ABSTRACT
Introduction: Despite the extremely favourable prognosis of patients with cerebral venous thrombosis (CVT), death occurs in 10–15% of patients. In severe cases of malignant CVT with supratentorial haemorrhagic lesions, cerebral oedema and brain herniation, decompressive surgery may be the only life-saving treatment.
Patient and methods:We present the case of a puerperal young woman with progressive headache, seizures and decreased alertness. Thrombosis of the entire superior sagittal sinus with bifrontal venous infarcts and midline shift was confirmed by magnetic resonance imaging with venography sequencing. Despite medical treatment with anticoagulation, progressive neurological deterioration was observed, so bilateral, frontal decompressive craniectomy was performed.
Results: At the 6-month follow-up, we observed partial functional recovery with a modified Rankin score of 3.
Discussion: Bilateral decompressive craniectomy may be a life-saving therapeutic option when medical therapy fails and there are clinical and radiological features of progression in both cerebral hemispheres.
LEARNING POINTS
- Malignant cerebral venous thrombosis presents with diffuse haemorrhagic lesions or cerebral oedema associated with brain herniation and rapid clinical deterioration.
- Decompressive surgery may be the only life-saving treatment in severe cases.
- Early and adequate intervention based on the characteristics of the lesions allowed preservation of life and improvement in long-term functionality.
KEYWORDS
Bilateral craniectomy, decompressive craniectomy, malignant cerebral venous thrombosis
INTRODUCTION
Malignant cerebral venous thrombosis (CVT) presents with diffuse haemorrhagic lesions or cerebral oedema associated with brain herniation and rapid clinical deterioration. Approximately 0.5% of stroke patients per year have CVT, and 4% of these CVT cases can be categorized as malignant[1]. Although anticoagulation therapy remains the cornerstone of treatment, other measures such as bilateral decompressive surgery should be considered in severe cases.
CASE DESCRIPTION
A 21-year-old woman was admitted to the emergency room in her second week of puerperium because of headache, seizures and decreased alertness. A computed tomography (CT) scan showed no remarkable alterations. The patient had no significant medical history. In the initial neurological evaluation, we found her to be poorly reactive and confused, with eye-opening to pain, symmetric and reactive pupils, brain stem reflexes present and localized pain with movement of the extremities as well as bilateral Babinski signs. A Glasgow Coma Scale (GCS) of 11 points was calculated.
Methods and Procedures
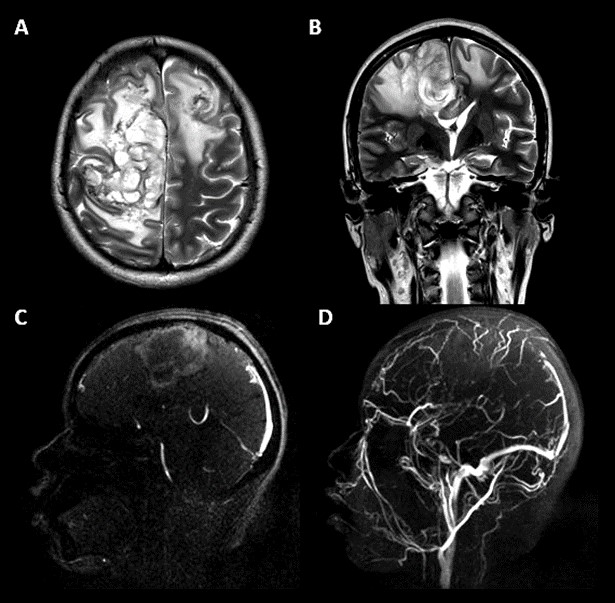
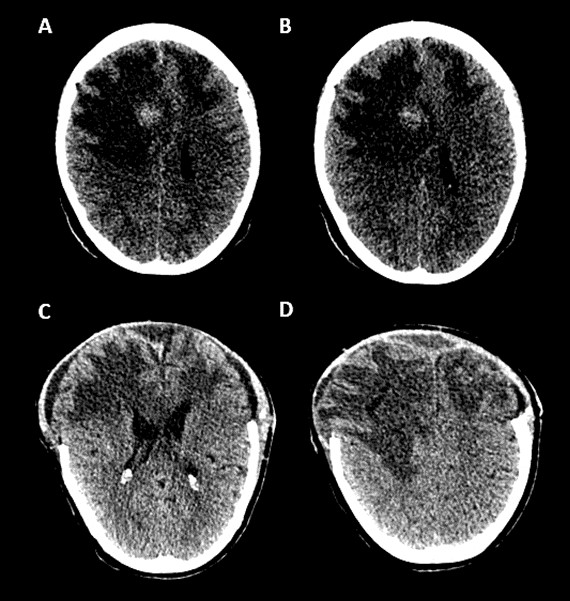
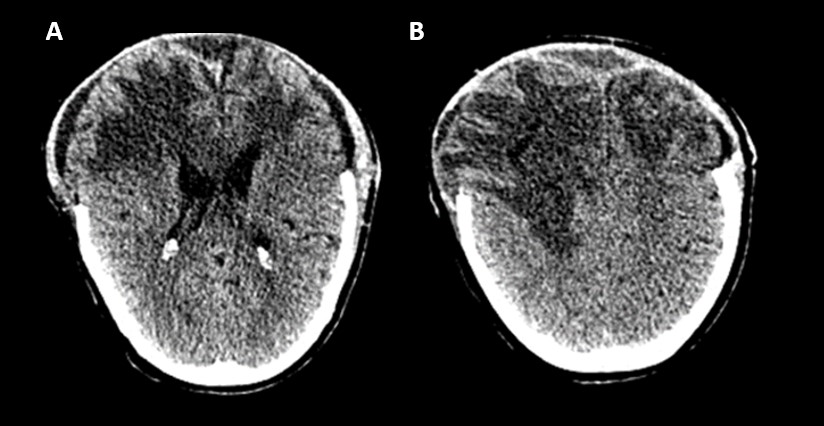
Magnetic resonance imaging (MRI) with a 3D time of flying (3D TOF) sequence showed thrombosis of the sagittal superior sinus with bifrontal venous infarcts (Fig. 1). Therapeutic anticoagulation with low-molecular-weight heparin was started. The patient remained stable during the following days, but neurological function deteriorated with the absence of pupillary reflexes, and a GCS of 7 was observed at 5 days. A new CT scan showed haemorrhagic transformation of the bilateral infarcts accompanied by severe oedema. Lesions on both sides were large and associated with midline shift greater than 5 mm (Fig. 2). Because of the clinical deterioration and length of the lesions, the patient underwent bifrontotemporal decompressive craniectomy (Fig. 3).
Figure 1. (A, B) Axial and coronal T2 sequences show right frontal parasagittal irregular hyperintensity suggestive of venous infarct with bilateral oedema and midline shift. (C, D) The 3D TOF sequence shows thrombosis of the superior sagittal sinus
Figure 2. Right frontal parasagittal venous infarct with haemorrhagic transformation and bilateral frontal severe oedema causing midline shift
Figure 3. Postsurgical non-contrast CT shows bilateral frontotemporal craniectomy and bilateral frontal oedema with anatomical restoration
After the procedure, she remained under sedation with mechanical ventilation support, and 3 weeks later was extubated. She maintained good clinical evolution and stable vital signs and was discharged 1 month after the procedure. Upon hospital discharge, she had quadriparesis and required support for all her activities of daily life. A modified Rankin score (mRs) of 5 points was calculated.
Genetic tests for MTHFR mutations and other studies such as those evaluating antithrombin III, anticardiolipin antibodies, lupus anticoagulant and anti-beta 2 glycoprotein antibodies were performed, and the results were reported as normal.
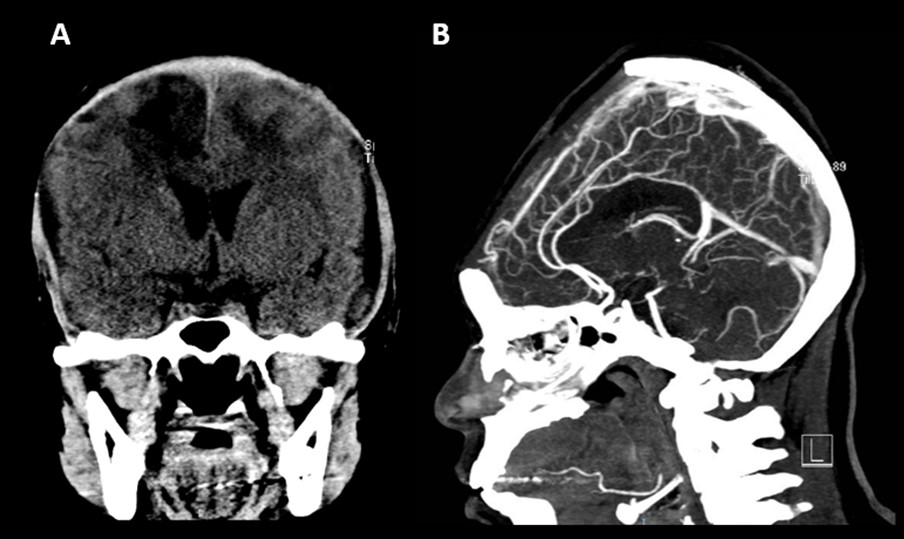
Treatment with dabigatran was maintained for the following months. By the 6-month follow-up, the patient was able to walk without assistance and attend to her basic needs, and an mRs of 3 was calculated. A new CT scan with venography revealed partial recanalization of the sagittal superior sinus (Fig. 4).
Figure 4. Bifrontal hygromas with compression of the cerebral parenchyma and partial recanalization of the sagittal superior sinus
DISCUSSION
The rate of CVT is higher in Mexico than in other countries. In a large stroke registry in our hospital, approximately 6.3% of all stroke patients during a 25-year period were CVT cases. Many of these patients developed severe presentations with bilateral infarcts (27.9%) and haemorrhagic transformation (38.4%)[2]. In our patient, a diagnosis of malignant CVT was made because of her rapid neurological deterioration, bilateral venous infarcts, haemorrhagic transformation and severe oedema with bilateral midline shift. No risk factors other than puerperium were found.
There are two main objectives in the treatment of CVT: recanalization of the affected sinus with early anticoagulant therapy, and management of the mass effect due to oedema and haemorrhage. The ESO-EAN Guidelines strongly recommend decompressive neurosurgery, although this recommendation was supported by a low level of evidence[3].
However, in most cases, decompression is required only from one side. The indication for bilateral craniectomy is limited to very severe cases with extensive bilateral lesions, and it may be more controversial.
In this case report, the clinical deterioration and the extent of bilateral lesions with mass effects made decompressive surgery an urgent procedure to save the patient’s life. Radiological features such as bilateral midline shift, haemorrhage and oedema helped determine that bifrontal craniectomy was a better option than hemicraniectomy.
Previous studies on decompression in CVT patients are retrospective or have a very small sample size and thus may overestimate the treatment effect. Many factors such as the time of anticoagulant therapy before surgery and a short interval between symptom onset and midline deviation to the time of the procedure have been associated with good outcomes[4]. In contrast, decreased levels of consciousness, seizures, intracerebral haemorrhage and bilateral lesions are predictors of unfavourable outcomes[5].
In our patient, seizures, decreased alertness, bilateral and large lesions with midline shift and haemorrhagic transformation were considered factors indicating a poor prognosis prior to the procedure; early and adequate intervention based on the characteristics of the lesions allowed the preservation of life and improvement in long-term functionality. Our case shows that bilateral craniectomy may be an option in patients with severe bilateral lesions and progressive neurological deterioration despite treatment with anticoagulation, both to preserve the patient´s life and for acceptable functional recovery.
CONCLUSION
Although most patients who require decompressive craniectomy have clinical and radiological factors associated with poor outcomes, bilateral decompressive craniectomy is a procedure that allows the preservation of life and improvement in functional prognosis in patients with a malignant presentation of the disease.