ABSTRACT
Introduction: Twenty-five per cent of tuberculosis patients have pleural tuberculosis, which is the third most common form of presentation. Most cases present as an exudative pleural effusion with just few cases reported as chylothorax in the literature. All pleural effusions from confirmed cases, including tuberculous chylothorax, had exudate features.
Aim: To describe a patient with Mycobacterium tuberculosis affecting the lungs and pleura, which laboratory testing demonstrated had features of transudate chylothorax.
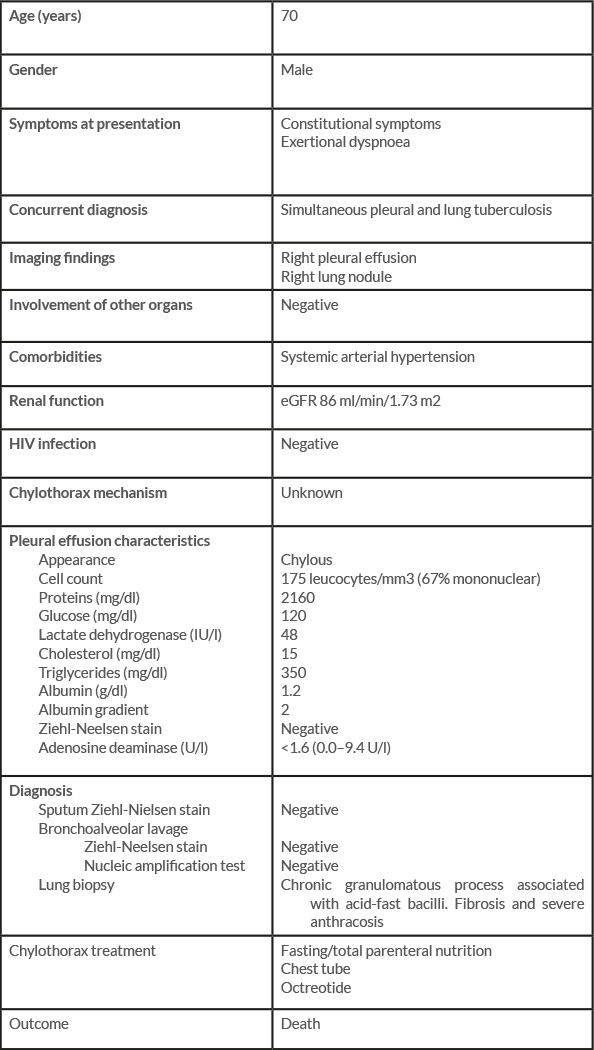
Patient and methods: A 70-year-old man presented with constitutional symptoms, progressive exertional dyspnoea and right pleural effusion with fibrocavitary changes on chest imaging. Thoracentesis and pleural fluid analysis revealed chylous fluid with transudate features, high triglycerides, low cholesterol content and mononuclear cell predominance. Acid-fast sputum stains and pleural fluid were negative for Mycobacterium tuberculosis as was an adenosine deaminase test for pleural effusion. Tomography-directed lung biopsy sampling of a lung nodule revealed a chronic granulomatous inflammatory process associated with the presence of acid-fast bacilli.
Discussion: Tuberculosis-associated chylothorax is an uncommon presentation of the disease. A recent review found only 37 cases of confirmed tuberculous chylothorax had been reported in the literature. All cases had exudate characteristics. The diagnosis of pleural tuberculosis was made through culture or testing of sputum, pleural fluid or biopsy samples in 72.2% of cases, with the rest identified by histopathology.
LEARNING POINTS
- The main cause of non-traumatic chylothorax is malignancy, which is found in 39–72% of cases.
- Few cases of transudative chylothorax have been reported in the literature; the main aetiology is chronic hepatopathy.
- Tuberculosis-associated chylothorax is a rare presentation of infection caused by Mycobacterium tuberculosis, an uncommon aetiology.
KEYWORDS
Chylothorax, Mycobacterium tuberculosis, pleural tuberculosis, pleural effusion
CASE DESCRIPTION
A 70-year-old man was referred to the emergency department due to progressive exertional dyspnoea. He had a 2-month history of constitutional symptoms, but denied weight loss, diaphoresis, cough, pleuritic pain or haemoptysis. He had been diagnosed with systemic arterial hypertension 20 years previously, which was treated with calcium antagonists. Physical examination revealed dullness to percussion, decreased tactile fremitus and diminished breath sounds in the right hemithorax.
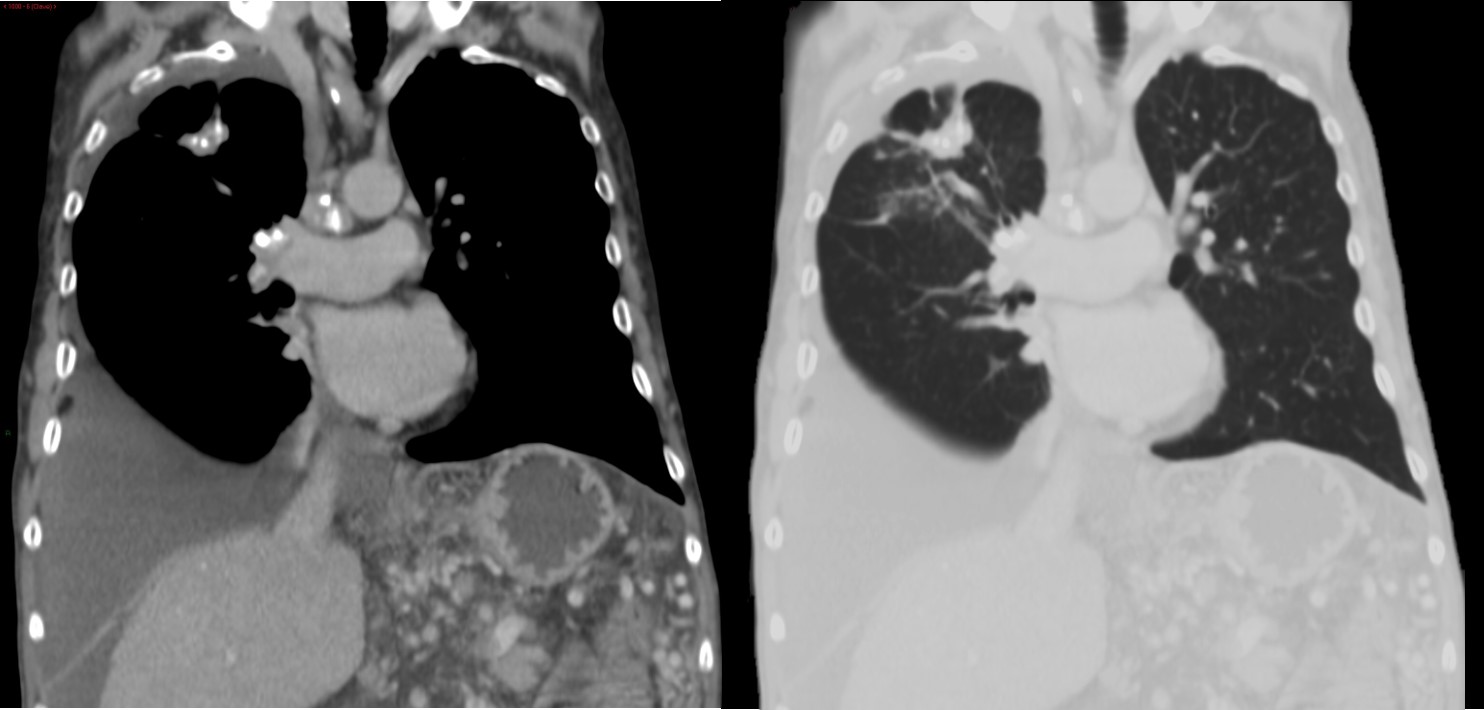
Radiography and contrast tomography of the lungs demonstrated right pleural effusion, chronic granulomatous lung disease and calcified mediastinal adenopathies (Fig. 1).
Figure 1. Left image: chronic pulmonary granulomatous disease with calcified mediastinal adenopathies; right image; pleural effusion
Thoracentesis and pleural fluid analysis demonstrated a chylous-appearing liquid with a lactic dehydrogenase ratio of 0.24, protein ratio 0.24, albumin gradient 2 g/dl, triglycerides 350 mg/dl, total cholesterol 15 mg/dl, and 175 leucocytes/mm3 with mononuclear cell predominance.
Acid-fast sputum stains and pleural fluid were negative as was a pleural effusion adenosine deaminase test. Bronchoalveolar lavage and a biopsy specimen obtained with flexible bronchoscopy were negative for Ziehl–Neelsen and periodic acid–Schiff staining. Tissue culture was also negative. Tomography-directed lung biopsy sampling of a lung nodule revealed a chronic granulomatous inflammatory process associated with acid-fast bacilli, confirming the diagnosis of chylothorax transudate associated with pulmonary tuberculosis (Table 1).
Treatment for the chylothorax consisted of nil-per-mouth, total parenteral nutrition and thoracostomy catheter drainage of approximately of 3 litres per day of chylothorax fluid at the beginning with progressive reduction. Antituberculous treatment was initiated at diagnosis but the patient died a few weeks later from secondary ventilatory insufficiency.
DISCUSSION
Malignancy is the main cause of non-traumatic chylothorax, being present in 39–72% of cases [1]. Tuberculosis-associated chylothorax is an uncommon presentation of the disease. Most cases of pleural tuberculosis present similarly to pleural effusion with exudate features with lymphocytic predominance [2].
A recent review described only 37 cases of confirmed tuberculous chylothorax reported in the literature. All cases had exudate characteristics, with a mean protein of 4.70 g/dl and an average lactate dehydrogenase of 177 IU/l. The diagnosis of pleural tuberculosis was confirmed in 72.2% by culture or testing of sputum, pleural fluid or biopsy samples, with the rest identified by histopathology. The pathogenesis of the chylothorax was described as secondary to mediastinal lymphadenopathy in 51% of cases, followed by abdominal lymphadenopathy (14.3%) and extensive pleural disease (14.3%) [3].
Tuberculosis-associated chylothorax with transudate features has not been previously described in the literature. Compared with reported patients, we found lower cholesterol and adenosine deaminase, in addition to lower levels of protein and lactate dehydrogenase.