ABSTRACT
Manifestations of chronic cutaneous lupus erythematosus are variable. Periorbital and facial swelling occurs in dermatomyositis and systemic lupus, but it has been rarely reported as a manifestation of exclusively cutaneous lupus. A 48-year-old woman presented with a 16-year history of asymptomatic, bilateral swelling and erythema of her face with marked worsening after sun exposure. No systemic symptoms were associated. A complete evaluation did not reveal other findings. Cutaneous biopsy showed features of lupus erythematosus. She was treated with photoprotection, topical tacrolimus, hydroxychloroquine and azathioprine with a partial response. Facial swelling with erythema represents quite an unusual manifestation of chronic cutaneous lupus erythematosus. Dermatomyositis, systemic lupus and Morbihan disease are the main differential diagnoses.
LEARNING POINTS
- Periorbital and facial swelling with erythema are clinical manifestations of dermatomyositis and systemic lupus erythematosus. However, these manifestations represent quite an unusual presentation of chronic cutaneous lupus erythematosus.
- The periorbital area is most frequently affected, while extensive facial involvement is much more unusual.
- A complete evaluation and cutaneous biopsy are essential to make the diagnosis and to rule out other disorders such as dermatomyositis, systemic lupus erythematosus and Morbihan disease.
KEYWORDS
Chronic cutaneous lupus erythematosus, erythema, oedema, face
INTRODUCTION
Cutaneous involvement in lupus erythematosus (LE) is quite common and includes a broad range of manifestations. Although facial swelling with erythema is a common presentation of systemic lupus erythematosus (SLE), it is quite an infrequent manifestation of exclusively cutaneous lupus.
CASE DESCRIPTION
A 48-year-old Caucasian woman was referred to the Department of Dermatology in September 2018 from another hospital. She presented with a 16-year history of asymptomatic swelling with erythema of her face. The erythema and swelling worsened after sun exposure. Initially, it occurred intermittently, but after 2 years it became permanent. At the same time, she presented patchy alopecia of the scalp. No systemic symptoms, aphthae, arthritis, Raynaud’s or muscle weakness were present Her past medical and family history was unremarkable. Physical examination showed oedema and marked erythema involving both cheeks and the forehead along with oedema of the eyelids (Fig. 1).
Figure 1. A, B. Marked oedema and erythema involving both cheeks, the nose and glabellar area. Bilateral oedema of eyelids
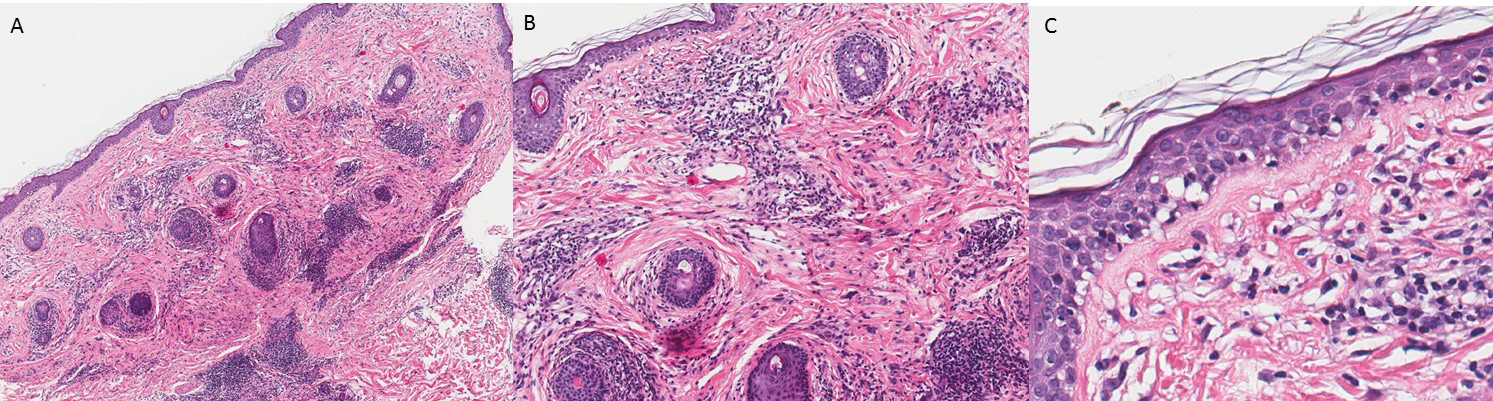
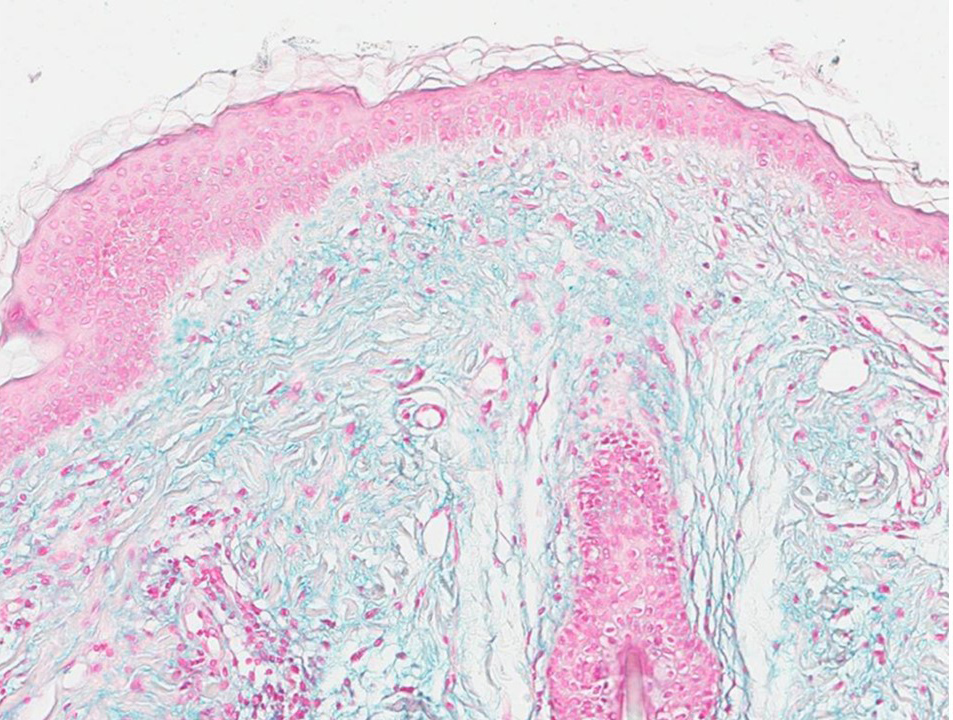
Moreover, two plaques of scarring alopecia were present on the scalp. Laboratory investigation [complete blood count, coagulation, erythrocyte sedimentation rate, C-reactive protein, liver function tests, creatinine, creatine kinase, aldolase, thyroid hormone, urinalysis, serologies for hepatitis B and C and HIV, complement levels, autoantibodies (including antinuclear antibody, anti-Ro (SSA), anti-La (SSB), anti-Jo-1, anti-Mi-2, anti-SRP, anti-MDA5)] yielded results that were within normal limits. Patch tests to standard and cosmetic products were negative. A cutaneous biopsy showed epidermal atrophy with mild hyperkeratosis and basal cell hydropic degeneration. In the dermis, there was a perivascular and periadnexal lymphocytic infiltrate (Fig. 2). Alcian blue staining showed mucin deposition (Fig. 3).
Figure 2. A. Biopsy of malar area showing superficial and deep perivascular and periadnexal lymphocytic infiltrate (haematoxylin and eosin, x100). B. Detail of the lymphocytic infiltrate (haematoxylin and eosin, x200). C. Epidermal atrophy with mild hyperkeratosis. Liquefaction degeneration of the basal cells. Lymphocytic infiltration in the papillary dermis (haematoxylin and eosin, x400).
Figure 3. Interstitial mucin deposition in the dermis (Alcian blue stain, x200)
An electromyography study and a high-resolution CT thoracic scan did not reveal alterations. The diagnosis was chronic cutaneous lupus erythematosus (CCLE). The patient was treated with strict photoprotection, topical tacrolimus and hydroxychloroquine 200 mg/12 h associated with prednisone 0.5 mg/kg/day for 1 month and tapered over the following 3 months with clinical improvement, but with relapse after withdrawal; therefore, azathioprine 2 mg/kg/day was added to hydroxychloroquine with a mild response.
DISCUSSION
Cutaneous manifestations of LE can be divided into 2 subgroups, LE-specific lesions and LE-nonspecific. LE-specific lesions are classified as acute cutaneous LE, subacute cutaneous LE and chronic cutaneous LE. Manifestations of CCLE are variable. Discoid LE (DLE), lupus profundus, chilblain LE and LE tumidus (LET) are different forms of CCLE presentation[1]. DLE is by far the most common form of CCLE. It is characterized by erythematosus, indurated plaques covered with adherent scales associated with hyperpigmentation, central hypopigmentation, telangiectasias and atrophic scarring. DLE typically affects the head and neck. LET is a less frequently occurring subtype of CCLE which often involves the face and trunk. Clinically, lesions are distinctly oedematous and infiltrated, while the scaling or atrophy present in DLE is absent. Photosensitivity is marked. Histologically, tumid LE shows little interface dermatitis and marked lymphocytic infiltration in the dermis with mucin deposition. Although SLE may present as facial swelling and erythema, these may appear as manifestations of an exclusively cutaneous lupus without systemic involvement[1–5]. Cyran et al. reported 2 cases with periorbital oedema and erythema and used the term CCLE to refer to this particular and uncommon subset of LE[3]. Likewise, in most cases, the periorbital area is the most commonly affected location and extensive facial involvement is described far less[4]. These patients have been diagnosed with DLE and also, LET, due to the absence of typical clinical features of DLE (including atrophy, hypopigmentation, scaling, scarring), marked photosensitivity and the absence of interface dermatitis in the biopsy; results from direct immunofluorescence testing are variable [1–5].
The diagnosis of CCLE presenting as facial oedema with erythema may be misdiagnosed because it can mimic other disorders. Therefore, a complete evaluation and cutaneous biopsy are essential to make the diagnosis. Dermatomyositis (DM) is considered in the differential diagnosis, since it frequently affects the face, and its presentation as periorbital and facial swelling with erythema is not uncommon. However, other skin lesions, musculoskeletal symptoms and signs of myopathy were absent in this patient. Furthermore, our patient presented with scarring alopecia of the scalp; scalp involvement in DM presents as diffuse erythematous and scaly plaques, poikiloderma and non-scarring alopecia. SLE may present as facial oedema, but our patient failed to meet the criteria for SLE after a prolonged course of disease. Morbihan syndrome is a rare entity that more commonly affects women in the third or fourth decade of life. This disorder is considered a special form of rosacea, characterized by the slow appearance of erythema and solid oedema on the upper portion of the face. The biopsy, although nonspecific, is characterized by perivascular dermal oedema with a lymphohistiocytic periadnexal infiltrate containing numerous mast cells and dilation of lymphatic vessels. Granulomas are sometimes present. Other differential diagnoses to be considered are orofacial granulomatosis, sarcoidosis, contact dermatitis, recurrent cellulitis/erysipelas, Hansen’s disease, cutaneous leishmaniasis, trichinosis, foreign body granuloma, superior vena cava syndrome, reactions to injectable fillers and scleroedema, among others.
Strict photoprotection, topical corticosteroids and calcineurin inhibitors are the first-line treatment. Antimalarials are the systemic treatment of choice for oedematous CCLE; azathioprine and thalidomide are useful in refractory cases. It is unknown whether this clinical presentation has a worse response to conventional treatments[1].
Chronic facial oedema with erythema is an unusual manifestation of CCLE and should be considered in the differential diagnosis. Despite its rarity, internal doctors should be familiar with this clinical presentation.