ABSTRACT
Mycobacterium tuberculosis affects the middle ear in rare cases and is a challenging diagnosis. In this case, we present a 57-year-old patient diagnosed with anti-neutrophil cytoplasmic antibody (ANCA)-negative granulomatosis with polyangiitis (GPA) following a biopsy result of nasal granulomas, who was immediately started on immunosuppressive treatment. Years later, she developed progressive hypoacusis. Magnetic resonance imaging (MRI) revealed an extensive mass in the tympanic cavity extending to the mastoid. A biopsy of the mass was positive for Mycobacterium tuberculosis. Immunosuppressants were weaned and the patient was started on anti-tuberculous therapy with resolution of the complaints and findings. Tuberculous infections are difficult to diagnose and frequently mimic other illnesses, but in our case, we believe that an indolent tuberculous process was present from the beginning and evolved under immunosuppressive therapy.
LEARNING POINTS
- The differential diagnosis of rhinosinus granulomatous findings includes inflammatory and infectious diseases (for example, tuberculous infections), in addition to neoplasms, cocaine abuse and trauma.
- A comprehensive differential diagnosis list is essential to mitigate diagnostic errors, especially in patients where auto-immune studies are negative or there is any doubt in the diagnosis.
- Latent tuberculosis screening should be a concern for physicians treating patients with immunosuppressive therapy, especially in endemic countries.
KEYWORDS
Tuberculosis, immunosuppression, mastoiditis, biopsy
CASE DESCRIPTION
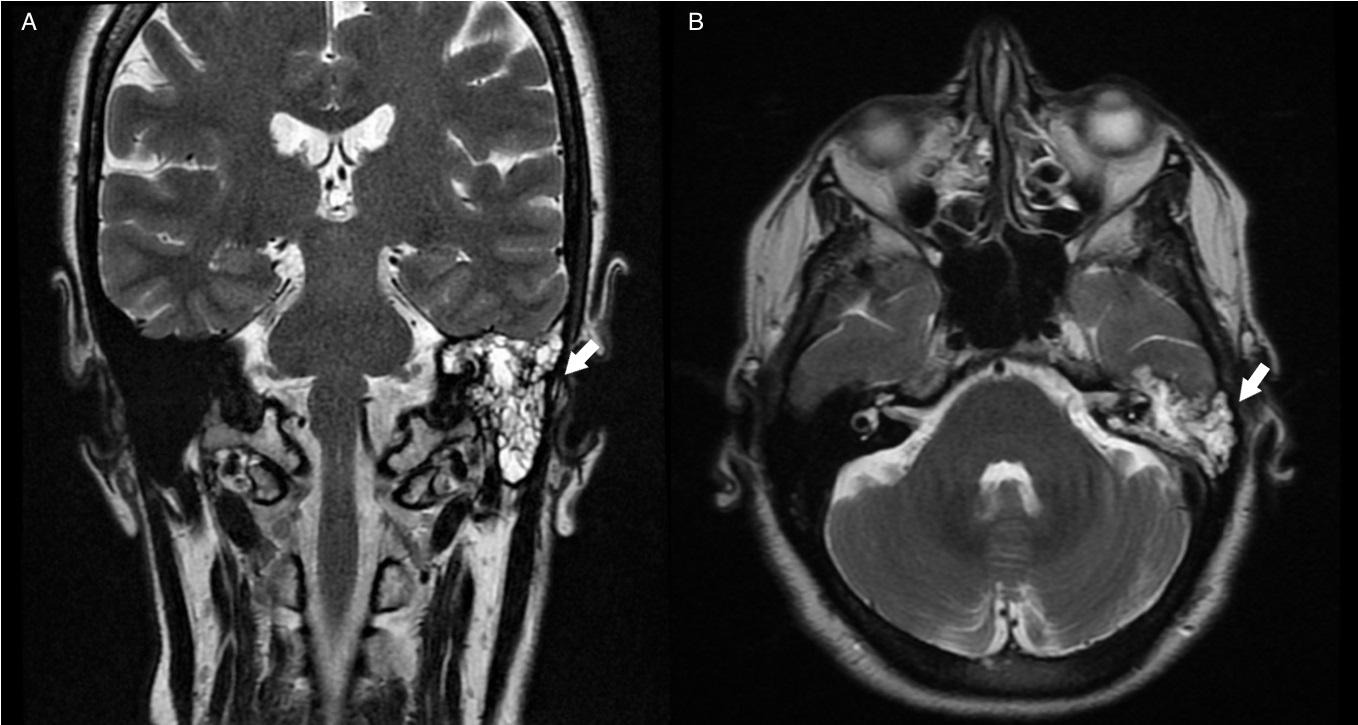
A 57-year-old Caucasian, Portuguese woman, without risk factors or relevant medical history, presented with pansinusitis, foul-smelling nasal secretions and crusts. The patient denied recent travel and had no contact with or risk factors for tuberculosis infection. After a biopsy result of nasal granulomas, she was diagnosed with anti-neutrophil cytoplasmic antibody (ANCA)-negative granulomatosis with polyangiitis (GPA) in 2010. Consequently, treatment with prednisolone and azathioprine was initiated. Over the course of 7 years, she presented progressive unilateral hypoacusis. Complementary studies, namely MRI, showed a mass originating in the left tympanic cavity extending into the posterior Eustachian tube, epitympanic recess and into the aditus ad antrum surrounding the auditory ossicles (Fig. 1). The biopsy of the lesion was positive for acid-fast bacilli and the patient started quadruple anti-tuberculous therapy (isoniazid, rifampin, pyrazinamide and ethambutol) and was weaned off the immunosuppressants. Soon afterwards, remission of the mass and symptoms was noted.
Figure 1. Coronal (A) and axial (B) MRI showing a mass in the left tympanic cavity (arrows)
DISCUSSION
Tuberculous otomastoiditis is a rare entity, representing a diagnostic and therapeutic challenge. It is more frequently seen in countries endemic for tuberculosis. Infection may be primary (mucus aspirated through the Eustachian tube or neonates who have aspirated infected amniotic fluid) or secondary (organisms may secondarily infect the nasopharynx when expectorated from the lung) and, less frequently, caused by haematogenous spread. Chronic otorrhoea and hearing loss are common symptoms. Preauricular or anterior cervical lymphadenopathy and facial nerve paralysis occur infrequently. Diagnosis is made by direct culture of Mycobacterium tuberculosis or molecular techniques from the local discharge or a biopsy sample. In our case, after the MRI showed a mass originating in the left tympanic cavity, there was a high suspicion of tuberculous otomastoiditis [1,2].
Although otorhinolaryngological forms of GPA may be ANCA-negative, the lack of evidence of localized or systemic vasculitis raised questions about the initial diagnosis and its auto-immune origin. It is possible that an indolent tuberculous process evolved to an exuberant growth under immunosuppressive therapy, causing unilateral hearing loss. The diagnosis of extrapulmonary forms of tuberculosis is often delayed and requires high clinical suspicion. This case reinforces our belief that it is essential to build a comprehensive differential diagnosis list, especially for patients where immunological studies are negative or inconclusive or there are doubts about the diagnosis. The finding of nasal granulomas is not exclusive to auto-immune disease and a comprehensive investigation of the aetiology (inflammatory, infectious, neoplasm, drugs) is mandatory. Due to the significant incidence of tuberculosis in Portugal, the presence of nasal granulomas makes the exclusion of tuberculosis imperative, and even more so if treatment encompasses a decision to start immunosuppressive therapy, as this may reactivate a latent infection. Therefore, this case highlights the importance of screening for latent tuberculosis before starting immunosuppressants, which may avoid further complications.