ABSTRACT
Pericardial effusion has a broad spectrum of clinical presentation, ranging from an incidental finding on imaging to a potentially fatal emergency such as pericardial tamponade, the most severe presentation. The authors present a case of a middle-aged male hospitalized due to shortness of breath. Initial work-up was positive for massive pericardial effusion with haemodynamic compromise. Additional study revealed panhypopituitarism. The acromegalic phenotype was suggestive of acromegaly secondary to pituitary adenoma, which had probably evolved to apoplexy. Hormone replacement was started with clinical improvement. At the 3-year follow-up, there was no evidence of recurrence of pericardial effusion. Panhypopituitarism is a relatively rare entity, but can lead to life-threatening complications such as adrenal crisis, coma and myxoedema-associated cardiac failure. Pericardial effusion is an extremely rare manifestation of secondary hypothyroidism.
LEARNING POINTS
- To recognize the clinical presentation of cardiac tamponade.
- To recognize atypical causes of pericardial effusion, such as severe panhypopituitarism.
- Hormonal replacement is efficient in treating panhypopituitarism.
KEYWORDS
Pericardial effusion, pericardiocentesis, panhypopituitarism
INTRODUCTION
Pericardial effusion has a broad spectrum of clinical presentation, ranging from an incidental finding on imaging to a potentially fatal emergency such as pericardial tamponade. The causes are numerous and vary according to the geographical area and clinical context of the patient. They can be divided into 2 groups: inflammatory (infections due to viruses, bacteria and mycobacteria, cardiac injury, autoimmune syndromes, urea, drug hypersensitivity) and non-inflammatory (primary or secondary, metabolic, traumatic or reduced lymphatic drainage). Pericardial tamponade is the most severe presentation and results from haemodynamic compromise imposed by the reduction of pericardial compliance to the right ventricular cavity and reduction of left ventricular filling resulting from interventricular interdependence. Echocardiography is the examination modality of choice for diagnosis and allows characterization of pericardial effusion based on size, location and haemodynamic status. Treatment, if necessary, is directed to the underlying disease. In the presence of cardiac tamponade, emergent pericardiocentesis, accompanied by haemodynamic resuscitation, is mandatory[1,2].Pericardial effusion may occur in cases of severe hypothyroidism, most often in cases of primary hypothyroidism due to the influence of elevated thyroid-stimulating hormone on the pathophysiology of the effusion, and therefore, it is rare in cases of central hypothyroidism[3].In the literature, there are only a few cases reporting pericardial effusion as a presenting finding in the diagnosis of central hypothyroidism.
CASE DESCRIPTION
A 63-year-old man with a history of hypertension, hypercholesterolaemia, chronic anaemia, left lacunar cerebral ischaemic infarction without sequelae, was hospitalized due to a 1-week clinical picture of shortness of breath.He also reported involuntary weight loss of approximately 10 kg over the previous 6 months.
On physical examination, he was alert, asthenic, with marked mucocutaneous pallor, an acromegalic phenotype and thinning hair, apyretic, haemodynamically stable (blood pressure 109/69 mmHg, heart rate 85 bpm), eupnoeic in room air, without venous jugular engorgement, but with decreased heart sounds and decreased vesicular murmur in the pulmonary bases bilaterally on auscultation.
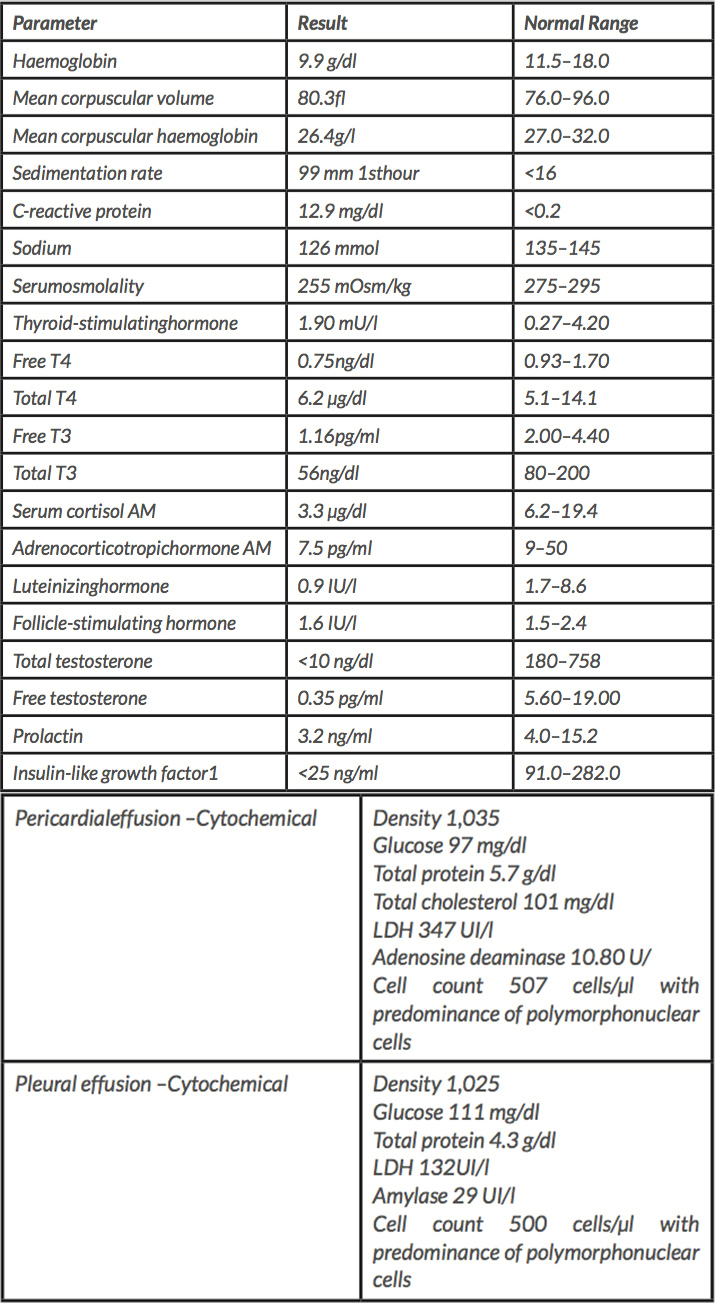
Analytical tests revealed normochromic, normocytic anaemia, elevation of inflammatory parameters and hypo-osmolal hyponatraemia (Table 1). Infectious, autoimmune and serological studies were negative.
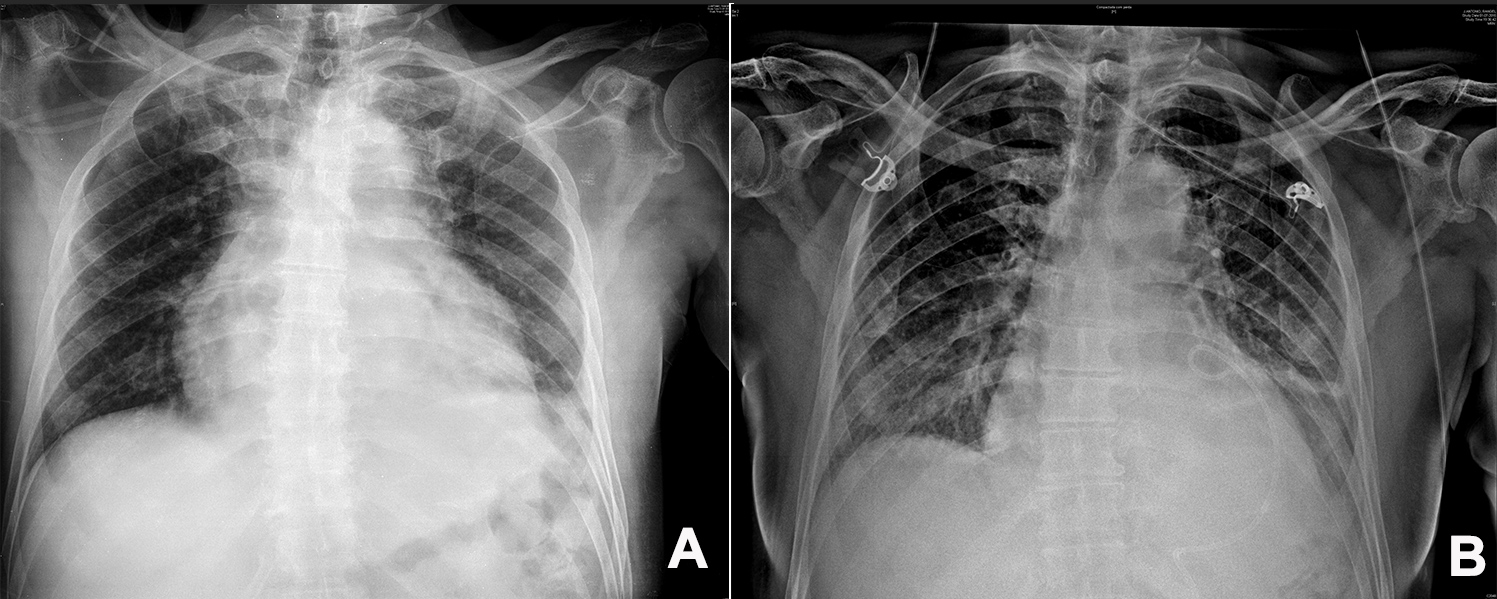
An electrocardiogram showed low-voltage QRS complexes and a chest x-ray presented an increased cardiac silhouette and bilateral pleural effusion (Fig.1A).
Figure 1. (A) Chest x-ray at diagnosis showing an increased cardiac silhouette and bilateral pleural effusion. (B) Chest x-ray after pericardiocentesis, with a pigtail catheter placed in the pericardial space
Table 1. Laboratory results
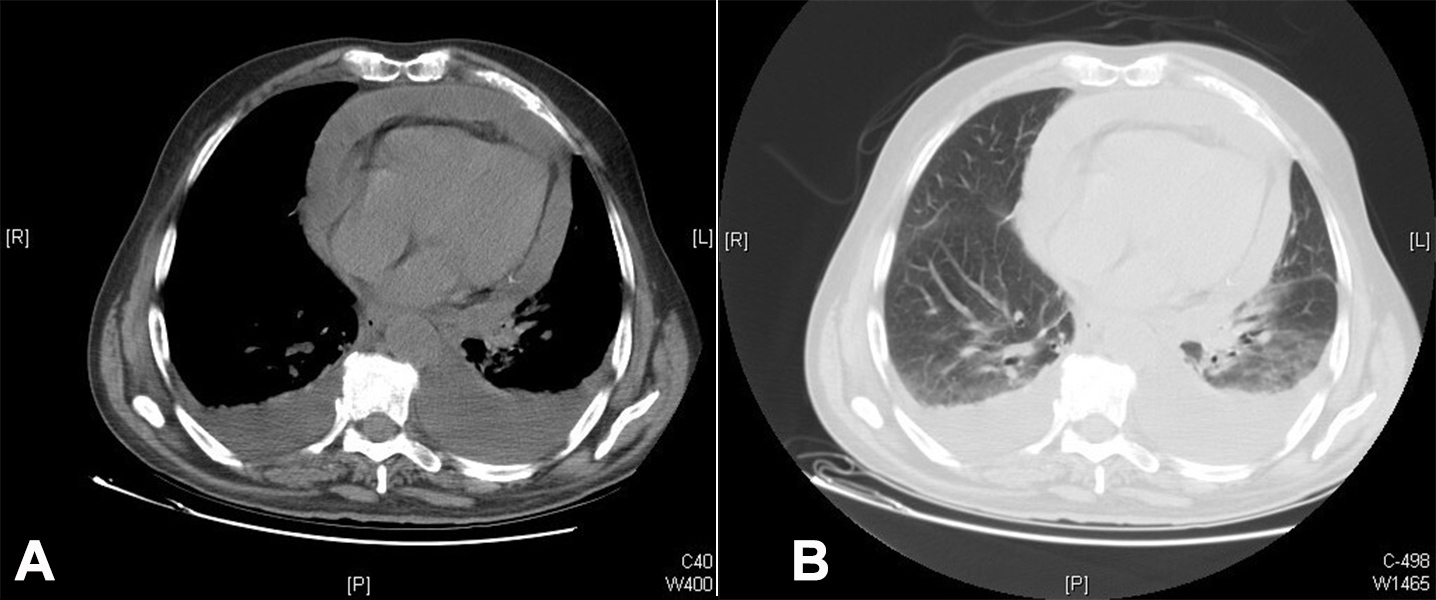
Thoraco-abdomino-pelvic computed tomography revealed the presence of a large pericardial effusion (approximately 25 mm in diameter) associated with bilateral pleural effusion (Fig. 2).
Figure 2. Thoraco-abdomino-pelvic computed tomography revealed the presence of a large pericardial effusion (approximately 25 mm in diameter) associated with bilateral pleural effusion (A: normal window, B: pulmonary window)
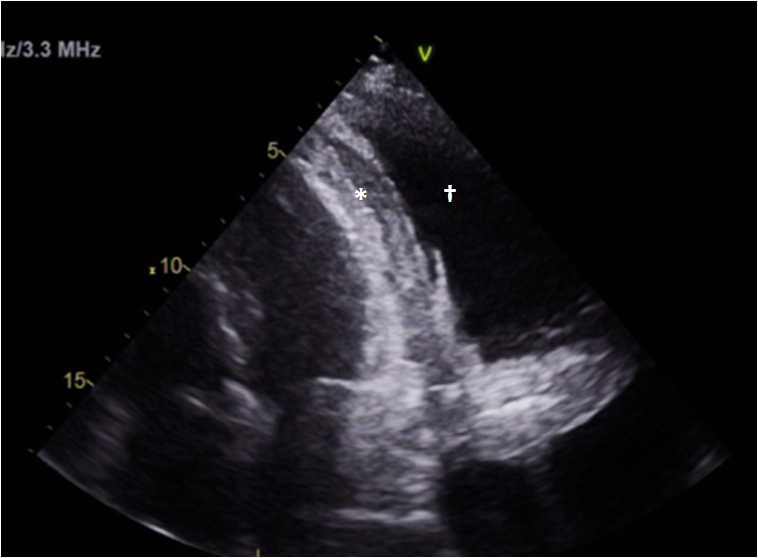
Transthoracic echocardiography confirmed massive pericardial effusion (Fig. 3), with abundant fibrin and haemodynamic compromise, impaired right ventricular filling, but with good biventricular function. Pericardiocentesis was performed with drainage of serohaematic pericardial fluid and thoracentesis with fibrinous citrus-yellow fluid (Fig. 1B).
Figure 3. Transthoracic echocardiography: massive pericardial effusion (*) and pleural effusion (†)
Cytochemical examinations of both the pericardial and pleural fluids were compatible with exudate (Table 1); bacteriological and mycobacteriological cultures were negative. Pleural biopsy showed signs of chronic inflammation, without granulomas or cellular atypia.
In the context of the aetiological study of hyponatraemia, panhypopituitarism was diagnosed: secondary hypothyroidism, secondary hypocortisolism, hypogonadotropic hypogonadism, hypoprolactinaemia and decreased insulin-like growth factor 1.
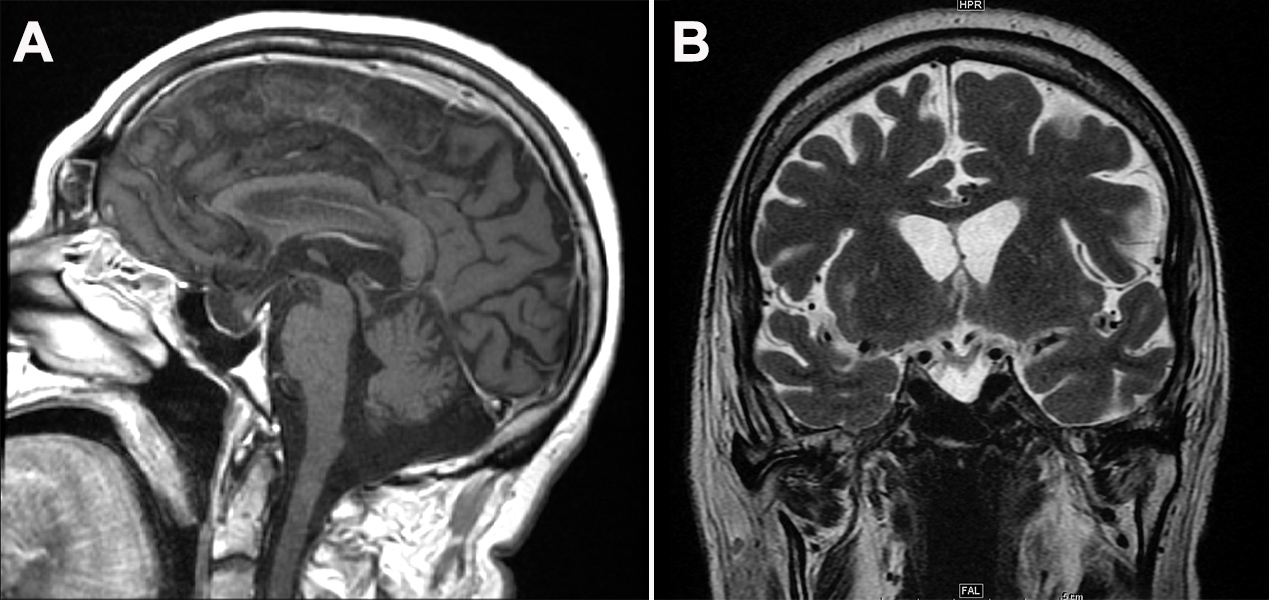
Magnetic resonance imaging of the sellarregion showed features compatible with a partially empty sella with increased dimensions, and persistence of the posterior pituitary gland (Fig. 4).
Figure 4. Magnetic resonance imaging: a partially empty sella with increased dimensions, and persistence of the posterior pituitary gland
DISCUSSION
Panhypopituitarism is a relatively rare entity (incidence of 2.07–4.2 cases per 100,000 people/year and a prevalence of 37.5–45.5 cases per 100,000 people), with no variation by sex[4,5].The causes are various, the most common being pituitary tumoural lesions (macroadenomas, cysts, metastases) followed by pituitary surgery or radiotherapy. Clinical manifestation is variable and dependent on the degree of onset, the number and type of pituitary hormones affected and the degree of hormonal insufficiency[5]. In addition to symptoms of endocrine dysfunction, patients may have symptoms associated with the underlying process[4].
The main cardiovascular manifestations are sinus bradycardia, left ventricular dysfunction, decompensated heart failure, dilated cardiomyopathy, conduction anomalies (prolonged QT, ventricular arrhythmias), mitral valve prolapse and pericardial effusion. Panhypopituitarism can lead to life-threatening complications such as adrenal crisis, coma and myxoedema-associated cardiac failure[3,6,7].
Pericardial effusion is an extremely rare manifestation of central hypothyroidism. Pericardial effusion formation is due to glycosaminoglycan deposition, protein extravasation secondary to increased capillary permeability, impaired lymphatic drainage coupled with sodium and water retention[3,7]. This case report involves an atypical presentation of panhypopituitarism with massive pericardial effusion. From his previous history, the patient had an acromegalic morphotype with several years of evolution, suggestive of a functioning pituitary adenoma, potentially complicated by asymptomatic pituitary apoplexy translated by the findings of a partially empty sella. Following pericardiocentesis and hormone replacement, there was a progressive improvement of the general condition. At the 3-year follow-up, there was no evidence of recurrence of pericardial effusion.