ABSTRACT
Wellens syndrome (WS) is identified by ECG changes in the precordial leads after resolution of angina chest pain. WS indicates critical stenosis of the proximal left anterior descending (LAD) artery. On the other hand, Kounis syndrome (KS) is an allergic reaction to various substances resulting in acute coronary syndrome. Contrast media can trigger the allergic reaction associated with KS. We describe a patient with WS who developed an allergic reaction to contrast media after percutaneous coronary intervention and experienced recurren myocardial infarction on re-exposure.
LEARNING POINTS
- Despite its rarity, physicians and radiologists should be aware of Kounis syndrome triggered by contrast media so it can be rapidly diagnosed and treated.
- The initial target of the prevention and treatment of KS is avoidance of the precipitating stimulus or allergen.
- There are three KS variants: angina due to allergic coronary spasm, allergic myocardial infarction and allergy-induced stent thrombosis.
KEYWORDS
Contrast media, Kounis syndrome, Wellens syndrome
INTRODUCTION
Allergic acute coronary syndrome is a rare condition caused by activation of mast cells in response to stimuli, followed by the release of inflammatory cytokines, which can lead to coronary spasm and/or destabilization of atheromatous coronary artery plaque and subsequent plaque rupture compromising coronary flow. The hypersensitivity can be to various agents and materials, including contrast. In our case, initial exposure to contrast media manifested as a skin reaction, while re-exposure led to recurrent myocardial infarction with a subsequent significant reduction in myocardial systolic function necessitating insertion of an implantable cardioverter defibrillator (ICD).
CASE DESCRIPTION
A 60-year-old male patient, with a 5-year history of hypertension, presented to the emergency department (ED) with a 2-day history of intermittent chest pain. His chest pain was mainly related to effort but the last episode had occurred while he was almost stationary. He was on lisinopril 10 mg once daily. He had no history of coronary artery disease or allergic reactions. His chest pain improved gradually in the ED and his first electrocardiogram (ECG) was normal. Troponin I was within the normal range. After admission he remained free of chest pain.
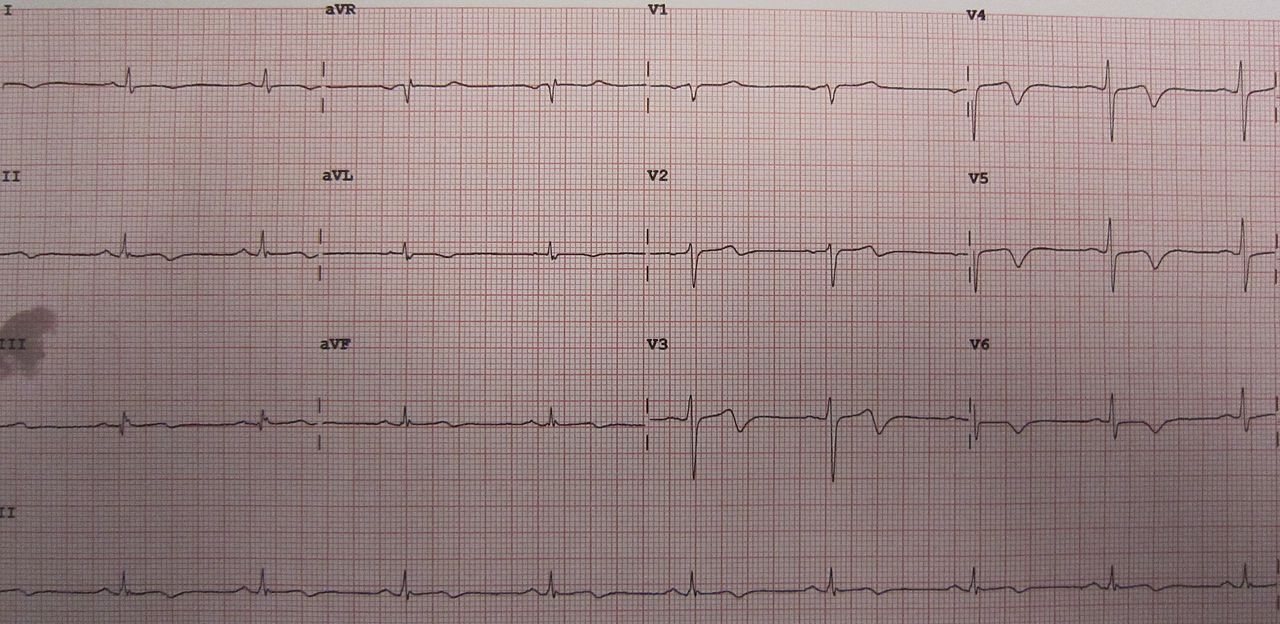
However, follow-up ECG was significant for a new biphasic T wave in precordial leads V2–V5, and an inverted T wave in V6, and leads I and AVL (Fig. 1).
Figure 1. Biphasic T wave inversion in precordial leads suggestive of Wellens syndrome
Troponin I remained normal on follow-up. The combination of angina and the characteristic ECG findings when the patient was free of chest pain suggested Wellens syndrome type II, which indicated critical stenosis of the proximal left anterior descending (LAD) artery. The patient underwent coronary angiography and the stenosis was treated with a drug-eluting stent. A few hours after percutaneous coronary intervention (PCI), the patient developed a generalized itchy maculopapular rash with no sign of respiratory compromise. The rash was diagnosed as an allergic reaction to contrast and was treated with antihistamine and steroid with a good response. After 2 days patient was
discharged home on dual antiplatelet therapy, bisoprolol 2.5 mg and atorvastatin 80 mg once daily.
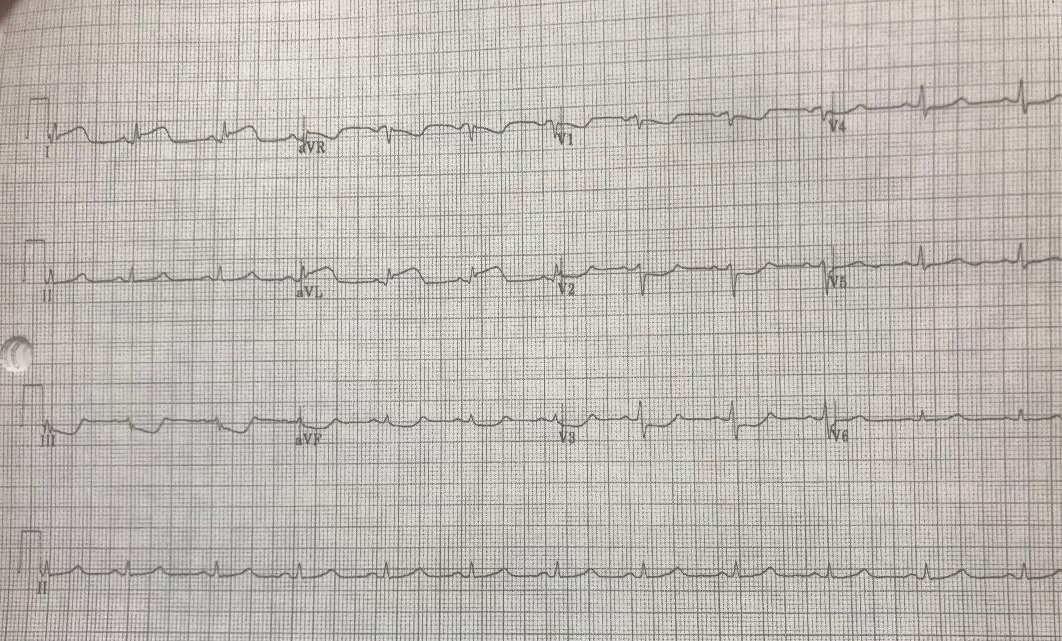
One week later, the patient presented to the ED with back pain and chest pain. His ECG showed no new changes since the last visit and cardiac enzymes were also normal. The patient had taken all prescribed dual antiplatelet therapy since his previous hospital discharge. To rule out aortic dissection, the patient underwent aortography computed tomography (CT) after receiving antihistamine and steroid according to the radiology protocol for contrast reaction. No evidence of aortic dissection was found. However, 20 minutes after aortography, the patient developed severe chest pain with stable haemodynamics but his ECG showed ST segment elevation in leads I and AVL (Fig. 2).
Figure 2. ST elevation in leads I and AVL, and ST depression in leads III, AVF and V1–V3
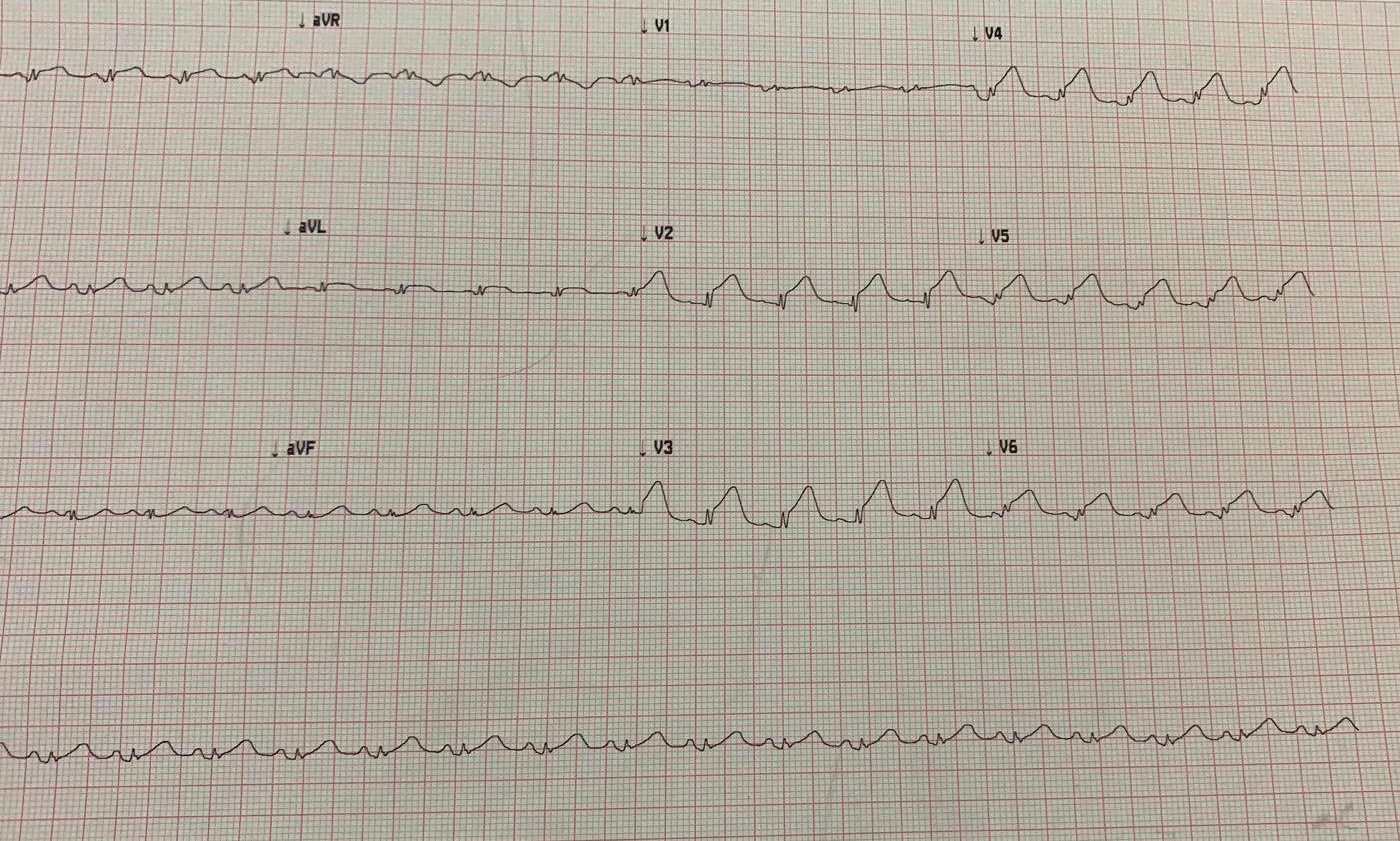
He was admitted to the critical care unit where echocardiography showed hypokinesia of the antero-lateral wall. As Kounis syndrome (KS) was suspected, thrombolytic therapy was administered to avoid contrast exposure during PCI. Gradually, the chest pain improved, and ECG showed good resolution of ST segment elevation. A few hours later, the patient developed severe chest pain and ECG showed extensive ST elevation in precordial leads (Fig. 3) with akinesia of the left ventricle in LAD territory on echocardiography.
Figure 3. Extensive ST elevation in precordial leads V2–V5, and leads I and AVL
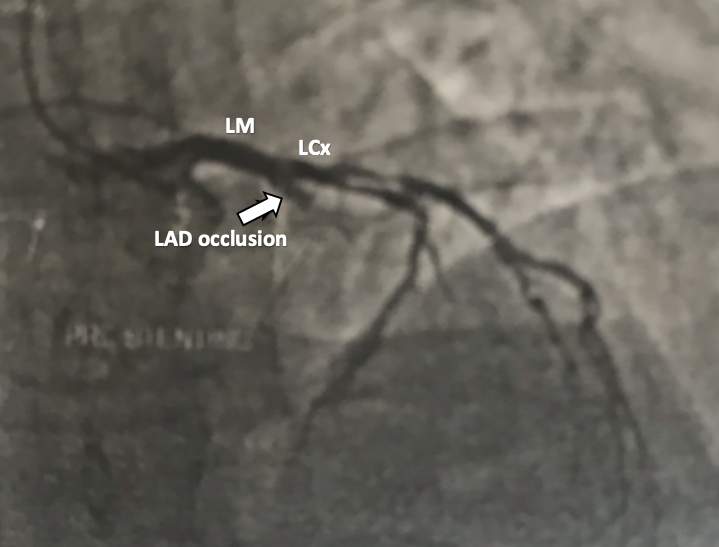
Although contrast-related KS was highly suspected, and re-exposure to contrast carried a higher risk of anaphylaxis, PCI had to be carried out since ST segment elevation was persistent with chest pain. Following antihistamine and steroid administration, coronary angiography showed acute stent thrombosis with total occlusion of the proximal LAD (Fig. 4). Thrombus aspiration was performed followed by angioplasty with a resulting TIMI 3 flow (Fig. 5). There were no more episodes of chest pain and skin manifestations were minimal. The patient was discharged home after a few days.
Figure 4. Coronary angiography (left anterior oblique and cranial view) revealing left anterior descending (LAD) artery occlusion due to stent thrombosis (arrow)
LCx, left circumflex artery; LM, left main coronary artery
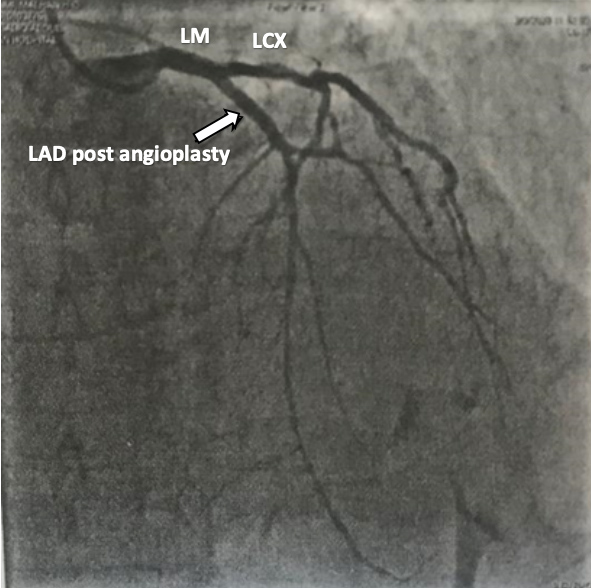
Figure 5. Coronary angiography (left anterior oblique and cranial view) revealing TIMI
3 flow in the proximal left anterior descending (LAD) artery after angioplasty (arrow)
LCx,left circumflex artery; LM, left main coronary artery
After 3-month echocardiography showed evidence of ischaemic dilated cardiomyopathy with an ejection fraction (EF) of 25%, an ICD was inserted to protect against sudden cardiac death.
DISCUSSION
Angina of vasospastic and non-vasospastic origin can develop secondary to an allergic or hypersensitivity reaction to different substances and results in a rare manifestation called Kounis syndrome [1]. It was first described as an allergic angina by Nicholas Kounis in 1991 [2]. A review in 2017 reported 130 men and 45 women with the condition, which makes the disorder rare, but these numbers are thought to be an underestimation.
Exposure to different substances such as medicines (antibiotics, NSAIDs), contrast media, bee stings or food [3] provokes an allergic reaction with a subsequent degranulation cascade of mast cells with the release of different inflammatory mediators, a variety of cytokines and chemokines. Acute coronary syndrome in the setting of an allergic reaction is caused by the action of these mediators and cytokines resulting in either coronary spasm and/or instability of a coronary plaque with subsequent rupture and thrombus formation, which leads to coronary flow compromise [3, 4]. Histological findings of infiltration by mast cells, eosinophils and other cells in coronary plaque [5] indicates released mediators and cytokines have a negative effect on coronary arteries and their lesions, However, the precise nature of the pathophysiological mechanism of KS remains unclear.
A review of the literature revealed only 11 cases of KS related to contrast media, five of which were associated with coronary angiography with the rest occurring during intravenous injection of contrast in the radiology department [6]. A well-established history of allergy has been reported in only a quarter of patient with KS [7].
KS can produce a similar picture of ST elevation myocardial infarction in patients with and without coronary artery disease. Consequently, three types of KS are recognized [8]. Type I is usually associated with a pure coronary spasm as a response to an allergic insult in a patient without coronary artery disease, which can lead to myocardial infarction with positive cardiac markers or coronary spasm with normal cardiac markers. Type I is manifested by endothelial dysfunction or microvascular angina [9]. In a patient with pre-existing coronary artery disease, the allergic insult may cause erosion and rupture of a coronary plaque with subsequent thrombus formation and total occlusion of
the artery, which is the characteristic sign of KS type II. Type III is distinguished by coronary artery stent thrombosis in response to an allergic insult.
KS can be challenging to diagnose and treat. It is usually diagnosed by retrospective clinical analysis, especially in the absence of definitive markers, although some research has suggested serum measurement of inflammatory mediators to identify the allergic component in acute coronary syndrome.
The main aim of KS treatment is to halt the allergic reaction and restore coronary flow. By reducing inflammatory cytokine production, agents such as steroids, adrenaline and antihistamines can improve vasospasm and decrease the effect of inflammatory cytokines on
vulnerable coronary plaque [10]. Nitrates and calcium channel blockers in addition to steroids and H1/H2 receptor blockers are the main treatments for KS type I where coronary spasm is dominant. In addition to this therapy, PCI is usually required in KS type II/III to restore coronary flow [11].
In our patient, the generalized urticarial rash was the first manifestation of allergy after PCI. It was not associated with respiratory or haemodynamic compromise and improved with steroid and antihistamine therapy. Even though re-exposure to contrast during CT aortography was preceded by antihistamine and steroid administration, the patient developed severe chest pain with ST elevation myocardial infarction, and this raised the possibility of KS triggered by contrast. To avoid re-exposure to contrast, thrombolytic therapy was given with a good initial response. However, the recurrent chest pain associated with extensive ST elevation myocardial infarction necessitated PCI resulting in discovery of the stent thrombosis and successful treatment. The finding of stent thrombosis suggests KS type III. Unfortunately, follow-up echocardiography after 3 months revealed ischaemic dilated cardiomyopathy with a reduced EF of 25% so an ICD was inserted to protect against sudden cardiac death.
CONCLUSION
KS is an allergic acute coronary syndrome. Contrast-related KS is a rare entity which can lead to significant myocardial dysfunction due to recurrent myocardial infarction.