ABSTRACT
Uterine leiomyomas are very common gynaecological benign tumours. Spontaneous torsion of a uterine subserosal leiomyoma is a rare cause of acute lower abdominal pain and should be treated immediately with surgery. We report a case of an enlarged subserosal leiomyoma that was first detected by computed tomography (CT) and further confirmed by laparoscopic surgery to be a subserosal leiomyoma with torsion.
LEARNING POINTS
- Spontaneous torsion of a uterine subserosal leiomyoma is a rare cause of acute lower abdominal pain.
- Contrast-enhanced CT of the pelvis reveals changes in size, abnormal or absent enhancement of the leiomyoma, and congestion of the vascular pedicle at the site of torsion.
- CT imaging can help in the accurate diagnosis of leiomyoma torsion.
KEYWORDS
Uterine leiomyoma, complication, torsion, diagnostic imaging
CASE DESCRIPTION
A 50-year-old postmenopausal woman presented to our emergency department with acute sudden lower abdominal pain for 2 hours associated with dizziness. She denied trauma or vaginal bleeding and had no other associated symptoms. Her medical history was significant only for a uterine fibroid. Her vital signs were stable. Abdominal examination revealed distension of the lower abdomen with diffuse tenderness, guarding and muscle rigidity. The white blood cell count was 11,900/µl (normal value 4,000–10,000/µl) with 88% neutrophils (normal value 40.0–74.0%), and C-reactive protein was elevated to 2.5 mg/dl (normal value <0.5 mg/dl). An ultrasound (US) scan revealed free pelvic fluid and a uterine leiomyoma. The patient later underwent an oral-contrast enhanced CT scan of the abdomen and pelvis before and after administration of an intravenous contrast agent. The CT scan revealed a large pelvic mass, measuring 10.3×5.1×12 cm, arising from the anterior wall of the uterine corpus. It had a heterogeneous appearance with hypodense regions. After injection of contrast medium, there was enhancement of a thin wall, but no enhancement inside the mass (Figs. 1 and 2). We presumed that it was a subserosal uterine leiomyoma. There was also a fan-shaped, poor contrast enhancement area in the uterus adjacent to the mass and free fluid in the pelvic region (Fig. 3). CT scanning also revealed an enlarged appendix, without fat stranding, so appendicitis was less likely to be the cause of the lower abdominal pain (Fig. 4). We presumed that the most probable diagnosis and cause of pain was torsion of a pedunculated subserosal uterine leiomyoma.
Figure 1. Sagittal CT scan (+iv contrast) of abdomen reveals a large heterogeneous pelvic mass (*). Note there is contrast enhancement at the thin wall (black arrow) of the mass. Also, there is free fluid (white arrow) in the pouch of Douglas
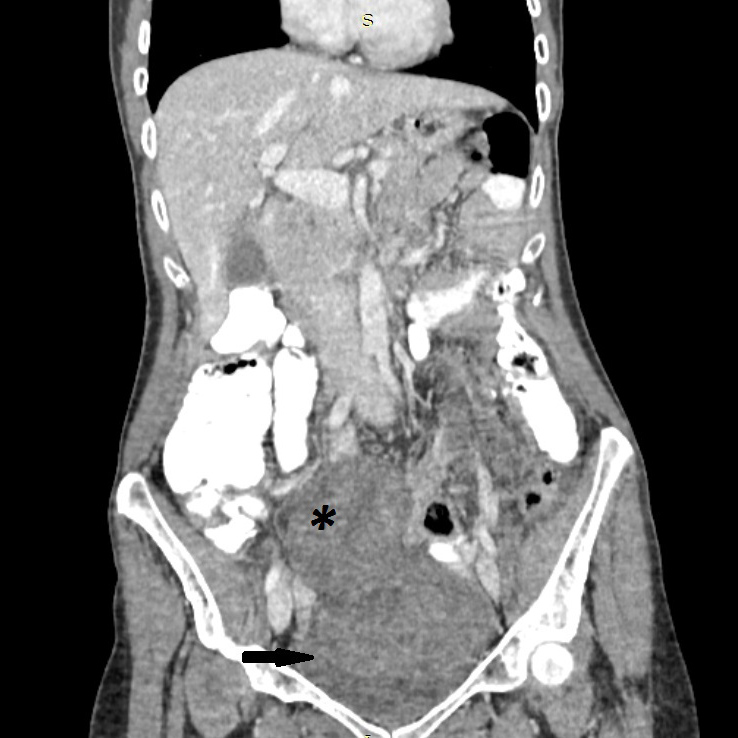
Figure 2. Coronal CT scan (+IV contrast) of the abdomen reveals a large heterogeneous pelvic mass (*). Note there is only contrast enhancement at the thin wall (black arrow) of the mass
Figure 3. Axial CT scan (+IV contrast) of the abdomen reveals a large heterogeneous pelvic mass (*). Note the dark fan sign (black arrow) and also the fluid (white arrow) in the pouch of Douglas
Figure 4. Axial CT scan (+IV contrast) of the abdomen reveals a large heterogeneous pelvic mass (*). The appendix is enlarged but without fat stranding (black arrow)
The current US scan showed the uterine leiomyoma had enlarged greatly since the last US scan was carried out 1 month previously.
Since the patient did not improved clinically and uterine leiomyoma torsion was suspected, a diagnostic laparoscopy under general anaesthesia was carried out the following day. A dark blue subserosal leiomyoma, approximately 11 cm in size, was identified on a twisted pedicle attached to the anterior surface of the uterus. The patient recovered after surgery with an uneventful postoperative course and was discharged home 10 days later.
DISCUSSION
Uterine leiomyomas are the most frequent gynaecological tumours, occurring in 20–30% of women of childbearing age. Depending on their intrauterine location, they are classified as: submucosal, intramural and subserosal [1]. Although usually asymptomatic, if they do cause symptoms, the most frequent are vaginal bleeding, abdominal pain, mass effect and even infertility [2]. Despite the fact that torsion of a uterine leiomyoma is considered a surgical emergency, other potential causes of acute abdomen such as appendicitis, pelvic inflammatory disease, ovarian torsion and red degeneration of fibroid should be excluded before considering leiomyoma torsion [3]. Red degeneration is occasionally seen in a fibroid, especially during pregnancy [1, 2]. Conversely, torsion of a subserous pedunculated fibroid is incredibly rare and only a few cases have been described in the literature. It produces symptoms of varying severity, depending on the degree of rotation. If torsion of the pedicle is partial and intermittent with spontaneous untwisting, symptoms may subside. However, complete torsion results in circulatory stasis that is initially venous with oedema and congestion and then causes compression of the arterial blood supply. Obstruction of the arterial network produces haemorrhagic necrosis [3]. The diagnosis is based on clinical manifestation and radiological examination. Diagnosis is usually difficult preoperatively, partly because no known specific findings are associated with this condition. However, knowledge about it is important since diagnostic delay can lead to leiomyoma necrosis with resulting peritonitis and life-threatening sepsis.
US, as the primary imaging modality of choice for the assessment of acute pelvic pain, can identify a subserosal leiomyoma but not its torsion. A simple fibroid is usually seen as a hypoechoic lesion that may be well-defined and arising within the surrounding myometrium [2]. Torsion of a subserosal leiomyoma may be suspected when colour Doppler demonstrates a twisted pedicle or when there is a space between the leiomyoma and the uterus. However, US may not be an effective method especially when the twisted pedicle is thin and invisible. As a result, the role of CT in this clinical setting is becoming more important [4].
CT can be performed as a second-line imaging modality for the evaluation of acute lower abdominal pain, but it is regarded as the first diagnostic tool utilized in an emergency setting for identifying acute torsion of uterine leiomyoma. Contrast-enhanced CT of the pelvis reveals interval changes in size, while the continuity of the mass with the uterus is an accurate sign of the uterine origin of the mass. In addition, an advantage of CT scanning compared with US is that, using intravenous contrast material, we can see abnormal or absent enhancement of the leiomyoma and congestion of the vascular pedicle at the site of the torsion. The typical CT features are poor contrast enhancement, thin rim enhancement and a dark fan sign (fan-shaped poor contrast enhancement in the area of the uterus adjacent to the leiomyoma) [2]. Although these findings indicate leiomyoma with acute torsion, some of them are also seen in leiomyoma with red degeneration. Degenerate fibroids also appear complex and contain areas of fluid attenuation [3, 4]. Also, red degeneration is a common complication of pregnancy, there are haemorrhagic areas inside the leiomyoma and enhancement is variable.
Magnetic resonance imaging (MRI) has greater sensitivity for evaluating leiomyoma size, number, location, and presence or extent of degeneration, but it requires a stable patient and may be difficult to perform in the emergency department [5]. Specifically, the presence of a pedicle between the mass and the uterus and the identification of a necrotic leiomyoma on MRI suggest torsion of a pedunculated leiomyoma. Necrotic leiomyomas have a heterogeneous appearance with hyperintense signal in T2 and hyper-isointense in T1 depending on whether the necrosis is haemorrhagic or ischaemic. After contrast administration, no enhancement is observed due to the interruption of vascular flow. In contrast, non-necrotic or non-degenerated uterine leiomyomas on MRI show hypo-intense homogeneous T2 signals and iso-intense T1 signals [3]. These imaging findings in conjunction with the clinical presentation may raise preoperative suspicion of torsion.
As mentioned above, even with all the imaging modalities, it is very difficult to make an accurate preoperative diagnosis of torsion of a leiomyoma. In our case, the possibility of torsion of a leiomyoma was considered because the leiomyoma was considerably bigger compared with a previous examination and we identified CT signs such as poor contrast enhancement, thin rim enhancement and a dark fan sign which suggested probable torsion. As this case shows, in patients with persistent lower abdominal pain and subserosal leiomyoma, we should consider torsion if the CT scan reveals the above mentioned CT signs.