ABSTRACT
We continue to learn about cardiac involvement in patients with COVID-19. These patients can develop acute coronary syndrome and severe myocarditis with a reduced ejection fraction. We describe two critically ill COVID-19 patients who developed ST elevation that resolved on repeat ECG without any intervention.
LEARNING POINT
- ST elevation may occur in critically ill COVID-19 patients.
KEYWORDS
ST segment elevation, COVID-19
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is the result of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. Cardiac involvement in COVID-19 is being increasingly recognized and may indicate a poor outcome [2]. While patients with COVID-19 can develop acute coronary syndrome, ST segment elevation on electrocardiogram (ECG) has been mainly described in patients with COVID-19-related acute myocarditis and severely reduced left ventricular ejection fraction (LVEF) [2–5]. We describe two cases of transient ST segment elevation in patients with preserved LVEF. Our goal is to raise awareness of this aspect of cardiovascular involvement in COVID-19 and prevent unnecessary catheterization.
CASE DESCRIPTION
Case 1
A 64-year-old male patient with a medical history of hypertension and hyperlipidaemia presented to the emergency room with a 3-day history of dyspnoea. His blood pressure at presentation was 85/51 mmHg, heart rate was 80 beats per minute, respiratory rate was 36 breaths per minute and oxygen saturation was 70% on room air. The patient was intubated, mechanically ventilated, started on norepinephrine for hypotension and admitted to the medical intensive care unit (MICU). The patient’s chest x-ray is shown in Fig. 1.
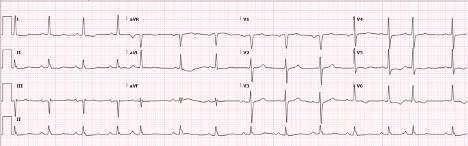
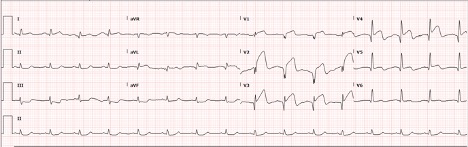
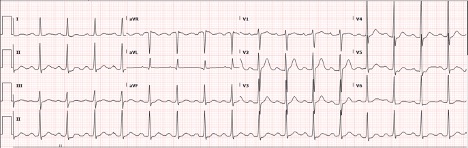
A baseline ECG showed non-specific T wave changes but did not demonstrate acute ischaemic changes or arrhythmia (Fig. 2). The patient’s baseline troponin was 0.17 ng/ml. On day 2 of hospitalization, the patient’s hypoxia worsened, requiring maximum ventilatory support and sedation. A repeat ECG showed ST segment elevation i\n leads I, aVL and V1–V4 and reciprocal ST depression in leads II, III and aVF (Fig. 3).
Due to the patient’s life-threatening respiratory failure, it was decided not to pursue reperfusion therapy. After administration of loading doses, aspirin 81 mg, clopidogrel 75 mg and a heparin drip were initiated. The patient’s other medications included azithromycin, hydroxychloroquine, meropenem, tocilizumab, norepinephrine, phenylephrine, vasopressin, atracurium, propofol and fentanyl.
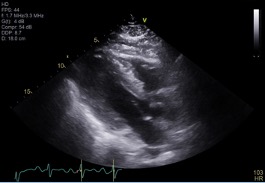
A transthoracic echocardiogram (TTE) showed a vigorous ejection fraction of 70–75% with no regional wall motion abnormalities (Fig. 4).
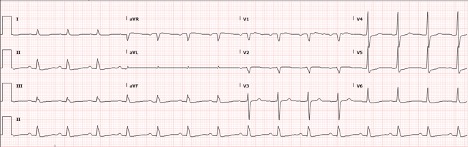
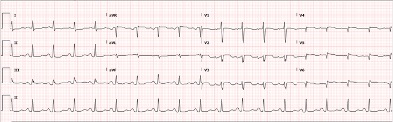
Repeat troponins obtained 6 hours apart were 0.056 ng/ml, 0.123 ng/ml and 0.11 ng/ml, respectively. A repeat ECG after 12 hours showed resolution of the ST elevation (Fig. 5). Unfortunately, patient did not recover and died 24 hours later.
Figure 1. Chest x-ray of male patient showing diffuse opacities bilaterally, consistent with acute respiratory distress syndrome
Figure 2. Baseline ECG showing non-specific T wave changes but no ST segment elevation
Figure 3. ECG showing ST segment elevation in leads I, aVL and V1–V4, and reciprocal ST depression in leads II, III and aVF
Figure 4. Transthoracic echocardiogram (parasternal long-axis view) showing an ejection fraction of 70–75% with no regional wall motion abnormalities
Figure 5. Repeat ECG after 12 hours showing resolution of ST elevation without any intervention
Case 2
A 71-year-old female patient with a medical history of multiple myeloma treated with bortezomib, was admitted with a 1-day history of fever, cough and dyspnoea. She tested positive for SARS-CoV-2. Her initial ECG at presentation is shown in Fig. 6.
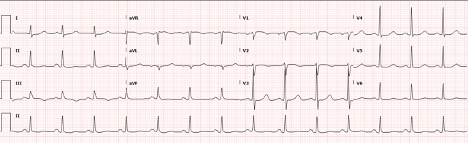
On day 2 of admission, the patient became acutely hypotensive and hypoxic with a blood pressure of 70/41 mmHg, a heart rate of 125 beats per minute, a respiratory rate of 33 breaths per minute and oxygen saturation of 70% on 4 l/min of oxygen by nasal cannula. Her chest x-ray showed bilateral alveolar and interstitial opacities (Fig. 7). She was intubated, initiated on mechanical ventilation and transferred to the MICU for further treatment including vasopressor support. A repeat ECG showed new 1 mm ST elevation in leads V2–V6 with associated Q waves in leads V4–V6 (Fig. 8).
Again, due to the patient’s life-threatening respiratory failure, it was decided not to pursue reperfusion therapy. After completing loading doses, she was started on aspirin 81 mg, clopidogrel 75 mg and a heparin drip. Her other medications included azithromycin, cefepime, vancomycin, tocilizumab, norepinephrine, phenylephrine, midazolam and fentanyl. A TTE showed an ejection fraction of 65–70% with no regional wall motion abnormalities (Fig. 9).
The patient’s baseline troponin of 1.6 ng/ml declined to 1.5 ng/ml after 6 hours and then to 1.1 ng/ml after another 6 hours. A repeat ECG after 12 hours showed complete resolution of the ischaemic changes (Fig. 10). Patient was still on mechanical ventilation at the time of writing.
Figure 6. Initial ECG showing first-degree heart block but no ST changes suggestive of ischaemia
Figure 7. Chest x-ray of female patient showing bilateral diffuse lung opacities consistent with acute respiratory distress syndrome
Figure 8. Repeat ECG showing new 1 mm ST elevation in leads V2–V6 with associated Q waves in leads V4–V6
Figure 9. Transthoracic echocardiogram (long-axis view) showing ejection fraction of 65–70% with no wall motion abnormalities
Figure 10. Repeat ECG after 12 hours showing resolution of ST elevation
DISCUSSION
We describe two cases of transient ST elevation on ECG in patients with normal left ventricular (LV) function and COVID-19. All previously described cases of COVID-19-related ST elevation involved patients with fulminant myocarditis and a severely reduced LV ejection fraction [2–5]. These cases add to our understanding of cardiac involvement in active COVID-19, especially given the uncertainty in proceeding with invasive coronary angiography and the need to balance staff exposure with patient benefit [6].
Possible explanations for the findings in our patients include focal myocarditis from SARS-CoV-2 infection or a type 2 myocardial infarction from severe hypoxia and hypotension [4, 5]. Acute coronary syndrome type 1 also remains a possibility given the systemic proinflammatory stimulation and hypercoagulability in patients with acute COVID-19 [7]. Management of patients should be based on a multidisciplinary approach and any reperfusion therapy should follow the guidelines of the American College of Cardiology's Interventional Council and the Society of Cardiovascular Angiography and Intervention [6].