ABSTRACT
Background: Coccidioidomycosis is an endemic disease in the Americas. No cases have been reported in Africa.
Patient: A 23-year-old HIV seronegative Ugandan man was referred to Mulago National Referral Hospital in Kampala, Uganda with a 10-month history of haemoptysis and difficulty breathing, and a 6-month history of localized swellings on the extremities. He had associated weight loss and drenching sweats, but no fevers. He had taken anti-tuberculosis medicine for 2 months with no improvement. He had never travelled out of Uganda. On physical examination, he had cystic swellings and ulcerated lesions on the extremities. He had tachypnoea, crackles in the chest and mild hepatomegaly. Bronchoscopic examination showed two masses occluding the right main bronchus. Bronchoscopic biopsy showed findings consistent with coccidioidomycosis. The patient improved with antifungal treatment and was discharged.
Conclusion: We report the first case of disseminated coccidioidomycosis with pulmonary and cutaneous manifestations in Africa.
LEARNING POINTS
- Coccidioidomycosis is an endemic disease in the Americas and may now be present in Africa.
- IThe patient had taken anti-tuberculosis medicine for 2 months with no improvement.
- Coccidioidomycosis should be considered in the differential diagnosis of tuberculosis.
KEYWORDS
Coccidioidomycosis, bronchial mass, endemic disease, tuberculosis
BACKGROUND
Coccidioidomycosis is endemic in desert regions of the southwestern United States, Central America and South America. Although this infection has been reported outside of America, such cases were imported by travellers who had visited endemic areas [1–3]. Disseminated coccidioidomycosis occurs mostly in immunocompromised hosts, and may develop weeks, months or years after the primary infection [4]. Here we report a patient with disseminated coccidioidomycosis in Uganda who has no evidence of immunosuppression and has no history of travel to a coccidioidomycosis endemic area.
CASE DESCRIPTION
A 23-year-old male Ugandan nursing student was referred from a local hospital to Mulago National Referral and Teaching Hospital in Kampala, Uganda with a 10-month history of haemoptysis and difficulty breathing, and a 6-month history of swellings on the extremities. He had associated weight loss (from 53 kg to 41 kg over 10 months), drenching sweats and arthralgia, but no fevers. He had been given treatment for tuberculosis for 2 months with no improvement. He had never travelled out of Uganda, and had no history of receiving gifts from abroad. He had no history of other chronic illnesses that may cause immune suppression.
Physical examination revealed a young, sick-looking man who was wasted, with a tinge of jaundice and no lymphadenopathy. He had cystic swellings on the right shoulder, right upper arm and right thigh, and ulcerated lesions near the medial malleoli bilaterally (Fig. 1). He had tachypnoea of 24 breaths/min, and crackles in the right infra-axillary and infra-scapular area with hepatomegaly of 3 cm below the costal margin.
Figure 1. Swelling on the thigh and skin ulceration near a medial malleolus
Results of serological testing were negative for HIV infection and hepatitis B surface antigen. The haemogram showed leucocytosis (18.5×106) with neutrophilia (81%) and eosinophilia (6.1%). Liver function tests showed direct bilirubinemia (4 times the upper limit of normal) with an increased gamma-glutamyl transpeptidase level (2.5 times the upper limit of normal). Sputum stain for AFB was negative.
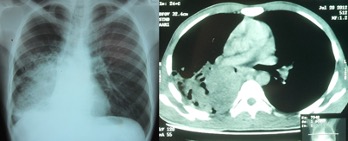
Chest radiography showed diffuse consolidation in the right mid and lower lung zones. A chest CT scan revealed heterogeneous mass-like consolidation with areas of low attenuation and cavities that obstructed the bronchus intermedius in the posterior segment of the right upper lobe and the entire segment of the right lower lobe (Fig. 2).
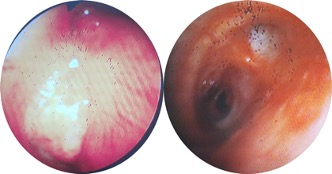
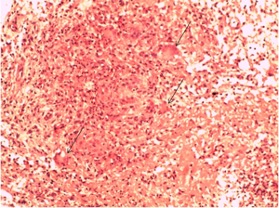
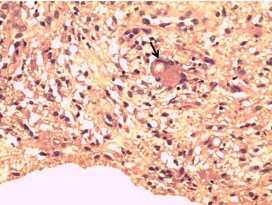
A bronchoscopic examination showed two masses that occluded the right upper lobe bronchus and intermedius (Fig. 3). Bronchoscopic biopsy showed granulomatous inflammation associated with multinucleated giant cells with mixed inflammatory cellular infiltrate in the background. The multinucleated giant cells contained ingested large spherules suggestive of coccidioidomycosis (Figs. 4 and 5).
Figure 2. Chest x-ray (PA view) and CT images
Figure 3. Bronchoscopic findings before and after treatment. Note the reopening of the right lower lobe bronchus
Figure 4. Histological finding. Haematoxylin & eosin-stained section showing granulomatous inflammation associated with numerous multinucleated giant cells (arrows)
Figure 5. Histological findings. Periodic acid–Schiff (PAS)-stained section showing a multinucleated giant cell (arrow) containing an ingested single large spherule. Note the thick refractive wall
Intravenous amphotericin B deoxycholate 0.7 mg/kg was given for 10 days daily and followed by oral itraconazole 200 mg/day. The patient showed clinical improvement (haemoptysis, difficulty breathing and night sweats all resolved) following treatment and was discharged.
One month after discharge, the skin lesions had healed with scar formation. A follow-up bronchoscopy revealed reopening of the airways with the masses markedly reduced in size. At the 2-month follow-up visit, the patient had regained much of his weight (50 kg).
DISCUSSION
Coccidioidomycosis is acquired via inhalation of the dimorphic fungi Coccidioides (C. immitis and C. posadasii) from the soil. The incidence of coccidioidomycosis outside the Americas is extremely low, and case reports from Asia and Europe have been shown to be imported disease through travel to endemic areas [1–3]. No cases of either indigenous or imported coccidioidomycosis have apparently been reported from Africa so far. The patient in our case report had neither travelled out of Uganda nor received a gift from abroad. This may be the first report of indigenous coccidioidomycosis in Africa.
We consider that coccidioidomycosis does exist in Africa, but had not yet been reported because of failures in diagnosis. It can be misdiagnosed as other infections that have similar clinical symptoms and signs. Our patient was misdiagnosed as having pulmonary tuberculosis and took anti-tuberculosis medicine for 2 months.
Disseminated coccidioidomycosis has commonly been seen in immunocompromised subjects, but our patient had no evidence of immunosuppressive conditions such as HIV infection, diabetes mellitus or malignancy.
Since we were unable to carry out serological tests for coccidioidomycosis, another fungal infection, especially blastomycosis, may still be a differential diagnosis for our patient. However, the histological findings (H&E staining) showed granulomatous inflammation associated with multinucleated giant cells containing empty spherules in a suppurative background that may be pathognomonic of coccidioidomycosis [5].
CONCLUSIONS
We report the first case of disseminated coccidioidomycosis in Africa, with pulmonary and cutaneous manifestations. The patient was misdiagnosed as having pulmonary tuberculosis and his condition worsened despite anti-tuberculosis medicine.
Coccidioidomycosis should be considered in the differential diagnosis of patients suspected of having pulmonary tuberculosis in Africa.
adenoma, triple assessment, including core biopsy, is the mainstay of diagnosis.