteric, of urogenital origin, mature cystic teratomas (dermoid cysts) and non-pancreatic pseudocysts[1]. The distinction between lymphatic and mesothelial cysts is important and can only be made histologically, as imaging techniques are usually not helpful in differentiating these. Peritoneal mesothelial cysts can be divided into simple mesothelial cysts (congenital), BCM (or peritoneal inclusion cysts) and malignant cystic mesothelioma[1,2].
Only approximately 130 cases of BCM have been reported. This rare condition occurs more often in young to middle-aged women and it has been associated with a history of previous abdominal surgeries, endometriosis or pelvic inflammatory disease[3]. In contrast to malignant peritoneal mesothelioma, BCM has no association with asbestos exposure[1,4]. In the case we report, the diagnosis was established in a young woman, and may be related to the history of abdominal surgeries.
Clinical presentation is commonly indolent. Symptoms are non-specific, mostly abdominal pain and an increase in abdominal girth, but also include nausea and vomiting, constipation and diarrhoea[1]. Symptoms are unveiled as a result of mass effect, since these masses can reach large sizes (a range of a few centimetres to 30 cm), or when other complications arise such as rupture, haemorrhage, erosion or infection[5].
As previously mentioned, cysts of lymphatic origin are a differential diagnosis of BCM, but so too are pseudomyxoma peritonei, endometriosis or other cystic neoplasms, benign or malignant.
Abdominal ultrasound identifies the cystic lesion and its location, but further imaging studies are indispensable to determine the extension, accurate location and content of the mass, and also, to delimitate anatomical relations and rule out complications. Radiologic features are of the utmost importance, although they do not allow differentiation of BCM from other cystic intra-abdominal neoplasms, such as cystic lymphangiomas or enteric duplication cysts[5]. Park et al. aimed to present the CT characteristics that may help to distinguish benign from malignant mesotheliomas. CT features of BCM describe a multilocular cystic mass, multiple thin-walled cysts or a unilocular cystic mass, while the CT findings for malignant peritoneal mesotheliomas can range from a “dry” aspect, a localized form with peritoneum-based masses, to a “wet” aspect, with diffuse irregular thickening of the peritoneum, ascites and a mass involving the omentum[4]. Moreover, malignant peritoneal mesotheliomas are usually diagnosed in the fifth and sixth decades of life and in association with asbestos contact. Histologically, the main distinction between malignant and benign mesotheliomas is made by evaluating the degree of cellular proliferation and atypia[1].
Though a benign clinical suspicion, surgery is highly recommended for large mesenteric cysts, as this excludes malignant transformation and avoids complications. Metastatic potential is not consensual, but malignant evolution of BCM has been documented[4] Therefore, in our case, a midline laparotomy was performed with surgical resection of the lesion, which was central to the accurate diagnosis of this benign condition.
The prognosis is excellent, since surgery is usually curative if a total resection is accomplished. Close long-term follow-up of these patients is advisable because of the high rates of local recurrence. In relapses, CT-guided cyst aspiration may help in diagnosis[3].
In conclusion, we report a case of a peritoneal mesothelial inclusion cyst or BCM. With this clinical case report, we would like to increase medical awareness of this rare entity and contribute to a better understanding of this pathology.
We also point out the good prognosis of this condition; nevertheless, correct pre-operative diagnosis is difficult – in the first instance, it is impossible not to suspect a malignant aetiology.