ABSTRACT
Objectives: We describe the novel case of a patient presenting with pulmonary mucosa-associated lymphoid tissue lymphoma (pMALToma) synchronous with metastatic prostate adenocarcinoma.
Materials and methods: We report the clinical, laboratory, radiological and histological findings of the above patient.
Results: While the patient’s metastatic prostate adenocarcinoma responded well to chemo-radio-hormonal therapy, a persistent area of lung consolidation was noted and further investigated, leading to the diagnosis of concurrent pMALToma.
Conclusion: It is important to pursue further investigation when there appears to be persistent change or altered disease response in malignancy if there is evidence for disease response elsewhere, as there may be two synchronous primary cancers.
LEARNING POINTS
- This is a novel case where pulmonary mucosa-associated lymphoid tissue lymphoma (pMALToma), a rare disease entity, presented synchronously and asymptomatically in a patient with metastatic prostate adenocarcinoma.
- From an instructive errors perspective, it is important to consider synchronous primary malignancy and pursue further investigations, as appropriate, when there appears to be persistent change or altered disease response if there is evidence for disease response elsewhere
KEYWORDS
pMALToma, prostate adenocarcinoma, synchronous primary malignancy, respiratory medicine, oncology
CASE DESCRIPTION
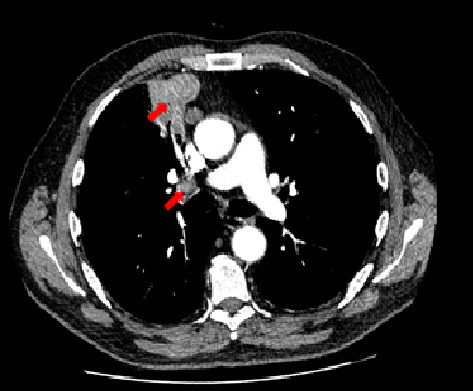
A 69-year-old male patient was referred to the respiratory clinic with a persistent cough, right hip pain and an abnormal chest x-ray (Fig. 1). The patient subsequently underwent computerised tomography (CT) of the thorax and abdomen with contrast which demonstrated airspace shadowing in the anterior segment of the right upper lobe with an air bronchogram and an enlarged right-sided anterior mediastinal lymph node measuring 17×12 mm adjacent to it (Fig. 2).
Following discussion in the lung cancer multi-disciplinary meeting, the patient underwent endobronchial ultrasound-transbronchial needle aspiration (EBUS-TBNA). Cellular pathology (cytopathology with rapid onsite evaluation and cell block preparation) confirmed metastatic prostatic adenocarcinoma (immunohistochemistry: AE1/AE3 strong, diffuse positive; PSA strong, focal positive; CK7 strong, focal positive (<5% of cells); CD10 strong, diffuse positive; CK20, CDX2, TTF-1, thyroglobulin and vimentin negative).
A subsequent positron emission tomography-computerised tomography (PET-CT) scan was reported as showing segmental collapse within the medial segment of the right upper lobe with moderately increased metabolic activity (SUVmax 3.8) with metabolically active lymph nodes in the left supra-ventricular fossa, central mediastinum, paracardiac fat, retroperitoneum and pelvis (SUVmax 5.9–10.1). There was a sclerotic focus within the right iliac bone (SUVmax 4.3) and asymmetrical uptake within the right side of the prostate gland (SUVmax 5.7) (Fig. 3).
Figure 1. Chest x-ray showing a bulky right hilum
Figure 2. Right mid-zone airspace shadowing and anterior mediastinal lymphadenopathy on computerised tomography
Figure 3. Positron emission tomography–computed tomography showing moderate activity in the right upper lobe with intense activity in a mediastinal lymph node
The patient’s prostate specific antigen (PSA) was measured and found to be elevated at 134.
He was reviewed in the uro-oncology outpatient clinic and commenced on bicalutamide 50 mg once daily, lifelong luteinizing hormone-releasing hormone agonist injections, docetaxel chemotherapy (six cycles completed) and palliative radiotherapy to the right hip (20 Gy in five fractions).
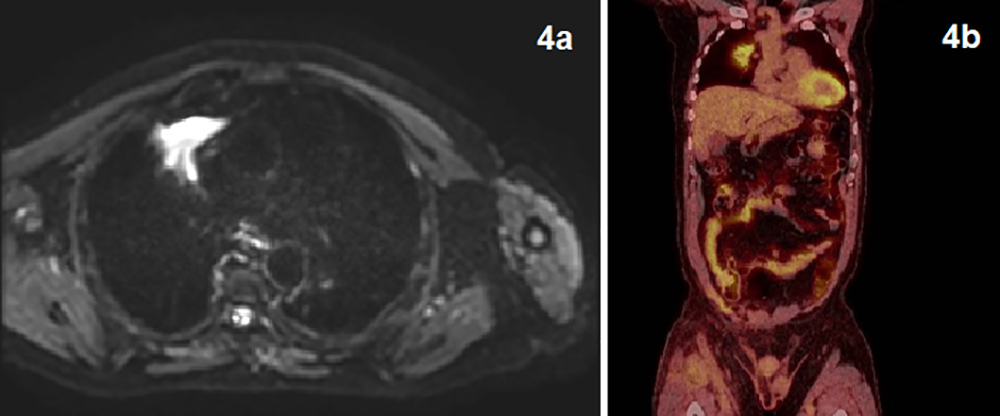
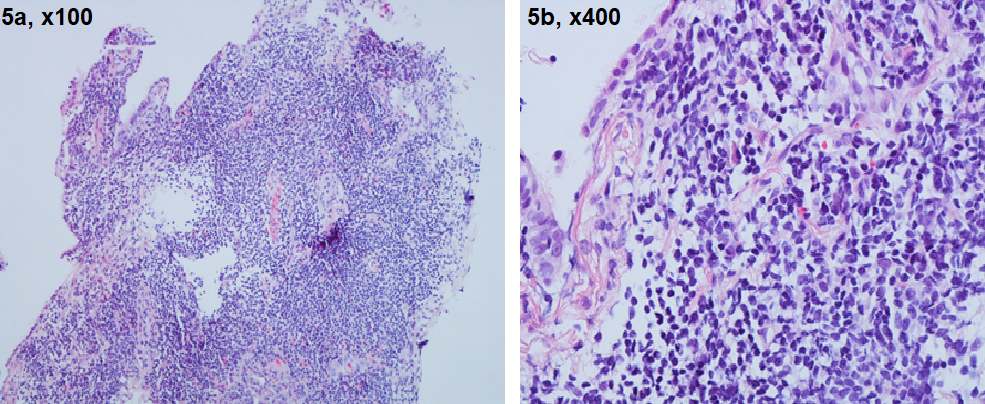
Biochemically, his disease responded well to treatment with normalisation of his PSA within 7 months of treatment (PSA 1.22). Completion-of-treatment whole body magnetic resonance imaging (MRI) showed persistent, cellular consolidation in the medial aspect of the right upper lobe but good disease response at other previously metabolically active sites (Fig. 4a). The patient was subsequently discussed again in the lung cancer multi-disciplinary meeting because of concern of a synchronous primary, and a repeat PET-CT was planned. This was reported as showing right upper lobe consolidation with diffuse low-grade activity throughout (Fig. 4b). Due to clinical stability, it was agreed to adopt a watch-and-wait approach with a repeat CT of the thorax planned for 6 months’ time. When this repeat CT demonstrated ongoing, persistent change, the patient underwent a bronchoscopy with radial EBUS with biopsies taken from the right upper lobe to determine causality. Rapid on-site evaluation (ROSE) was performed and showed a scanty aspirate of predominantly lymphocytes and reactive bronchial epithelial cells (Fig. 5a). Histopathology of the biopsy demonstrated a dense infiltrate of angular, irregular lymphoid cells, with immunohistochemical analysis showing positive CD20 immunostaining, indicating a B-cell infiltrate. As reactive infiltrates usually have a preponderance of T-lymphocytes, this widespread B-cell positivity was highly suggestive of lymphoma and, in the clinical context given the indolent presentation, pulmonary mucosa-associated lymphoid tissue lymphoma (pMALToma). Central review confirmed the diagnosis of pMALToma (Fig. 5b).
It was agreed at a subsequent haematology oncology multi-disciplinary meeting that given the relatively localised nature of the pMALToma and the fact that the patient was asymptomatic that management should be through a watch-and-wait approach.
Figure 4. (a) Magnetic resonance imaging showing persistent consolidation in the right upper lobe; (b) PET-CT showing static uptake in the right upper lobe
Figure 5 (a) Histology slide showing dense lymphoid infiltrate (magnification, ×100); (b) histology slide showing angular, irregular lymphoid cells with positive CD20 immunostaining (B-cell marker), suggestive of lymphoma (magnification, ×400)
DISCUSSION
Mucosa-associated lymphoid tissue (MALT) lymphomas, first described in 1983 by Isaacson and Wright, have since been recognized as a separate entity and account for 8–10% of all non-Hodgkin lymphomas [1]. pMALToma, also referred to as bronchial-associated lymphoid tissue lymphoma [2], is the most common form of primary pulmonary lymphoma but is a rare disease. The development of some pMALTomas has been reported to be associated with chronic inflammation due to autoimmune or infectious diseases [3]. pMALToma usually has an indolent course and remains localized in the lung for long periods prior to dissemination. The median age at diagnosis of pMALToma is 50–60 years [4]. Most patients are diagnosed with minimally invasive procedures such as radial EBUS [4]. The existing literature reports an indolent course of pMALToma, with an estimated 72% 10-year survival rate [5, 6]. The optimal therapy for this rare disease remains under debate, mainly due to the limited availability and heterogeneity of the data reported in the literature [7–9]. Various therapeutic regimens including radiotherapy, surgery and chemotherapy have been proposed, however following review of a case series of 11 patients, it has been suggested that a watch-and-wait policy may be adopted as the initial management of pMALToma in the absence of symptoms [10].
In the case described, further investigations were pursued because the cause of persistent right upper lobe lung consolidation was unexplained and concerning for a synchronous primary malignancy. In epidemiological studies, the frequency of multiple primaries is reported to be in the range of 2–17% [11].
PET-CT imaging has become firmly established as an excellent clinical tool in the diagnosis, staging and restaging of cancer [12]. However, we believe that its use should be clinically correlated to avoid misdiagnosis, overstaging of disease and unnecessary biopsies.
In conclusion, we present the unique case of a 69-year-old man with metastatic adenocarcinoma of the prostate synchronous with pMALToma. pMALToma is a rare disease and its progression is generally indolent. The educational interest of this case is that the pMALToma was diagnosed incidentally. The patient presented with symptoms caused by his metastatic prostate adenocarcinoma and the pMALToma was diagnosed in subsequent follow-up. The key learning point from this case is that it is important to consider synchronous primary malignancy and pursue further investigations, as appropriate, when there appears to be persistent change or altered disease response if there is evidence for disease response elsewhere.