ABSTRACT
Mesenteric cysts are a rare nosologic entity, the diagnosis of which is complex due to their nonspecific presentation. They may emerge from any part of the mesentery and grow to any size, thus conditioning a wide range of clinical manifestations that renders them easily mistaken for different gastrointestinal pathologies. Diagnosis encompasses a mixture of clinical suspicion, imaging techniques and sometimes surgery, and curative treatment is based on complete surgical resection of the cyst. We hereby present a case of a mesenteric cyst that developed on the anterior abdominal wall of a 59-year-old man awaiting allogeneic bone marrow transplantation after being diagnosed with chronic myeloid leukaemia. He was admitted to the emergency room with complaints of an increased abdominal perimeter and increased weight, not associated with alterations to his dietary or physical exercise habits. Suspecting ascites in the context of leukaemic progression, the patient was admitted to the medical ward; however, subsequent study identified a mesenteric cyst as the most probable diagnosis and the patient was proposed to undergo surgery. He underwent laparotomic cyst excision without complications and the histological evaluation of the surgical specimen confirmed the diagnosis.
LEARNING POINTS
- Although rare entities, mesenteric cysts should be suspected whenever nonspecific gastrointestinal symptoms are present and liquid collections are identified.
- Treatment consists of complete surgical excision, which, although not free of complications, is usually safe and the recurrence rate is very low.
- In light of the lymphatic theory with respect to the aetiology of mesenteric cysts, this nosologic entity should be highly suspected in oncologic patients where lymphangiogenesis is potentiated.
KEYWORDS
Mesenteric cyst, chronic myeloid leukaemia, abdominal mass, ascites
CASE DESCRIPTION
A 59-year-old male patient, diagnosed 7 months previously with chronic myeloid leukaemia (CML), presented to the emergency ward with complaints of an increased abdominal perimeter and associated weight gain, with no accompanying changes to his lifestyle. He denied gastrointestinal symptoms, namely anorexia, nausea, vomiting or abdominal pain, and on his clinical record only a tubular adenoma with low-degree dysplasia diagnosed 1 year previously was listed. His chronic medication consisted only of hydroxyurea 500 mg once a day, and he was awaiting allogeneic bone marrow transplantation.
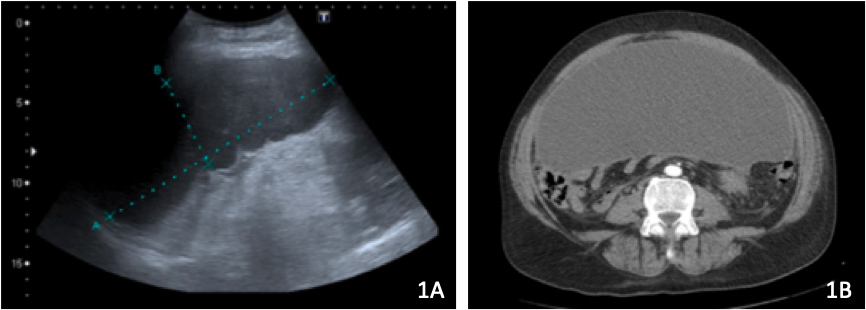
At admission, the patient presented as eupnoeic, apyretic and with normal blood pressure values and cardiopulmonary auscultation. His abdomen, however, was stretched, tense and barely depressible, with diminished abdominal sounds at auscultation. No peripheral oedema, namely of his lower limbs, was observed. Blood work-up revealed no significant alterations apart from neutrophilic leucocytosis (leucocytes 44,400 × 106; neutrophils 27,970 × 106) and increased C-reactive protein (CRP, 4.85 mg/dl); thyroid function was normal; HIV, CMV and hepatitis virus serologies were negative and a chest x-ray depicted elevation of both diaphragmatic domes. Abdominal ultrasonography identified a homogeneous splenomegaly along with a finely septated intraperitoneal effusion (Fig. 1A). Diagnostic paracentesis yielded a citrus-yellow ascitic liquid with normal glucose and protein levels, no neoplastic cells and no microbial growth, while a subsequent computed tomography (CT) approach revealed a well-defined and regularly thin-walled cystic lesion expanding into the anterior region of the abdominopelvic cavity, measuring approximately 26 × 27 × 12 cm of higher axes, encapsulating a simple liquid with density inferior to 20 HU (Fig. 1B). Adenopathies were also identified near the hepatic hilum, coeliac trunk, hepatoduodenal ligament and small gastric curvature, and no associated free peritoneal effusion was documented.
Figure 1. Radiographic study of the mesenteric cyst. 1A: Ultrasonography showing a finely septated intraperitoneal effusion in the anterior region of the abdominopelvic cavity. 1B: CT scan depicting the liquid content of the cyst, which was encapsulated by a regularly thin and well-defined wall
In light of the obtained results, the patient was admitted to the Internal Medicine Department. Following exclusion of leukaemic progression, his accompanying haematologist was contacted and the bone marrow transplantation was delayed until surgical excision of the cyst was carried out, as it would involve profound immunosuppression and there was a risk of potential complications. The patient was then addressed to the General Surgery Department and the cyst was excised using a laparotomic approach. Samples of both the content and wall of the cyst were collected and histological study established the diagnosis of a peritoneal pseudocyst of probable inflammatory nature containing a proteinaceous fluid with some lymphocytes and no malignant neoplastic cells. Three days after surgery, the patient was discharged and at the 1-month follow-up consultation he presented as asymptomatic. He is currently awaiting bone marrow transplantation.
DISCUSSION
With fewer than a 1,000 cases reported in the literature since the first publication in the 16th century, mesenteric cysts (MCs) are a rare nosologic entity, the aetiology and pathophysiology of which remain obscure. The prevalence rate has been estimated to be between 1 in 27,000 to 1 in 250,000 patients, with a predominance in white women in the fourth decade of life[1]. However, considering the absence of diagnostic criteria and the need for surgery to confirm the diagnosis and for treatment, the statistics are probably biased with respect to access to medical care.
MCs are grossly divided into true cysts and pseudocysts, depending upon whether the membranes have 3 cellular layers (serous, muscular and epithelial/endothelial) or not. They may be simple or multiple, uni- or multilocular, can adopt any size and shape, can form anywhere along the mesentery and can extend to the retroperitoneum. The majority of those structures form at the small bowel mesentery, although nearly one-quarter were observed in the large bowel mesentery[1]. The malignancy rate approaches 3%, and although this may affect any cyst, it was reported higher among cysts with solid components[2]. Excluding malignancy may sometimes be essential, as highlighted in our case, where confirmation of the benign nature of the cyst was decisive in proposing the patient for bone marrow transplantation. However, as the treatment is extremely efficient and safe, diagnosis, malignancy confirmation and treatment are performed in 1 sole procedure (surgery), recommended for virtually all patients.
The most widely accepted theory regarding the aetiology of MCs advocates that they may derive either from an obstruction to the lymphatic drainage or from a miscommunication between the lymph nodes and the lymphatic or venous systems following benign proliferation of ectopic lymphatics[3]. This second option is of particular interest in the setting of oncologic patients, where the pro-inflammatory environment and activation of the invasion-metastasis cascade are associated with lymphangiogenesis[4].
The clinical presentation of MCs is nonspecific and extremely variable. The cardinal symptom is abdominal pain, present in more than 80% of patients, generally associated with nausea, vomiting and alterations in intestinal elimination patterns. Not infrequently, these tumours are mistaken for ascites, as happened in our clinical case. Diagnosis is based on a combination of clinical suspicion and imaging techniques, generally ultrasound and CT, although MRI was found to be more precise and accurate[5]. Surgical excision of the cyst is the gold standard for MC treatment, sometimes demanding extended margins of resection encompassing parts of the intestine or other neighbouring structures. Either a laparoscopic or laparotomic approach is adequate, depending on the size and characteristics of the cyst. Prognosis is usually good, with early patient discharge and a return to normal life. The recurrence rate is low when complete resection with safety margins is performed[1].