ABSTRACT
Sarcoidosis is a chronic multisystemic inflammatory disease of unknown aetiology. Virtually any organ or system can be involved, resulting in a wide range of clinical presentation. Pleural sarcoidosis is rare. Pleural effusion can only be attributed to pleural sarcoidosis in the presence of pleural non-caseating epithelioid granulomas and after excluding other granulomatous diseases. Anthracosis is a pneumoconiosis associated with thoracic adenopathies and bronchial disease, and it is usually asymptomatic. The authors present a case of a middle-aged man hospitalized due to cough, right-sided pleuritic chest pain and trepopnoea.
LEARNING POINTS
- To pursue a systematic and exhaustive investigation of pleuraleffusion until a definitive diagnosis is established.
- To recognize atypical presentations of sarcoidosis with a high degree of suspicion whenever the initial investigation is inconclusive.
KEYWORDS
Pleural effusion, pleural sarcoidosis, anthracosis, exhaustive investigation
INTRODUCTION
Sarcoidosis is a chronic multisystemic inflammatory disease of unknown aetiology. Diagnosis is based on clinical and radiological findings supported by the histological presence of non-caseous granulomas. Virtually any organ or system can be involved, resulting in a wide range of clinical presentation[1]. Anthracosis is a pneumoconiosis associated with thoracic adenopathies and bronchial disease, diagnosed by bronchoscopy and confirmed by histological analysis[2].
CASE DESCRIPTION
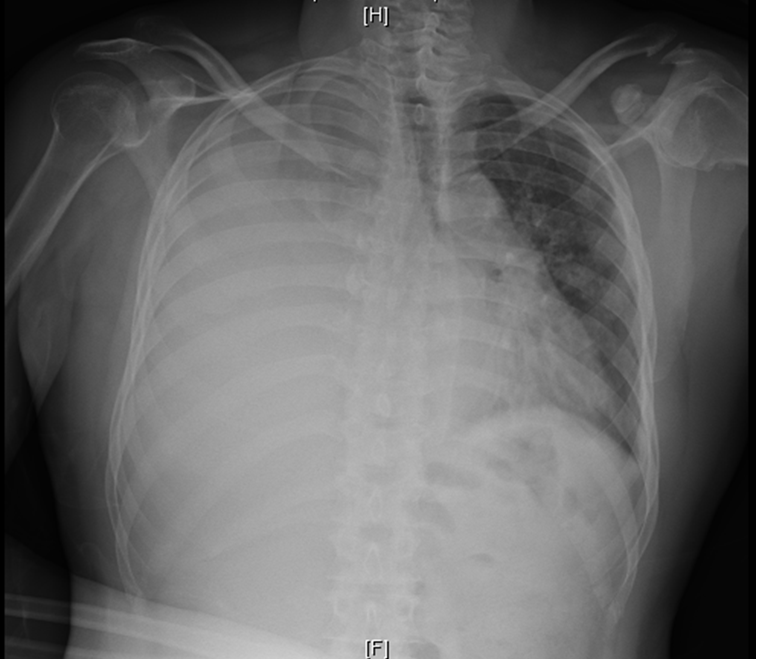
A 49-year-old black man with a past medical history of hypertension presented with a 2-week history of cough, right-sided pleuritic chest pain and trepopnoea. He had occupational exposure to dust as a construction worker, with no other hazardous environmental exposure or smoking history. On examination, he was afebrile and tachypnoeic with reduced air entry, absent vocal fremitus and dullness on percussion on the right hemithorax. Arterial blood gas assessment revealed type I respiratory failure. A chest radiograph showed a large right-sided pleural effusion (PE) (Fig.1).
Blood analysis showed a normocytic anaemia, an elevated erythrocyte sedimentation rate (ESR; 117mm/h), normal calcium and angiotensin-converting enzyme levels. Thoracocentesis revealed a paucicellular yellow fluid biochemically compatible with an exudate. A transthoracic echocardiogram was unremarkable.
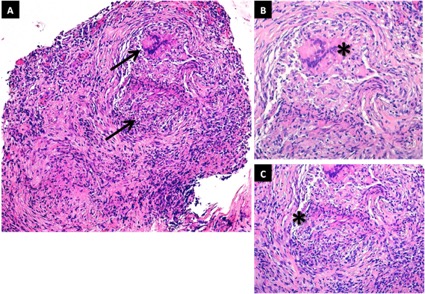
Chest computerized tomography (CT) confirmed the large right-sided PE and revealed multiple bilateral hilar and mediastinal adenopathies. Pleural biopsy identified the presence of non-caseating epithelioid granulomatosis compatible with pleural sarcoidosis (Fig. 2).
Figure 1. A chest radiograph showing a large right-sided pleural effusion
Figure 2. Parietal pleural biopsy showing multiple well-formed non-caseating granulomas (arrows and asterisks) with tight epithelioid cells and multinucleated giant cells. Haematoxylin and eosin stain, x10 (A) and x20 (B and C)
Flexible bronchoscopy revealed normal bronchial mucosa and echoendoscopy confirmed the presence of multiple hypoechoic mediastinal adenopathies. Histological analysis showed lymphatic tissue with marked sinus histiocytosis and histiocytes with abundant anthracosis pigment. Overall, the study excluded infective, tumoral or auto-immune conditions.
Based on the above-mentioned results, the diagnosis of pleural sarcoidosis associated with lymphatic anthracosis was established. Due to relapse of the PE and symptomatic deterioration,the patient was started on prednisolone 40 mg once-daily with resolution of the effusion. To assess disease activity, he underwent a positron emission tomography scan, while already under steroid therapy, which demonstrated mild inflammatory activity within multiple lymph nodes compatible with the diagnosis.
DISCUSSION
Pleural sarcoidosis is a rare condition (estimated prevalence of 1–4%) presenting with thickening, nodules, PE, pneumothorax, hydropneumothorax and trapped lung. It affects both sexesequally and all age groups (more common between 41–60 years of age). Approximately two-thirds of patients are asymptomatic. Respiratory symptoms are the most common (33–50%) followed by constitutional symptoms (33%) [1, 3, 4, 5].
PE can be the initial presentation of pleural sarcoidosis or it can develop at a later stage. The characteristics of the pleural fluid can often be correlated with the underlying pathological alterations caused by sarcoidosis. The inflammatory response to the granulomas causes an increase in capillary permeability, resulting in an exudative effusion. A transudate may arise from heart failure, endobronchial sarcoidosis (causing trapped lung, bronchial stenosis and/or atelectasis) and superior vena cava obstruction. Chylothorax may arise as a result of thoracic duct or lymphatic obstruction. Pleural vasculature compression or erosion by granulomas may lead to a haemothorax [4, 5].
Pleural sarcoidosis may result in bilateral or unilateral PE (right-sided more frequent). Most cases produce small to moderate effusions. Large effusions are rare. Cytochemical analysis tends to show a paucicellular exudate with lymphocyte prevalence with a CD4+/CD8+ ratio of 1/1.33 and elevated protein content [5, 6]. A definitive diagnosis is made by the histological documentation of non-caseous granulomas as well as the exclusion of other granulomatous conditions[4].
Small effusions often remit spontaneously within 1–3 months[7]. Steroid therapy is indicated for a large PE, symptomatic relief or effusion relapse. Patients tend to respond to steroids alone or in combination with hydroxychloroquine[5]. Those who do not respond may need pleurodesis or surgical decortication. The prognosis is favourable with complete effusion resolution [7, 8].
Anthracosis is a pneumoconiosis of unknown aetiology but is associated with lung accumulation of coal dust or other small particles[2].
The main known risk factors are exposure to biomass fumes, coal dust and other minerals. Clinical presentation is similar to other forms of pneumoconiosis. Mediastinal adenopathy can cause compression and paralysis of the vocal cords or broncholithiasis. Anthracosis can be unilateral or bilateral and the right middle lobe tends to be the most affected. A chest radiograph can look normal or may reveal heterogeneous infiltrates, subsegmental atelectasis or solid lesions. Thoracic CT shows the presence of hilar and/or mediastinal adenopathies (94%) and bronchial wall thickening with or without atelectasis. The pleura is affected in 25% of patients[9].
Definitive diagnosis is through histological sampling via bronchoscopy. This can reveal 3 distinct patterns: superficial black discolouration; scattered foci or black spots with inward mucosal retraction as a result of adjacent anthracotic lymphadenopathy and bronchial anthracofibrosis which may occur with tightening, distortion and occlusion of the bronchial lumen. Endobronchial ultrasound is not yet extensively used; however, it may show the presence of a scattered nodular hypoechoic pattern in the subepithelial area of the bronchus or lymph nodes adjacent to the bronchial mucosa. Anthracosis has no specific therapeutic approach. Management tends to be conservative and directed to symptomatic control. Endobronchial stenting may be required in cases of significant bronchial stenosis [2, 9].
This case describes an unusual occurrence of pleural sarcoidosis and lymphatic anthracosis in a patient presenting with a history of dyspnoea, pleuritic chest pain and a large right-sided PE. There was no relapse of either the symptoms or effusion upon cessation of steroid therapy, which is consistent with the benign course of sarcoidosis and anthracosis. Regarding the anthracosis, it is important to take this into account on patient follow-up due to the risk of bronchial disease onset and its complications.
CONCLUSION
The aetiological investigation of PE should be systematic and exhaustive. Pleural involvement in sarcoidosis is extremely rare, and therefore, a high degree of suspicion is needed, especially in the absence of findings suggestive of pulmonary sarcoidosis. This diagnosis should be suspected whenever the initial investigation is inconclusive. Anthracosis manifests in the presence of endobronchial disease or complications associated with mediastinal adenopathy.