ABSTRACT
Background: Right heart thrombus (RHT) is a medical condition associated with acute pulmonary embolism and congestive cardiac failure. Rapid recognition is essential for instituting early treatment and preventing adverse outcomes.
Case summary: A 55-year-old male presented with symptoms of congestive cardiac failure complicated by cardiac arrest. Initial transthoracic echocardiography (TTE) demonstrated moderate impairment of both ventricles and a moderately dilated right ventricle (RV). After initial improvement with heart failure treatment, the patient subsequently had a second cardiac arrest. Bedside TTE revealed complete RV obstruction by thrombus, and intravenous thrombolysis was immediately instituted, with complete dissolution of the thrombus and haemodynamic recovery 15 minutes after treatment. Unfortunately, the patient suffered significant hypoxic brain injury and did not survive.
Discussion: RHT can manifest acutely in a dramatic fashion with cardiac arrest. Bedside TTE is key to making a rapid diagnosis in this setting to allow early administration of thrombolytic therapy.
LEARNING POINTS
- Right heart thrombus (RHT) may manifest acutely as cardiac arrest in patients with underlying cardiomyopathy.
- Echocardiography is essential for rapid diagnosis of RHT.
- Thrombolysis can lead to rapid thrombus dissolution and haemodynamic improvement.
KEYWORDS
Case report, right heart thrombus, thrombolysis, heart failure
INTRODUCTION
Right heart thrombus (RHT) represents a medical emergency requiring urgent treatment. Diagnosis of this condition is generally confirmed by two-dimensional transthoracic echocardiography (TTE) [1]. The treatment of RHT varies on a case-wise basis and may include surgical embolectomy, thrombolysis or anticoagulation therapy alone [2]. We report a case of massive RHT leading to cardiac arrest in a patient with underlying cardiomyopathy, with echocardiographic demonstration of rapid clot dissolution after thrombolysis.
CASE DESCRIPTION
A 55-year-old male presented to the emergency department of a regional hospital with scrotal oedema of 2 weeks’ duration. He had a history of hypertension and type 2 diabetes mellitus with associated nephropathy and peripheral vascular disease. Physical examination revealed bilateral leg oedema as well as generalized scrotal swelling with associated erythema and tenderness. The patient was admitted into the surgical unit and treated with intravenous (IV) antibiotics for scrotal cellulitis.
On day 2 of admission, he had a witnessed cardiac arrest whilst getting out of bed. A rhythm check during resuscitation revealed asystole. The patient had return of spontaneous circulation after 15 minutes of cardiopulmonary resuscitation (CPR) and 2 mg of IV adrenaline. He was intubated and subsequently transferred to a tertiary hospital intensive care unit (ICU) for further care.
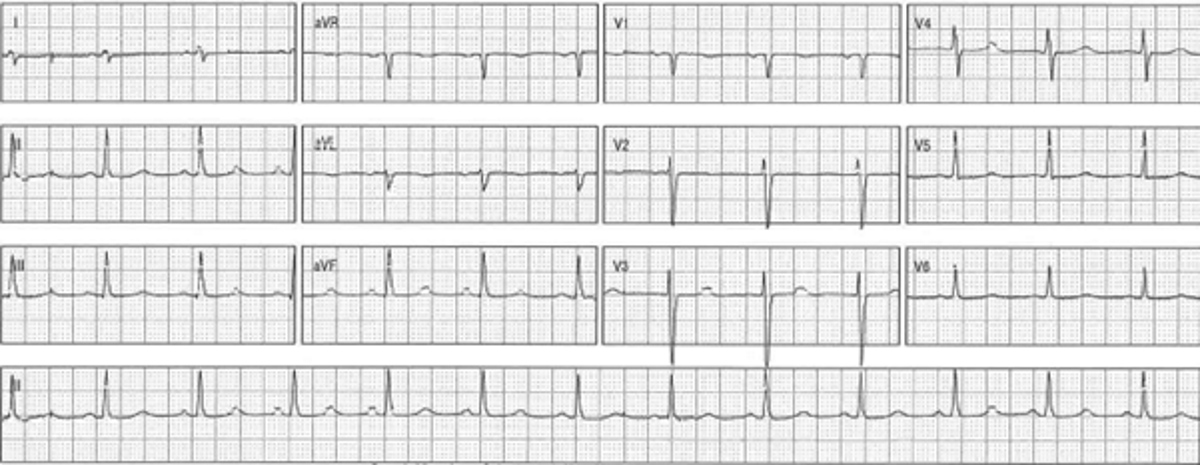
On arrival at the ICU, physical examination revealed dual heart sounds with a pansystolic murmur consistent with mitral regurgitation, bilateral inspiratory crepitations at the lung bases and moderate bilateral pitting oedema to the thighs and scrotum. An electrocardiogram (ECG) showed sinus rhythm, normal QRS morphology, a prolonged QTc interval at 470 ms and no features of ischaemia (Fig. 1).
Figure 1. Electrocardiogram (ECG) at admission showing sinus rhythm with normal QRS morphology and mild QTc prolongation
Serum creatinine was 402 µmol/l, and troponin T was 266 ng/l (normal <14). Chest x-ray revealed cardiomegaly and pulmonary congestion. A transthoracic echocardiogram showed a mildly dilated left ventricle (LV) with moderate impairment of ejection fraction (EF) at 35%, a moderately dilated right ventricle (RV) with moderate impairment of systolic function, moderate mitral regurgitation, mild tricuspid regurgitation and a right ventricular systolic pressure of 49 mmHg. The provisional diagnosis for the patient’s presentation was congestive cardiac failure (CCF) and an arrhythmia secondary to underlying cardiomyopathy, and a decision was made to delay coronary angiography due to the lack of ECG changes and the risks of contrast-induced nephropathy. He was treated with frusemide, hydralazine, and glyceryl trinitrate. He was also given subcutaneous heparin for venous thromboembolism (VTE) prophylaxis.
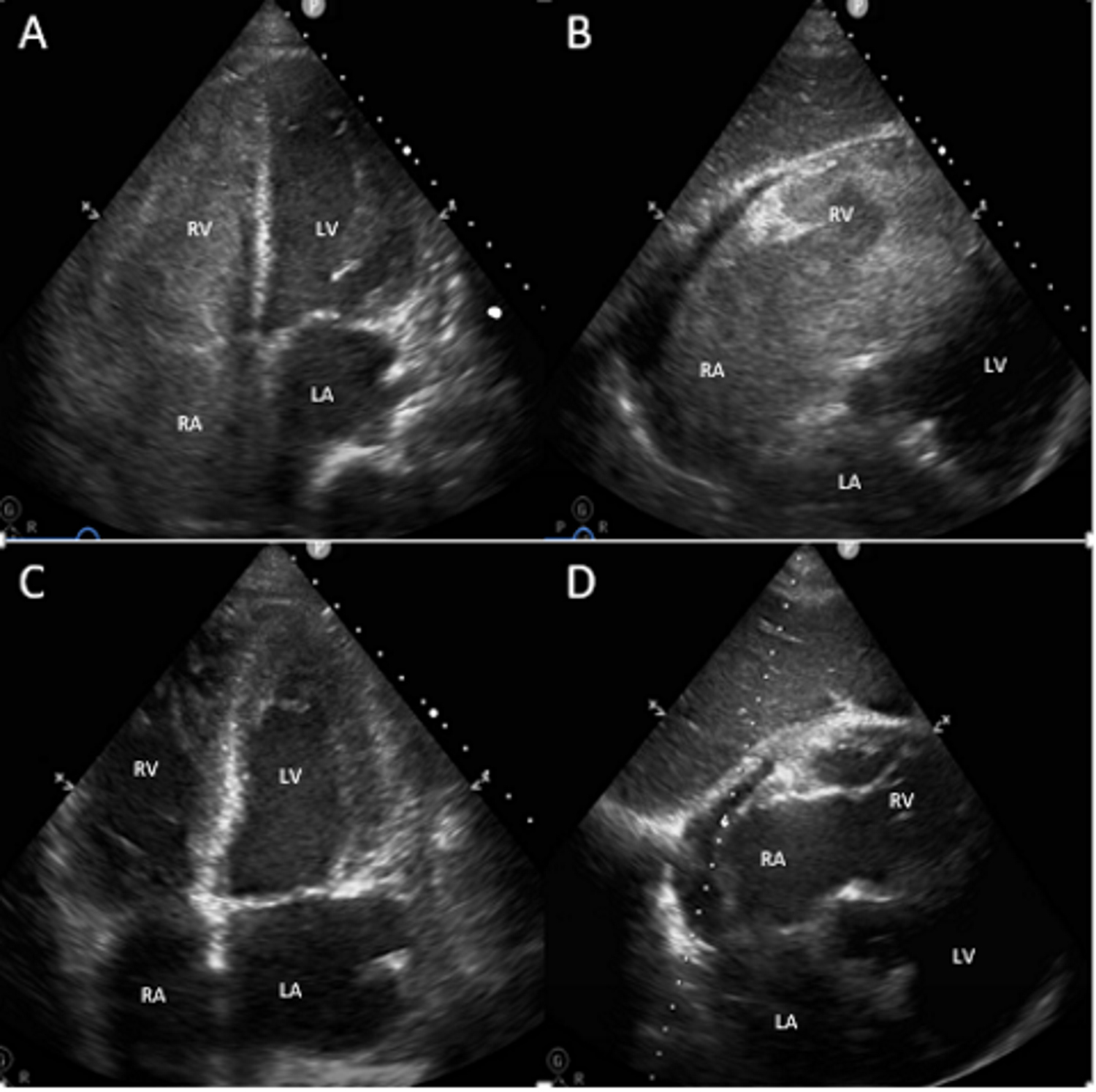
The patient was mildly delirious after extubation on day 3, but subsequently made a full neurological recovery by day 5. Ventilatory status was stable after extubation with oxygen saturation at 98% on room air. He was transferred to the coronary care unit and subsequently had a second cardiac arrest the same night. The initial rhythm was asystole, followed by ventricular fibrillation (defibrillated at 200 J), and intermittent asystole and pulseless electrical activity. After administration of multiple doses of IV adrenaline, intubation and 16 minutes of CPR, a weak carotid pulse was felt, along with a systolic blood pressure of 70 mmHg. An ECG showed sinus rhythm with a PR interval of 260, a normal QTc interval and no ST segment changes suggestive of ischaemia. The on-call cardiology team was contacted to perform emergent bedside echocardiography, which revealed complete occlusion of the RV and right atrium (RA) by thrombus, and severe LV systolic impairment with spontaneous echo contrast in the LV and left atrium (LA) (Figs. 2A and 2B, Videos 1 and 2). Thrombolysis was immediately initiated using IV alteplase, leading to prompt restoration of haemodynamic stability. Repeat TTE performed 15 minutes post-thrombolysis demonstrated complete resolution of the RHT, as well as improvement in both RV and LV systolic function (Figs. 2C and 2D, Videos 3 and 4).
Figure 2. (A) and (B): Complete occlusion of the right ventricular cavity by thrombus and spontaneous echo contrast in the left ventricle. (C) and (D): Resolution of right ventricular thrombus 15 minutes post-initiation of intravenous thrombolysis
Video 1 (click to enlarge)
Video 2 (click to enlarge)
Video 1. Apical 4-chamber view pre-thrombolysis demonstrating complete occlusion of the right heart chambers with severe left ventricular systolic impairment.
Video 2. Subcostal view pre-thrombolysis demonstrating complete occlusion of the right heart chambers with severe left ventricular systolic impairment.
Video 3 (click to enlarge)
Video 4 (click to enlarge)
Video 3. Apical 4-chamber view 15 minutes post-thrombolysis demonstrating complete resolution of right heart thrombus with improvement in left ventricular systolic function.
Video 4. Subcostal view 15 minutes post-thrombolysis demonstrating complete resolution of right heart thrombus with improvement in left ventricular systolic function.
A bilateral venous duplex study was performed to investigate a potential source of the RHT. This showed hypoechoic acute and occlusive thrombus in the posterior tibial and soleal veins of the right leg, and hypoechoic acute thrombus in the peroneal and soleal veins of the left leg. The proximal leg veins and the inferior vena cava were free of thrombus. Unfortunately, the second cardiac arrest resulted in brain death, which was confirmed by clinical examination and cerebral scintigraphy with single photon emission computed tomography. After discussion with the patient’s family, the decision was made to withdraw ongoing invasive ventilatory and inotropic support. The patient died shortly thereafter.
DISCUSSION
RHT is a relatively uncommon finding in patients with CCF and VTE. Two major subtypes of RHT have been described, each with distinct morphology and pathophysiology. Type A thrombi are mobile and snake-like in appearance, representing thrombus in transit after embolization from the lower extremity veins. Type B thrombi are immobile and flat in appearance, representing in situ formation from predisposing cardiac abnormalities such as cardiomyopathy [3].
Patients with CCF have activation of both platelets and the coagulation system, increasing their propensity for thromboembolism [4]. The association between VTE and heart failure has been well described, with studies showing a greater than two-fold increase in the risk of pulmonary embolism (PE) in patients hospitalized with CCF [5]. Similarly, patients with both PE and RHT are significantly more likely to have a history of CCF compared to PE patients without RHT. The presence of RHT is a predictor of increased mortality in patients with acute PE. Data from the International Cooperative Pulmonary Embolism Registry showed that RHT was associated with haemodynamic instability and significantly increased 14-day mortality (21% vs 11%) [6].
The treatment of RHT remains controversial. A meta-analysis of 119 patients with RHT assigned to surgery, thrombolysis or heparin alone demonstrated similar mortality rates amongst the surgery and thrombolysis groups, and slightly improved mortality in the heparin only group. However, a lack of randomized comparison of different treatments did not allow a firm conclusion to be drawn regarding the optimal management of RHT [7].
To the best of our knowledge, this is the first reported case of a massive RHT causing complete obstruction of the right-sided chambers, with echocardiographic demonstration of rapid resolution post-thrombolysis. The thrombus size and morphology were unusual in this case, and did not conform to the classic appearance of either type A or type B RHT described in the literature. RHT in this case may represent either in situ thrombosis from stasis secondary to cardiomyopathy, or embolization of a massive thrombus from the deep pelvic veins. Although the cause of the patient’s initial presentation was thought to be due to an arrhythmia secondary to underlying cardiomyopathy, in retrospect it is feasible that the first cardiac arrest represented the manifestation of massive VTE. However, the lack of other suggestive signs of PE including tachycardia, hypoxaemia or ongoing hypotension made this diagnosis a less likely consideration on the initial differential list. We postulate that RHT in this case was more likely to be secondary to stasis given the shape of the thrombus, as well as the patient’s presentation with biventricular CCF. An underlying superimposed thrombophilia may also have accounted for the massive thrombus.
Our case highlights three important learning points. First, a concurrent diagnosis of VTE should be entertained in a patient presenting with cardiac arrest and an underlying cardiomyopathy. Second, it illustrates the importance of having echocardiography-trained staff on the resuscitation team, as a prompt diagnosis may have led to a better outcome in this case. Third, IV thrombolysis can lead to rapid clot lysis and haemodynamic improvement in RHT, and should be administered as a matter of priority in an unstable patient once the diagnosis is established.