ABSTRACT
Inferior vena cava syndrome is rare and often difficult to diagnose because of its rarity and consequent low suspicion.
We describe the case of a 28-year-old female patient with a history of nephroblastoma of the right kidney, stage IV, with a favourable histology with epidural metastasis (D5-D9), diagnosed at 3 years of age. The patient underwent treatment with surgery, chemotherapy and radiotherapy.
The patient suffered from sudden low back pain worsening over 2 weeks, with progressive inability to walk. The pain radiated to the front of the thighs. Concomitantly, oedema of the lower limbs with cephalocaudal progression was observed. At admission to our institution, the physical examination showed peripheral oedema, abdominal wall venous collaterals, an inability to walk due to low back pain in the supine position, with no neurological deficits. Lumbar MRI showed exuberant epidural venous congestion. The hypothesis of inferior vena cava thrombosis (IVCT) was considered and confirmed by angio-CT.
IVCT is prevalent in patients with congenital anomalies of the inferior vena cava, occurring in approximately 60–80% of these cases, and most published series on inferior vena cava syndrome refer to thrombotic complications in this subgroup of patients. There are currently no guidelines defined or validated to guide the diagnosis and approach to IVCT. With this case, we would like to draw attention to a rare disease that should be suspected in all patients with inferior vena cava disease, whether resulting from congenital disease or after surgical procedures.
LEARNING POINTS
- Diagnosing IVCT can be challenging and a high index of suspicion is needed in presence of abnormalities of the inferior vena cava.
- In rare instances, IVCT can present with severe lumbar pain due to epidural venous congestion.
KEYWORDS
Thrombosis, inferior vena cava syndrome, lumbar pain, nephroblastoma
INTRODUCTION
Inferior vena cava syndrome (IVCS) is rare and often difficult to diagnose because of its rarity and consequent low suspicion. It is usually suggested by the presence of bilateral oedema and more rarely by low back pain; it may mimic a lumbar hernia and even cauda equina syndrome [1]. Nephroblastoma is the most common childhood abdominal malignancy[2].
We describe the case of a 28-year-old woman with a history of nephroblastoma and a rare surgical complication: cavo-ilio-femoral thrombosis.
CASE DESCRIPTION
We describe the case of a 28-year-old female patient with a history of nephroblastoma of the right kidney, stage IV, with a favourable histology with epidural metastasis (D5-D9), diagnosed at 3 years of age. The patient underwent treatment with surgery (right nephrectomy, inferior vena cava thrombectomy, para-aortic lymphadenectomy, laminectomy and epidural tumour removal), chemotherapy (cumulative doses: ifosfamide 22,500 mg/m2, carboplatin 1380 mg/m2, epirubicin 390 mg/m2 and etoposide 780 mg/m2) and radiotherapy (abdominal - 18 Gy and thoracic spine - 30 Gy). The patient attended regular follow-up oncology appointments until the age of 18 years old. Apart from recurrent episodes of dorsolumbar pain due to scoliosis, the patient had never presented signs of neurological or vascular compromise.
At presentation, she was being medicated with oral contraceptives (gestodene and ethinyl oestradiol).
The patient suffered from sudden low back pain worsening over 2 weeks, with progressive inability to walk. The pain radiated to the front of the thighs. Concomitantly, she experienced oedema of the lower limbs and ecchymoses on the abdomen, thighs and lower back. For this reason, the patient visited the emergency department twice at another institution, where a CT scan of the lumbosacral spine was performed showing no alterations.
The patient reported a 16-day car trip, with prolonged immobilization, that ended one week before the onset of symptoms.
At admission to our institution, the patient presented with a tympanic temperature of 37.8°C, peripheral oedema, the ecchymoses already described, abdominal wall venous collaterals (Fig. 1), an inability to walk due to low back pain in the supine position (numeric pain intensity scale – 10/10), with no neurological deficits or decreased muscle strength.
Figure 1. Abdominal wall and right thigh showing venous collateral circulation
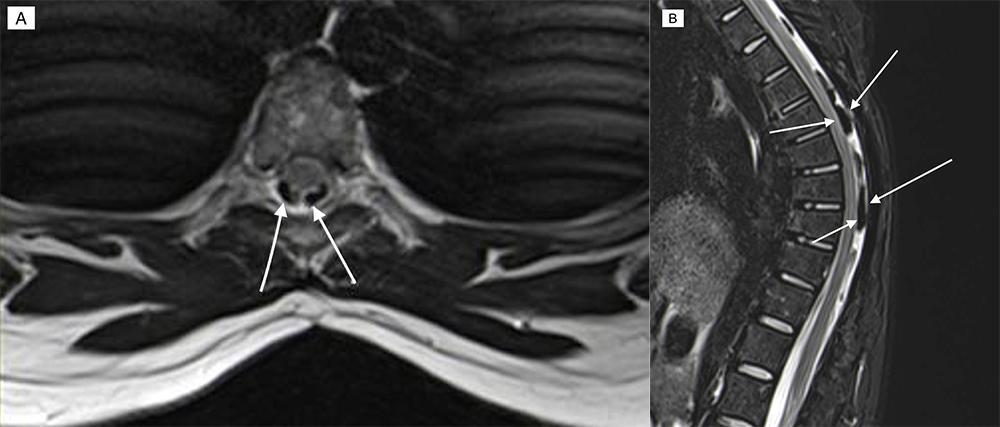
Laboratory analysis showed elevated inflammatory parameters (CRP 137.5 mg/l, ESR 105 mm/min), normochromic normocytic anaemia (Hb 10.5 g/dl), moderate cholestasis (ALP 140 U/L, GGT 163 U/L), elevated LDH (303 U/L) and haemoglobinuria. Lumbar MRI did not show evidence of spondylodiscitis, but densification of the prevertebral fat and exuberant epidural venous congestion (Fig. 2).
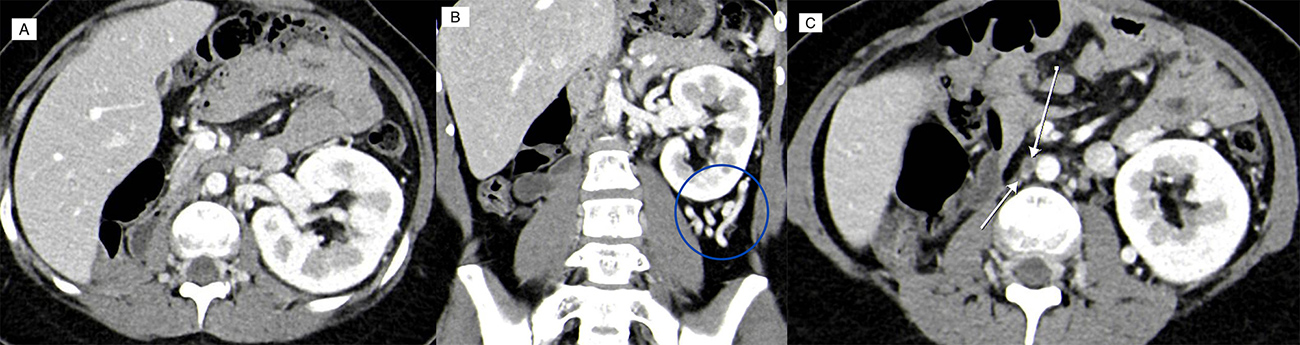
After discussing the case with the Neurosurgery and Neuroradiology departments, a diagnosis of inferior vena cava thrombosis (IVCT) was hypothesized. An abdominal angio-CT scan was performed and an absence of continuity of the inferior vena cava with the suprahepatic veins was identified, as well as dilation and absence of permeability of the inferior vena cava and the common and external iliac veins, with slight surrounding densification attributable to thrombosis; in addition, there was permeability of the left renal vein with venous collateral pathway to the mesenteric vein, as well as through the haemorrhoidal plexus, creating a portosystemic shunt and venous collateral circulation through the azygos system (Fig. 3).
Figure 2. Lumbar spine MRI, axial (A) and sagittal (B), with evidence of epidural venous engorgement (arrows)
Figure 3. Abdominal angio-CT: (A) absence of right kidney and no visualization of inferior vena cava; (B) evidence of multiple tortuous venous structures – portosystemic shunt (circle); (C) inferior vena cava without opacification (arrow)
Once the diagnosis of cavo-ilio-femoral thrombosis was made, anticoagulation therapy was started with low molecular weight heparin (LMWH), with progressive improvement of peripheral oedema and pain complaints, with the ability to walk small distances at the time of discharge.
After 2 months of anticoagulation therapy with enoxaparin, anticoagulation was started with warfarin. After 6 months, the patient presented complete resolution of all complaints and normal laboratory test results.
DISCUSSION
IVCT is prevalent in patients with congenital anomalies of the inferior vena cava, occurring in approximately 60–80% of these cases, and most published series on IVCT refer to thrombotic complications in this subgroup of patients. IVCT in the absence of congenital anomalies is rare, and according to different authors, in addition to an acquired anatomical anomaly of the inferior vena cava or adjacent structures a hypercoagulable state is required[1,3,4].
It presents commonly with pain, oedema, sensation of weight and cramps in the inferior members. In rare instances, paraspinal venous collaterals develop, resulting in severe lumbar pain, sciatica or even cauda equina syndrome, due to the compression of peripheral nerves by dilated veins[1,5].
CT and MRI are essential for the diagnosis, since ultrasound does not always allow a correct visualization of the inferior vena cava [1].
Anticoagulation therapy is the treatment of choice, but there are no specific recommendations to guide anticoagulation management. The most consensual approach is to initiate anticoagulation therapy with an unfractionated heparin or LMWH with conversion to oral therapies such as warfarin[3]. Therapies such as surgical thrombectomy, endovascular or systemic thrombolysis do not yet have well-defined roles in the treatment, with the decision to opt for a more invasive treatment made on a case-by-case basis [1].
Nephroblastomas have an incidence of 10 per 1,000,000 children and adolescents before 15 years of age[2]. The therapy instituted depends on tumour staging, but in most cases treatment involves surgery, chemotherapy and radiotherapy. Advances in therapy have led to a 5-year survival rate of approximately 90%, at the cost of long-term sequelae. IVCT is not described as a comorbidity[2,6,7].
In this clinical case we identify 2 rarities: 1) IVCT as a complication of therapy for nephroblastoma, potentiated by 2 procoagulant factors; the use of oral contraceptives and prolonged immobilization and 2) the less typical presentation with lumbar pain and functional disability which motivated the delay in diagnosis.
There are currently no guidelines defined or validated to guide the diagnosis and approach to IVCT. As this case illustrates, the diagnosis may be challenging due to the lack of specificity and its rare presentation. This case study is intended to highlight a pathology that should be suspected not only in the context of follow-up of patients with a history of nephroblastoma surgery, but in all patients with inferior vena cava disease.
To our knowledge this is the first case in which this association is described.