ABSTRACT
Emphysematous pancreatitis is a rare and fatal complication of acute necrotizing pancreatitis. We report a radioclinical observation of a 61-year-old female patient who consulted for epigastric pain radiating to the back, associated with vomiting and elevated lipasaemia more than 3 times the normal value. The abdominal computerized tomography (CT) scan carried out on the fourth day of hospitalization, based on worsening of the clinical condition, showed pancreatic necrosis associated with the presence of air bubbles. Percutaneous puncture of a peripancreatic collection was positive for Escherichia coli. A diagnosis of emphysematous pancreatitis was established. The clinical and biological evolution of our patient was favourable with antibiotic treatment.
LEARNING POINTS
- Emphysematous pancreatitis is a rare and fatal complication of acute necrotizing pancreatitis.
- Abdominal CT allows for suspicion of this pathology based on the intra- and/or peripancreatic presence of air.
- The diagnosis is confirmed by the isolation of the bacterial agent in peripancreatic needle aspiration fluid.
KEYWORDS
Acute necrotizing pancreatitis, infection, emphysematous pancreatitis
INTRODUCTION
Emphysematous or gangrenous pancreatitis is a rare and fatal complication of acute necrotizing pancreatitis. It is characterized by the presence of gas in the necrotic pancreatic parenchyma and/or in peripancreatic collections[1]. Abdominal CT is the examination modality of choice with high sensitivity and specificity for gas detection, collection and vascular pedicle abnormality detection, as well as other complications associated with acute pancreatitis[2]. It allows for suspicion of emphysematous pancreatitis based on the intra- and/or peripancreatic presence of air, in a context of epigastric pain with elevated lipasaemia, 3 times higher than the normal value[3]. However, gas is only observed in a minority of proven infections (12 to 22%). The absence of gas does not exclude a diagnosis of secondary infection of acute necrotizing pancreatitis[4]. Therefore, confirmation of the diagnosis is by percutaneous puncture of a peripancreatic collection in the context of a worsening clinical state despite adequate treatment. The objective of this work is to present through a case, the radiological aspects of emphysematous pancreatitis, as well as presenting the elements of the radiological report.
CASE DESCRIPTION
A 61-year-old female patient with no specific medical history presented to the emergency department of University Hospital Centre Ibn Rochd of Casablanca for sudden-onset epigastric pain radiating to the back for 2 days, associated with nausea and vomiting. On examination, her temperature was 36.5°C, blood pressure was 120/70 mmHg, heart rate was 96 beats per minute and the respiratory rate was 16 cycles per minute. The patient had epigastric and right hypochondrium tenderness. The rest of the examination was unremarkable. Blood tests showed hyperleucocytosis of 18,680.103 cells/µl of blood, C-reactive protein (CRP) levels of 185.4 mg/l, lipasaemia of 450 IU/l and creatinine levels of 16 mg/l. The diagnosis retained was acute pancreatitis.
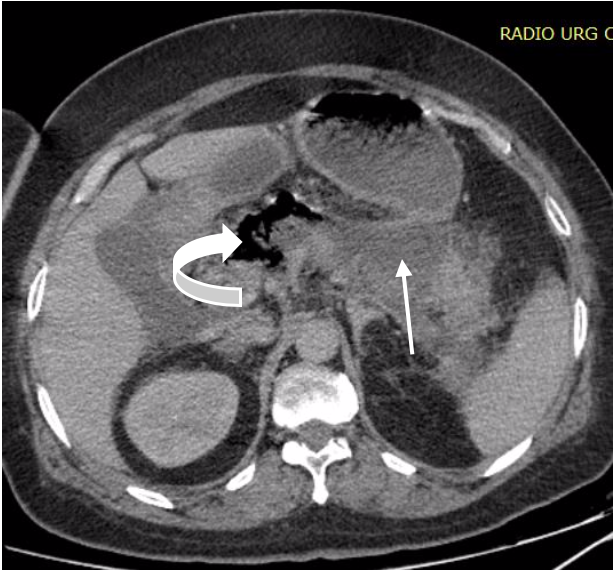
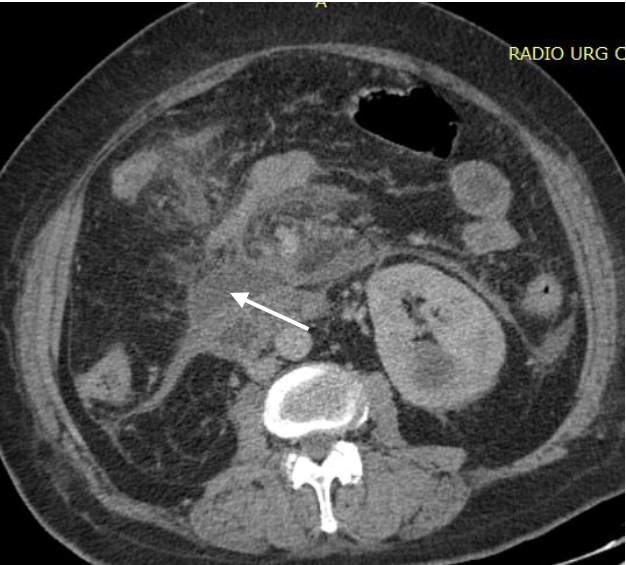
After 4 days of hospitalization, the patient developed a fever of 39°C, with a deterioration in clinical condition. Abdominal CT was requested and showed a pancreatic corporocephalic necrosis of more than 50%, the presence of air bubbles (Fig. 1), several peripancreatic collections (Fig. 2), right colonic parietal thickening (Fig. 3) and peritoneal effusion and thrombosis of the superior mesenteric vein extending to the portal trunk (Fig. 4).
Figure 1. Axial contrast-enhanced CT section showing corporocephalic pancreatic necrosis (arrow) and the presence of air bubbles (curved arrow)
Figure 2. Axial contrast-enhanced CT section showing infiltration of the peripancreatic fat which was the site of collections (arrow)
Figure 3. Axial contrast-enhanced CT section showing right colonic parietal thickening with submucosal oedema (arrow)
Figure 4. Axial CT scan after contrast injection in the portal phase showing the non-homogeneous enhancement of the portal trunk (curved arrow) related to partial thrombosis of the portal trunk
Percutaneous puncture of a peripancreatic collection for bacteriological analysis was positive for Escherichia coli as a pathogenic agent, which was multisensitive to antibiotics. The clinical and biological evolution of our patient was favourable under antibiotic treatment. She was discharged after 15 days of hospitalization.
DISCUSSION
Emphysematous pancreatitis results from acute necrotizing pancreatitis superinfection with Gram-negative bacteria, with Escherichia coli being the most frequently isolated. Other pathogens such as Klebsiella, Pseudomonas, Enterobacter and Clostridium perfringens are sometimes encountered [1]. This pathology occurs mainly in immunocompromised patients, especially in diabetic individuals [5].
Many mechanisms for superinfection have been discussed. Bacterial superinfection may result from haematogenous or lymphatic circulation. It may also occur through the ampulla of Vater or via contiguity with the adjacent colonic wall. Vesicular lithiasis migrating to the level of the lower bile duct and alcohol consumption are the main aetiologies of acute pancreatitis. Other possible but less frequently encountered aetiologies are metabolic, medicinal and infectious causes, as well as autoimmune and genetic diseases. Gastroduodenal ulcer perforation can rarely occur in the pancreas with glandular superinfection[6].
CT is the examination modality of choice for detection of intra- and/or peripancreatic gas that allows suspicion of emphysematous pancreatitis in a suggestive clinical and biological context. The diagnosis is confirmed by isolation of the bacterial agent in peripancreatic needle aspiration fluid, accompanied by an antibiogram. In our case, Escherchia coli was isolated and was multisensitive to antibiotics.
The differential diagnosis of emphysematous pancreatitis includes entero-pancreatic fistula due to rupture of a pancreatic pseudocyst, an external duodenal diverticulum, pancreatic biopsy and pancreatic lumpectomy with postoperative air bubbles[3].
The elements of the radiological report must include a description of the pancreatic parenchyma (presence and extension of necrosis with gas); a description of the collections; an evaluation of the severity of acute pancreatitis according to the CT severity index (CTSI) and the presence or absence of ascites, pleural effusion, gallstones, dilation of the bile ducts, vascular anomalies (portal thrombosis, arterial pseudoaneurysm) and neighbouring inflammatory anomalies, in particular, those that are digestive (colon, stomach, duodenum, small intestine), splenic, hepatic or renal [4]. A well-established radiological report allows the avoidance of omission of locoregional complications. Despite adequate management, the death rate from emphysematous pancreatitis remains high at 50% of cases [5]. Mortality occurs within the context of sepsis with multiorgan failure.
CONCLUSIONS
Emphysematous pancreatitis results from a superinfection of an acute necrotizing pancreatitis, occurring most often in immunocompromised patients. Abdominal CT is the examination modality of choice for suspicion of emphysematous pancreatitis, which is indicated by the presence of intra- or peripancreatic gas in an evocative clinical and biological context. The diagnosis is confirmed by isolation of the pathogen in the peripancreatic aspiration fluid. However, mortality remains at a high level despite adequate treatment, occurring usually in a sepsis context with multiorgan failure.