ABSTRACT
A 77-year-old man was admitted to the internal medicine department for a 5-day history of progressive preauricular swelling. Two lines of antibiotic treatment failed to achieve any improvement. Fine needle aspiration cytology was conducted and smear staining with the Ziehl-Neelsen stain as well as a PCR test were positive for Mycobacterium tuberculosis. These results were confirmed with culture of the sample. A diagnosis of tuberculosis parotitis was made and anti-tuberculous drugs were initiated.
LEARNING POINTS
- In patients not responding to usual antibiotic treatment, other rare causes of parotitis should be suspected.
- Fine needle aspiration cytology was an important procedure in establishing the diagnosis.
KEYWORDS
Parotid tuberculosis, inflammatory swelling, Mycobacterium tuberculosis
INTRODUCTION
The incidence of tuberculosis is increasing among the general population of developing countries. Despite being a common infection, tuberculosis of the major salivary glands is rarely encountered in daily clinical practice. Tuberculous parotitis constitutes 2.5–10% of salivary gland tuberculosis[1,2]. As a result, it is often misdiagnosed as a parotid neoplasm.
CASE PRESENTATION
A 77-year-old man was admitted to the internal medicine department for a 5-day history of progressive preauricular swelling. The swelling was painless, insidious in onset and progressively increased in size. The patient had been previously evaluated by his primary doctor on 2 occasions and was on oral ciprofloxacin without any improvement. The patient reported that he felt weaker than usual over the past 7 days. No history of fever, cough, shortness of breath or weight loss was noted.
His past medical history was relevant for end-stage chronic renal disease secondary to diabetic nephropathy, hypertension, coronary artery disease and chronic obstructive pulmonary disease. His family history was relevant for type 2 diabetes mellitus and hypertension.
With respect to social history, he had no known drug or food allergies, as well as no history of smoking, alcohol abuse or illicit drug use. There had been no exposure to tuberculosis and no recent travels.
The physical examination revealed an alert patient with a regular pulse rate of 84 beats/min, blood pressure of 110/70 mmHg, a respiratory rate of 20 breaths/min and an oxygen saturation of 95% while breathing room air. Local examination revealed a 4×3 cm swelling in the left parotid region that was slightly tender accompanied by small non-painful anterior cervical lymphadenopathies. Heart sounds were regular without any rubs or murmurs. The lungs were clear. The rest of the physical examination was normal.
Blood tests showed elevated C-reactive protein (330 mg/l), leucocytosis (17.59×109/l) with a predominance of polynuclear neutrophils (13.72×109/l) and thrombocytosis (555×109/l). The glomerular filtration rate (GFR) was 15 ml/min, serum creatinine was 357 µmol/l and urea was 31.8 mmol/l. Electrolytes were within normal ranges. Coagulation, liver and thyroid tests were normal. Angiotensin-converting enzyme, antinuclear antibodies and anti-SSA/SSB were negative. Serology for HIV, HBV, HCV, CMV and EBV returned negative. Blood cultures were negative.
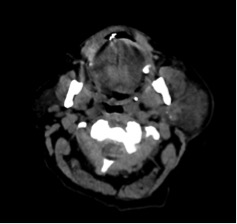
Ciprofloxacin was discontinued and intravenous ceftriaxone 1,000 mg and metronidazole 500 mg 3 times per day was initiated. On day 5 after admission, no clinical or biological improvement was achieved. A non-contrast neck scan was performed; it showed the presence of a significant infiltration of the left parotid compartment with parotitis without any detected collection. The infiltration extended to the left latero-cervical part of the compartment up to the base of the neck with fat infiltration, thickening of the skin and thickening of the superficial cervical fascia (Fig. 1).
Figure 1. A neck scan showed an infiltration of the left parotid compartment with parotitis without any detected collection
After discussion, fine needle aspiration cytology (FNAC) was conducted. The cytological assessment showed only neutrophils, lymphocytes and cellular debris. Smear staining with the Ziehl-Neelsen stain as well as a PCR test were positive for Mycobacterium tuberculosis. These results were confirmed with culture of the sample. The patient was diagnosed with tuberculous parotitis and anti-tuberculous drugs were initiated. Chest radiography was normal and the Tuberculosis Skin Test (PPD) was 12 mm.
DISCUSSION
Tuberculous parotitis may clinically present as an asymptomatic unilateral preauricular swelling, recurrent swelling with fistula or acute inflammatory swelling/abscess[2]. Parotid glands are the salivary glands most commonly involved in primary tuberculosis, whereas the submandibular glands are the most commonly involved in systemic tuberculosis as the result of drainage of the mouth occurring mainly to the submandibular lymph nodes.
Two hypotheses have been considered in the pathogenesis of tuberculous parotitis: the direct spread of mycobacteria from a nearby infected source or haematogenous or lymphatic spread from the lungs. The sources may be the tonsils or teeth and the spread may occur through direct inoculation by sputum, retrograde spread of bacilli through ducts due to the low flow of saliva at rest or by afferent lymphatics. The gland may be infected by haematogenous or lymphatic spread from the lungs. It is hypothesized that a hypersensitivity reaction on initial infection leads to the bacilli being covered in scar tissue. These bacteria are reactivated during low immunity after a period of months to years[3,4].
The patient presented with an acute inflammatory swelling; localized, slow-growing and slightly tender, localized in the left preauricular region. Pain, abscess, fistula and facial nerve involvement are late features but were not seen in our case. Furthermore, the constitutional symptoms of tuberculosis such as cough, fever, weight loss and loss of appetite, as described in the literature[5], were not seen.
The diagnosis of tuberculous parotitis is very difficult owing to the absence of symptoms, especially in the absence of pulmonary infection, and it may often be misdiagnosed as a benign parotid tumour as was initially the case for this patient.
A precise history, clinical examination and FNAC have been proposed for the diagnosis of tuberculous parotitis. FNAC has a high sensitivity (80%) and specificity (93%) but it is only of value when positive, even though false-positive results can be obtained especially in cases of large and necrotic parotid gland neoplasms[2]. Ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI) could be helpful in the diagnosis but are nonspecific. Ultrasonography is sensitive for lesions situated in the superficial lobe of the parotid gland, while CT/MRI is better for deep-lobe involvement[4].
The differential diagnosis should also include: actinomycosis, suppurative parotitis, mumps, HIV, sarcoidosis and Sjogren's syndrome[4]. Most cases of tuberculous parotitis have been reported in India and other endemic areas. Medical treatment consists of the combination of powerful anti-tuberculous drugs according to the regimen: 2RHZ/4RH for a period of 6 to 9 months[2,4].
CONCLUSIONS
Tuberculous parotitis is a rare entity but it should be suspected in patients not responding to usual antibiotic treatment. Its diagnosis requires a high index of clinical suspicion.