ABSTRACT
Pulmonary hypoplasia or agenesis is a rare congenital disorder that results in lung underdevelopment. This disease is usually found in children but rarely encountered in adults. We describe the case of an 84-year-old woman diagnosed with a unilateral pulmonary hypoplasia presenting simultaneously with left pulmonary artery hypoplasia. Due to this condition, the patient had a lifelong history of pulmonary infections that resulted in several bronchiectases in the affected lung. Moreover, the pulmonary artery hypoplasia led to the development of pulmonary hypertension and collateral circulation causing hemoptysis, giving rise to the patient attending the emergency department. Although we were able to medically manage the hemoptysis, it can be fatal and require surgical intervention. Hence, an early diagnosis is essential so that appropriate follow-up and prompt prevention and treatment of complications, such as pulmonary infections, hemoptysis and pulmonary hypertension, are achieved.
LEARNING POINTS
- Although rare and typically associated with childhood, lung and pulmonary artery hypoplasia can in exceptional cases be present in adult life.
- The diagnosis of lung and pulmonary artery hypoplasia is challenging in adults as they can easily be mistaken for more common diseases.
- Symptoms and complications may be life-threatening, including dyspnea, hemoptysis, recurrent pulmonary infections and pulmonary hypertension.
- An early diagnosis is extremely important because it allows a close follow- up with consequent timely detection and treatment of serious complications, especially pulmonary hypertension.
KEYWORDS
Radiology, respiratory medicine, congenital disorders, lung hypoplasia, pulmonary artery agenesis, pulmonary artery hypoplasia, hemoptysis
INTRODUCTION
Pulmonary hypoplasia or agenesis is a rare congenital disorder that can range from partial to almost complete lung underdevelopment. It can be unilateral or bilateral and in 1955 was classified by Boyden into three categories: pulmonary agenesis, in which there is complete absence of the lung, bronchus and blood vessels of the affected site; pulmonary aplasia, in which a rudimentary bronchus is present without any lung tissue; and pulmonary hypoplasia, in which a variable amount of lung parenchyma, bronchial tree and supporting vasculature is present [1, 2]. According to the etiologic factors, pulmonary hypoplasia is divided into primary and secondary. The latter is usually associated with variable fetal or maternal abnormalities (60%), space-occupying lesions in the chest, development anomalies of the chest wall as well as urogenital and neuromuscular diseases[3]. Primary pulmonary hypoplasia is rare and, though no apparent cause is implicated in its pathogenesis, can be caused by an accident in utero or an embryologic defect of the lung or vascular tissue, such as unilateral absence of the pulmonary artery. Considering that these are early errors of development, whether they are the cause, effect or an association is still unknown [4].
We describe a rare case of unilateral pulmonary hypoplasia presenting simultaneously with left pulmonary artery hypoplasia in an 84-year-old patient. This condition led to the development of pulmonary hypertension and collateral circulation causing hemoptysis.
CASE DESCRIPTION
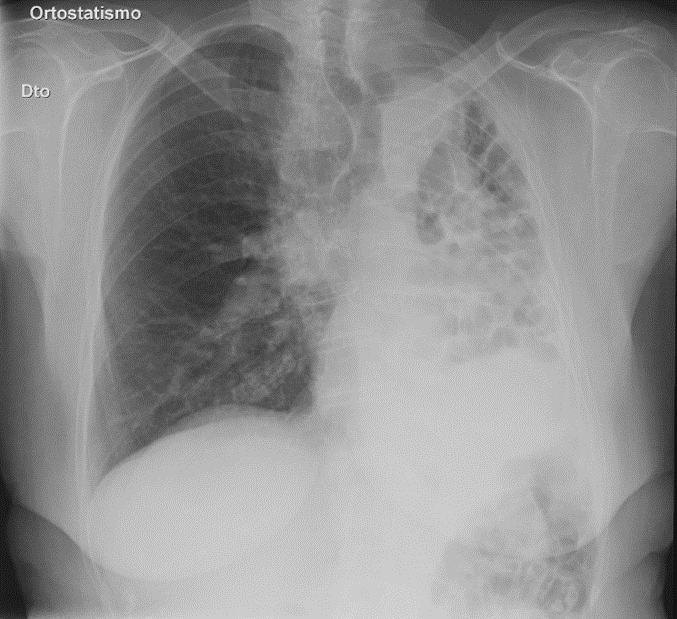
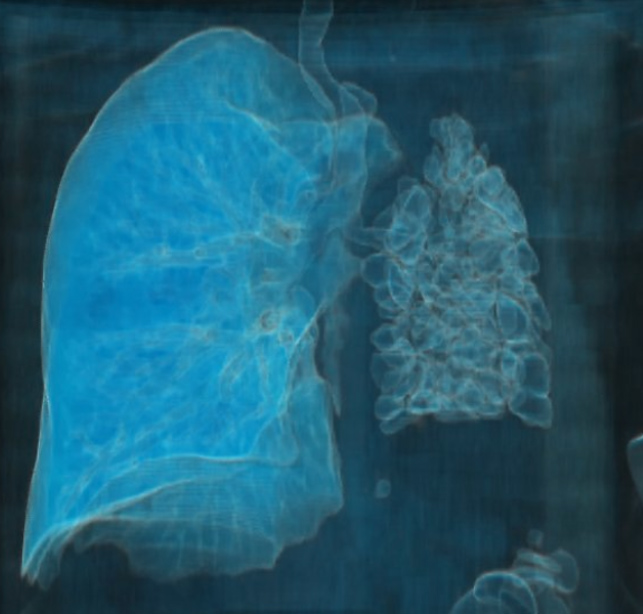
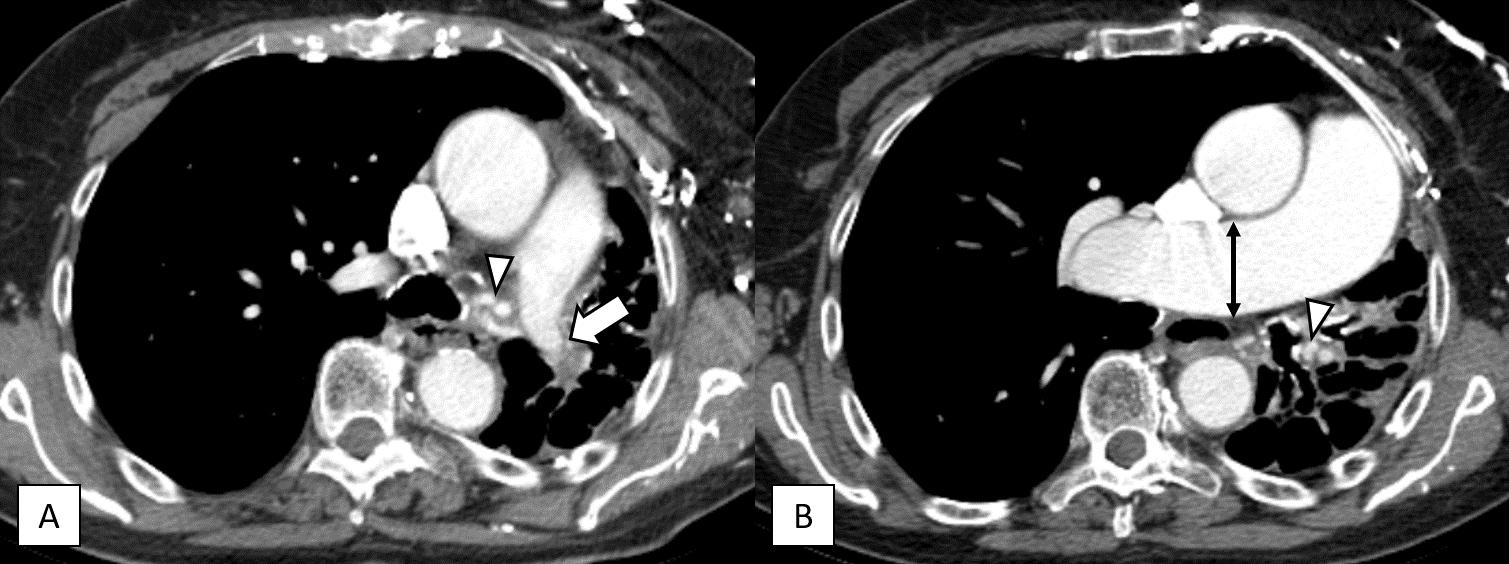
We present the case of an 84-year-old female with no signs of congenital cardiac anomalies in a previous transthoracic echocardiogram and with a history of lung disease (unspecified by her) diagnosed during infancy, with no follow-up. She mentioned having frequent respiratory tract infections, usually associated with hemoptysis and denied ever having been infected with tuberculosis (though previously tested) or having a family history of lung diseases. She presented to the emergency department (ED) with a 3 week history of productive cough, complicated by hemoptysis in the previous 2 days. There was no evidence of chest pain, fever, night sweats, weight loss, recent travel or contact with sick people. In the ED she was apyretic and hemodynamically stable. Physical examination revealed diminished breath sounds on the left hemithorax with diffuse crackles. Blood tests showed leukocytosis and increased C-reactive protein levels. A posteroanterior chest X-ray (Fig. 1 ) showed mediastinal shift to the left, with hyperinflation of the right lung as well as an asymmetrically smaller left lung, with multiple cystic areas. Further imaging evaluation with chest computed tomography (CT) revealed narrowing of the left pulmonary artery with a few small branches and a small hypoplastic left lung filled with multiple cystic bronchiectases (Figs. 2, 3, 4A). There was also ectasia of the main pulmonary trunk and right pulmonary artery as well as hypertrophy of bronchial arteries, indicating pulmonary hypertension (Fig. 4B). A mild cardiomegaly was noted but no cardiac anomalies were detected. Culture (Löwenstein–Jensen and Mycobacterium Growth Indicator Tube) and smear of sputum for acid-fast bacilli failed to reveal any sign of Mycobacterium tuberculosis. However, microbiological analysis of the sputum showed the presence of Pseudomonas aeruginosa. In light of the typical clinical history, including the diagnosis of a pulmonary disease in infancy, along with the characteristic findings in the CT scan, the diagnosis of a congenital disease (lung hypoplasia associated with pulmonary artery hypoplasia) exacerbated by a respiratory infection was made. The patient was admitted to the medical ward and started on antibiotic therapy (levofloxacin) as well as aminocaproic acid, with clinical improvement and without hemoptysis recurrence. She was then discharged and continued follow-up on an outpatient basis. She has been asymptomatic for the last 12 months, with no directed therapy.
Figure 1. Chest X-ray showing a cardiomediastinal silhouette shift to the left, with hyperinflation of the right lung. The left lung is asymmetrically smaller, with multiple cystic areas
Figure 2. CT scan image in lung window showing a left mediastinal shift with hyperinflation and expansion of the right lung. The left lung is almost entirely hypoplastic with multiple dilated bronchi with cystic morphology
Figure 3. 3D lung reconstruction showing right lung hyperinflation and left hypoplastic lung with multiple bronchiectases
Figure 4. CT scan images in mediastinal window showing (A) hypoplastic left pulmonary artery (arrow); (B) pulmonary trunk and right pulmonary artery (double head arrow) are markedly dilated, indicating pulmonary hypertension. Note also the hypertrophied bronchial arteries (arrowheads)
DISCUSSION
Unilateral pulmonary hypoplasia or agenesis has a prevalence of 1–2 per 12,000 births and in 70% of cases it affects the left lung [2] This disease is usually found in children but rarely encountered in adults. Cases of long survival in adulthood are usually seen in primary lung hypoplasia, due to the absence of associated embryological pathology, and explained by compensatory hypertrophy of the contralateral lung. This is better accomplished by the right lung (three lobes), explaining the best survival odds of patients with left lung underdevelopment [1,5].
Adult diagnosis is especially challenging due to nonspecific symptoms, which are similar to more ominously acquired diseases. Their clinical presentation is highly variable, ranging from asymptomatic patients to cases of repeated pulmonary infections. The latter are due to alveolar tissue underdevelopment leading to a small fibrotic and non-functioning lung with associated surfactant deficiency and impaired mucociliary clearance, which increases host susceptibility to bacterial and viral proliferation [5]. This occurred in our patient’s case, in whom we believe that frequent pulmonary infections (since infancy) led to the development of multiple bronchiectases in the hypoplastic lung, resulting in a radiographic image of a cystic lung. Our patient also had left pulmonary artery hypoplasia, which resulted in redirection of blood flow toward the normal pulmonary artery (right), leading to the development of pulmonary hypertension. This was also responsible for an increased collateral circulation through the bronchial arteries. The presence of cystic bronchiectasis and hypertrophied bronchial arteries has been proposed as the probable cause for the development of hemoptysis, a less frequent symptom that brought our patient to ED.
In this case, the main differential diagnoses are congenital pulmonary airway malformation (CPAM) and Swyer–James–MacLeod syndrome (SJMS). CPAM is a congenital lung disease characterized by a multicystic mass of pulmonary tissue, which commonly presents with recurrent pulmonary infections [1]. The radiographic cystic appearance of our patient’s lung could raise the suspicion of this disease; however, usually CPAM is neither associated with bronchiectasis nor the arterial anomalies described. SJMS is a rare entity associated with post-infectious bronchiolitis obliterans occurring in childhood. Although it can present with pulmonary artery hypoplasia, bronchiectasis and unilateral loss of lung volume (all detected in our patient), it is characterized by a hyperlucent lobe or lung on chest X-ray and a mosaic pattern on chest CT [2]. Our patient’s radiological examinations were not similar to the typical radiological images of this disease.
Considering the typical clinical history and radiological examinations, as well as the less likelihood of the previously described differential diagnoses, we assumed the probable diagnosis to be a left lung and pulmonary artery hypoplasia with consequent pulmonary hypertension and increased collateral circulation. The latter, in association with a pulmonary infection, led to the development of hemoptysis. No further studies were performed due to our patient’s age and fragility as well as the absence of therapeutic implications associated with their potential results.
Although rare and typically associated with childhood, these diseases can in exceptional cases be present in adult life, since a combination of some characteristics may allow children to survive. Their diagnosis is challenging in adults as they can easily be mistaken for more common diseases. However, an early diagnosis is extremely important because it allows a close follow-up and a consequent timely detection and treatment of complications, such as pulmonary infections and hemoptysis, but especially pulmonary hypertension.