ABSTRACT
Home parenteral nutrition is a therapeutic option for chronic intestinal failure. A tunnelled central venous catheter is commonly used for self-application of nutrition and hydration over a long period of time; that is, months or years. Air embolization within the venous circulation can be caused by inconsistent self-handling of the catheter in combination with air bubbles in the infusion set. Paradoxical air embolization within the brain and coronary arteries together with catheter perforation is a rare medical and technical complication. The authors report the case of a 63-year-old woman with type 3 chronic intestinal failure treated with home parenteral nutrition. During the first year of treatment and use of the catheter a fatal complication occurred. The patient experienced recurring asystolic episodes and strokes with monoplegia during flushing of the catheter. Although 2 resuscitations were successful, the third was not, and the patient died. The cause of these life-threatening complications was an unknown patent foramen ovale, with paradoxical air embolization within the coronary and brain arteries. The authors discuss the clinical consequences of arterial and venous air embolization, the differences between these and the therapeutic algorithm with a link to practice.
LEARNING POINTS
- Home parenteral nutrition using a Hickman central venous catheter is a therapeutic option for chronic intestinal failure.
- Paradoxical air embolization is a rare complication with an unknown patent foramen ovale.
- A very small volume of air (0.5–3 ml) in coronary or brain arteries can cause fatal complications such as asystole and brain ischaemia.
KEYWORDS
Air embolization, patent foramen ovale
INTRODUCTION
Chronic intestinal failure requires long-life parenteral substitution. The best therapeutic option is home parenteral nutrition (HPN) with patient self-management at home. Tunnelled central venous catheters are frequently used for delivery of home nutrition in type 3 irreversible intestinal failure. Hickman long-term central venous catheters are inserted into the internal jugular or subclavian vein with the end near the right atrium of the heart. Proper handling of the catheter minimizes complications. The most common complications associated with the catheter are: catheter-related bloodstream infection and sepsis, thrombosis at the end of the catheter and intraluminal thrombosis with obturation of the lumen. A rare complication is air embolization (venous or arterial). Arterial air embolization can be caused by a patent foramen ovale or through arteriovenous shunts in the lung circulation (this is very rare). Of note, there is an extremely important clinical difference regarding the presence of air in venous and arterial circulation
CASE DESCRIPTION
The 63-year-old female patient had 3 malignancies in her medical history; breast cancer with quadrantectomy and chemotherapy, renal cancer with nephrectomy without metastases and stomach cancer with a total gastrectomy with chemotherapy and radiotherapy.
Each of the 3 malignancies was in complete remission after therapy, without local or distant metastases. The patient underwent multiple abdominal operations (cholecystectomy, hysterectomy and ovariectomy). From the last operation (gastrectomy), she had abdominal pain, cramps and diarrhoea due to adhesive ileus, which required repeated surgical therapy with bowel resection. She lost 30 kg per year (BMI of 15) with subsequent impairment of movement. A diagnosis of chronic intestinal failure was made. The causes of intestinal failure were: post-actinic enteropathy, repeated chemotherapy with mucosal injury, repeated resection for adhesive ileus and multiple blind bowel loops. Enteral feeding was ineffective with progressive weight loss, and so, HPN was initiated. A Hickman tunnelled central venous catheter was inserted into the vena jugularis interna. Complete parenteral nutrition with hydration, vitamins and trace elements was administered daily. The catheter was taurolidine/acid-protected to minimize infection and sepsis.
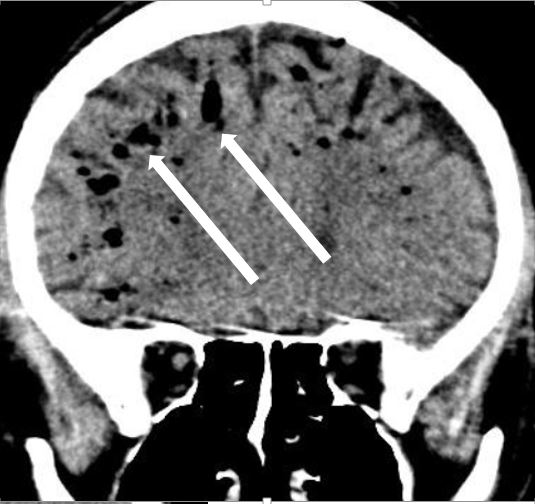
Almost 1 year of HPN was successful in terms of weight gain, with full recovery of mobility. The patient was admitted to the intensive care unit of the Internal Clinic for coma (Glasgow Coma Scale score of 3) after flushing of the catheter and administration of catheter lock fluid. During ECG monitoring, an asystolic episode was registered, followed by successful resuscitation. Neurological examination with a CT scan of the brain revealed ischaemic stroke in the left arteria cerebri media basin. Consciousness improved in a week (Glasgow Coma Scale score of 15). Strokes were repeated twice with right-sided upper limb monoplegia. A control CT brain scan displayed extensive air collections (bubbles) with a subarachnoid location in the supratentorial region of both hemispheres, along the falx and sagittal sinus (Fig. 1), and post-ischaemic lesions in the left part at a subacute stage (without head trauma or skull injury). The only possible source of air bubbles in the brain arteries could have been the Hickman catheter along with an unknown patent foramen ovale. Transoesophageal echocardiography (TOE or TEE) was performed without revealing a shunt between the atria. The left atrial appendage was without clots. The Hickman catheter was partially damaged and ruptured due to resuscitation, and was replaced with a new one. Within a short time period, recurring asystole was registered. The third episode was fatal; after an unsuccessful resuscitation attempt, the patient died.
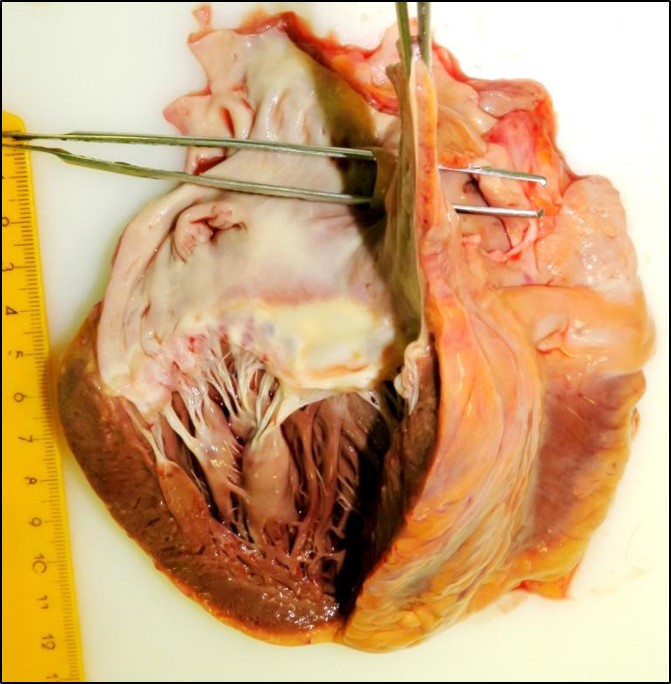
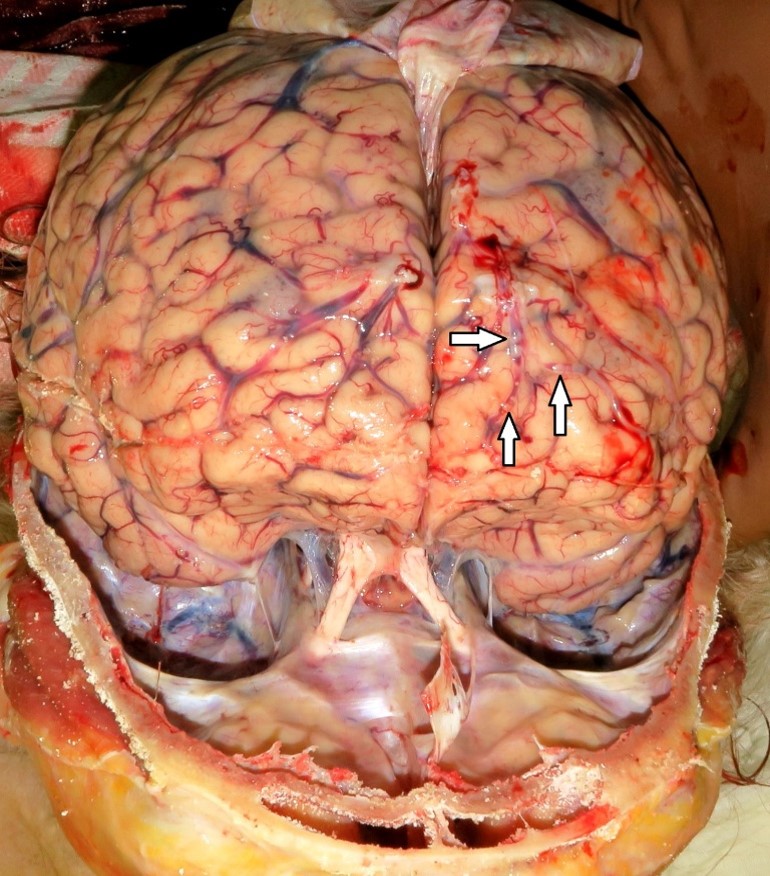
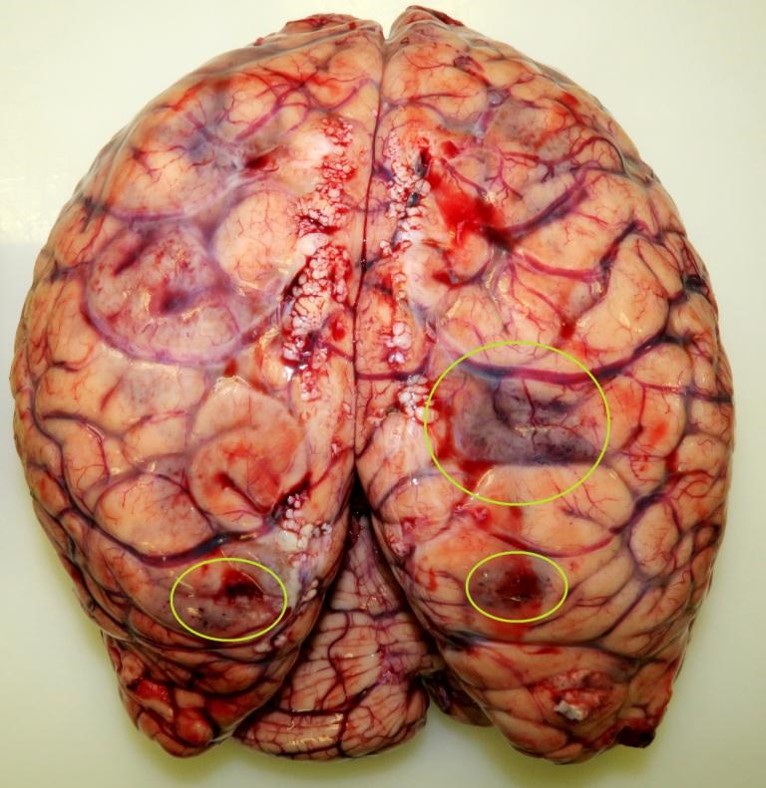
A clinical autopsy revealed a patent foramen ovale (Fig. 2), not found with TOE (opening 12×4 mm), and air bubbles in brain surface arteries (Fig. 3) and multiple brain infarctions (Fig. 4). Near the Hickman catheter a wall thrombus was observed in the vein. In the abdomen, there was a small bowel “sticky” conglomerate without a detectable bowel lumen and excessive adhesions.
Figure 2. A patent foramen ovale: autopsy
Figure 3. Air bubbles in the brain vessels (arrows): autopsy
Figure 4. Ischaemic changes within the brain: autopsy
DISCUSSION
Paradoxical air embolization is a rare and fatal complication of an inserted tunellized long-term central venous catheter. Air can be drawn in during administration of parenteral nutrition or through a damaged wall in the catheter (a small crack in the wall). A patent foramen ovale (communication between the cardiac atria) occurs frequently in 25% of the population; in patients with cryptogenic brain infarction prevalence is very high, up to 70% [1, 2]. This case report documents paradoxical air embolization within brain arteries through an unknown patent foramen ovale and to coronary arteries with recurring asystolic episodes, with a fatal end. The first episode of brain air embolization was during catheter flushing with a physiological solution and lock. It is likely that the solution may have contained small air bubbles, which were transported to the left atrium due to high pressure during flushing. In clinical practice, a very large and important difference exists between venous and arterial air embolization.
Venous air embolization may result from catheterization of the right heart, head and neck surgical procedures and injuries in this localization. Occurrence of this complication is 1/47 to 1/3,000. The lethal air volume is 50–100 ml; mortality is 23–50%. Embolism supporting factors are: hypovolaemia, deep inspiration and the sitting position. Air bubbles migrate via pulmonary artery branches to lung circulation. Air is mixed with blood to form a foam in the right ventricle. A small amount of air (under 50 ml) in the lung circulation is without clinical effect. 50–100 ml causes vasoconstriction and pulmonary hypertension [3, 4]. Arterial air embolization is the most common paradoxical embolization, due to passage of air from the right to the left atrium through a patent foramen ovale. More rarely, passage of air through arteriovenous shunts in the lung circulation can be the cause. Very rare is the migration of air to coronary arteries during catheterization of the left heart (incidence 0.1–0.3%, mortality 1%). Percutaneous lung biopsy can also be complicated with air embolization (incidence 0.02–0.07%, mortality 26%). 0.5–3 ml of air is a lethal volume in arteries. Air bubbles can cause acute ischaemic changes in organs. The most serious manifestation is embolization within the brain arteries with acute ischaemic stroke with paresis or plegia. Ventricular fibrillation, asystole and acute cardiac ischaemia are caused by air bubbles in coronary arteries [5–7].
CONCLUSION
Paradoxical air embolization was a rare and fatal complication of an inserted tunnellized long-term central venous catheter in a patient with a patent foramen ovale. Precise and careful handling of the catheter minimizes air ingress to the heart and circulation.