ABSTRACT
Oesophageal varices are a dilated submucosal venous plexus in the lower third of the oesophagus which result from increased pressure in the portal venous system. The portal system is connected to the systemic circulation in specific locations referred to as sites of portosystemic anastomosis. An increase in portal venous pressure is therefore reflected at these anastomotic sites, causing manifestations such as oesophageal varices, rectal varices, caput medusae and splenorenal shunts. Varices do not cause symptoms until they leak or rupture and this is the main complication which requires prompt treatment. Here, we present a post-liver transplant patient with metastatic hepatocellular carcinoma who had oesophageal varices that fistularized with a left pulmonary vein, thus creating a right-to-left shunt. Right-to-left shunts are usually intracardiac or intrapulmonary in location. The complications of a right-to-left shunt include predominantly hypoxia, cyanosis and, sometimes, paradoxical emboli in the case of intracardiac shunts. This patient had a very uncommon cause of such a shunt caused by a direct fistulous connection.
LEARNING POINTS
- Right-to-left shunts create a ventilation-perfusion mismatch.
- Recognizing situations where there is a connection between the systemic circulation and pulmonary circulation without intermediate oxygenation is important because of possible clinical implications such as hypoxia.
KEYWORDS
Right-to-left shunt, oesophageal varices
CASE DESCRIPTION
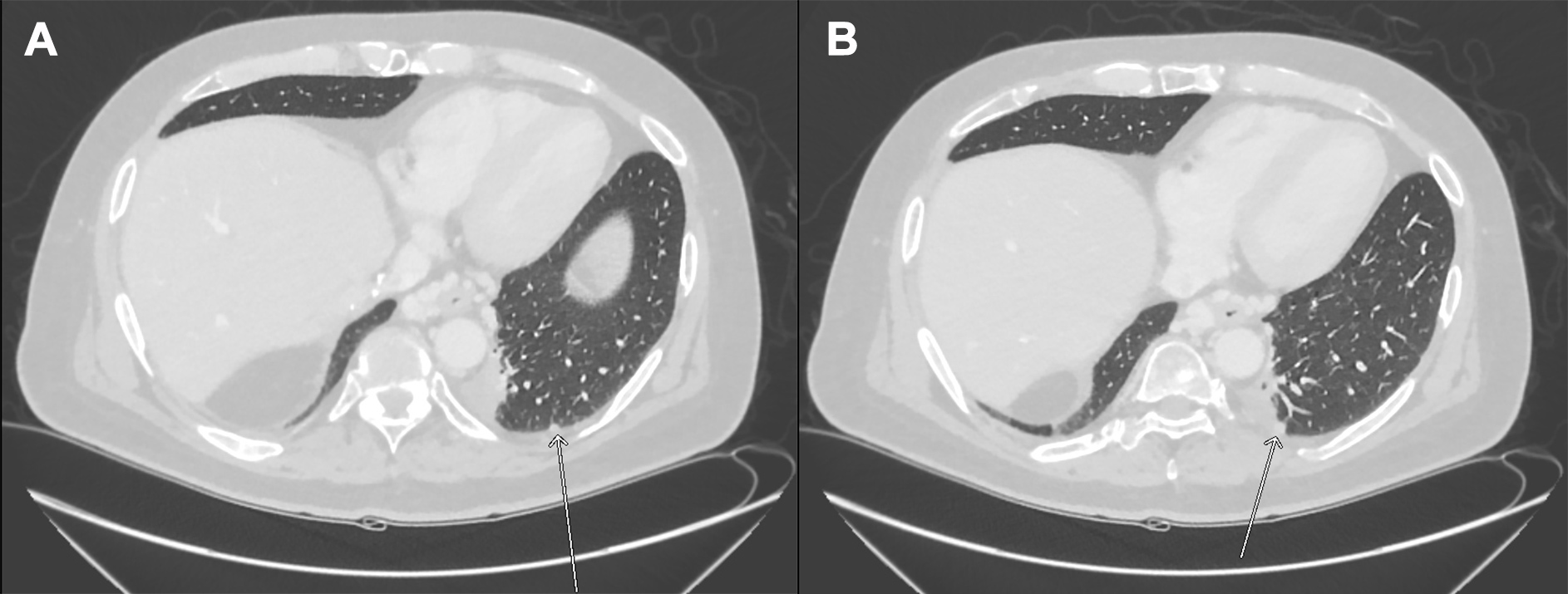
We present a case of a 64-year-old male who had a liver transplant in 2013 for hepatitis C virus (HCV) and hepatocellular cancer (HCC) which was complicated by HCC recurrence with metastasis. He was noted to have metastatic lung lesions post-transplant for which he underwent a surgical resection followed by stereotactic radiation. He received treatment for HCV with Harvoni for 12 weeks followed by Harvoni/ribavirin for 24 weeks with sustained viraemia. However, he had stable liver function tests, and in view of his metastatic cancer and concurrent therapy for the same, he was not started on antiviral agents. He was also on immunosuppressive medication. For his metastatic HCC, he was started on palliative therapy with sorafenib in April 2016, which he continued until March 2018. At this time, imaging results showed definite evidence of disease progression. The patient had metastatic disease in the lungs bilaterally and in several lymph nodes. He was subsequently started on second-line regorafenib. During routine surveillance imaging in August 2018, he was noted to have an incidental finding of a fistula between his oesophageal varices and the left pulmonary vein (Fig. 1). This created a right-to-left shunt. However, the patient had no symptoms as a result of this shunt and has continued maintenance therapy with regorafenib and remains a follow-up outpatient with Oncology as well as Hepatology.
DISCUSSION
Right-to-left shunts refer to a situation where there is an abnormal connection between the systemic and pulmonary circulation without intermediate oxygenation of the blood in the lungs. This can be due to anatomic or physiologic causes[1,2]. Anatomic shunts occur when the alveoli are completely bypassed as in the case of intracardiac shunts or intrapulmonary arteriovenous malformations. Physiologic shunts refer to a scenario where there is perfusion of non-ventilated alveoli as in the case of atelectasis, ARDS and so on. This creates a ventilation-perfusion mismatch. If the shunt is significant, it can result in hypoxia. Pulmonary manifestations of liver disease include hepatopulmonary syndrome, portopulmonary hypertension and hepatic hydrothorax[1].
Hepatopulmonary syndrome is the most common of these and is a special variant of a right-to-left shunt. The pathophysiology behind this is not fully understood but is associated with intrapulmonary vascular dilatations and arteriovenous connections. These are more common in the bases of the lungs and postulated to be secondary to the action of vasoactive mediators such as nitric oxide stimulated by bacterial translocation, and an inability of the liver to clear pulmonary vasodilators[3]. This clinically results in dyspnoea and hypoxia. Classically, hepatopulmonary syndrome is associated with platypnoea and orthodeoxia. Platypnoea refers to increased dyspnoea when moving from a recumbent to an upright position, which is contrary to the much more common orthopnoea seen in patients with congestive heart failure. Orthodeoxia refers to a decrease in oxygen tension when moving from a supine to an upright position[1,3].
Our patient did not have any clinical manifestations as a result of the anatomic shunt that was detected. In addition, he did not have any underlying pulmonary hypertension or hepatopulmonary syndrome. This is probably because the volume of blood being shunted was minimal and not adequate to cause symptoms. Hence, he did not need any intervention. Hypothetically, however, a variceal-pulmonary venous fistula could become significant in a patient with hepatopulmonary manifestations as a result of native/transplanted liver cirrhosis and could necessitate an intervention to obliterate the fistula[4,5].
Atrio-oesophageal fistulas after procedures such as atrial fibrillation ablation, a broncho-oesophageal fistula as a complication after sclerotherapy and arterioportal fistulas causing oesophageal varices have all been documented in several case reports[6]. However, a fistula between oesophageal varices and the pulmonary vein has, to the best of our knowledge, not been reported before. In the right clinical setting, the presence of such a fistula could have clinical relevance and also require treatment.