ABSTRACT
Spontaneous, non-traumatic intra-cerebral haemorrhage is the second most common type of stroke and is associated with significant morbidity and mortality. It is defined as the presence of blood within the cerebral parenchyma without prior injury or surgery. The purpose of this work is to describe an atypical presentation of spontaneous intra-cerebral haemorrhage in a healthy young adult. A literature review was also carried out.
LEARNING POINTS
- Spontaneous intra-cerebral haemorrhage is a challenge in daily practice due to the wide range of clinical symptoms on presentation.
- Chest pain mimicking acute myocardial infarction is an atypical presentation of intra-cerebral haemorrhage.
- In the primary care setting, misdiagnosis of a patient with spontaneous cerebral haemorrhage with chest discomfort suggesting cardiac aetiology and prompting antiplatelet/aspirin therapy could result in disaster.
- Taking a detailed history and conducting a thorough neurological examination is important in every clinical encounter and may trigger diagnostic suspicion.
KEYWORDS
Acquired haemophilia, eosinophilic fasciitis
CASE DESCRIPTION
A 36-year-old previously healthy man was admitted to the Primary Health Care Centre in Kissamos, Crete complaining of a crushing retrosternal chest pain of 3 hours’ duration accompanied by a sensation of numbness in the left hand, sweating and nausea. The chest discomfort was described as a pressure sensation and was not relieved in intensity by movement or deep breathing. The patient was obese with a body mass index (BMI) of 34.6 kg/m2. He did not smoke or consume a lot of alcohol. He was not taking any medications.
The patient’s vital signs were: temperature 36.5°C, blood pressure (BP) 240/154 mmHg, pulse 86 per minute, and oxygen saturation 94% on ambient air. Heart sounds were normal with no murmurs. The clinical features of the chest pain suggested acute coronary syndrome.
The electrocardiogram (ECG) showed a sinus rhythm without pathological findings. Laboratory work-up did not show any elevation of cardiac enzymes, troponin I, T or creatine kinase MB iso-enzyme (CK-MB). Pulmonary auscultation and chest x-ray were also normal. The abdomen was soft on palpation, non-tender and non-distended with normal bowel sounds. Neurological examination disclosed a patient well oriented in space and time with meaningful speech. His pupils were round, regular and reacted promptly to light. Hypo-aesthesia was noted over the distribution of the first and second divisions of the trigeminal nerve. Barre sign was positive in the left upper and lower extremities. A mild decreased proximal muscle weakness bilaterally (4/5) in both upper and lower extremities was also found.
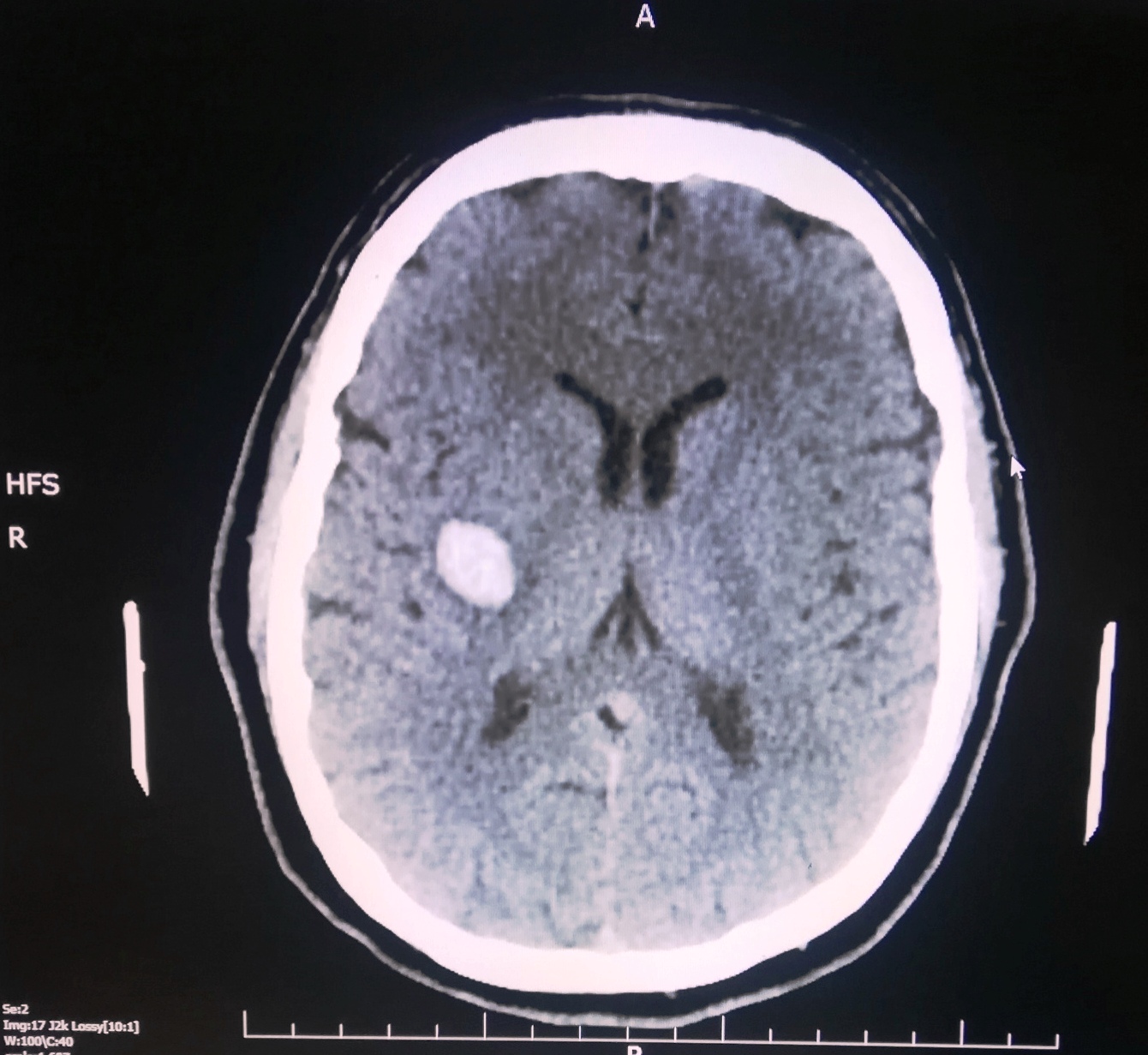
In view of these neurological deficits, the patient was referred to a secondary care centre for further evaluation. Computed tomography (CT)of the brain showed intra-parenchymal haemorrhage in the right parietal lobe (Fig. 1).
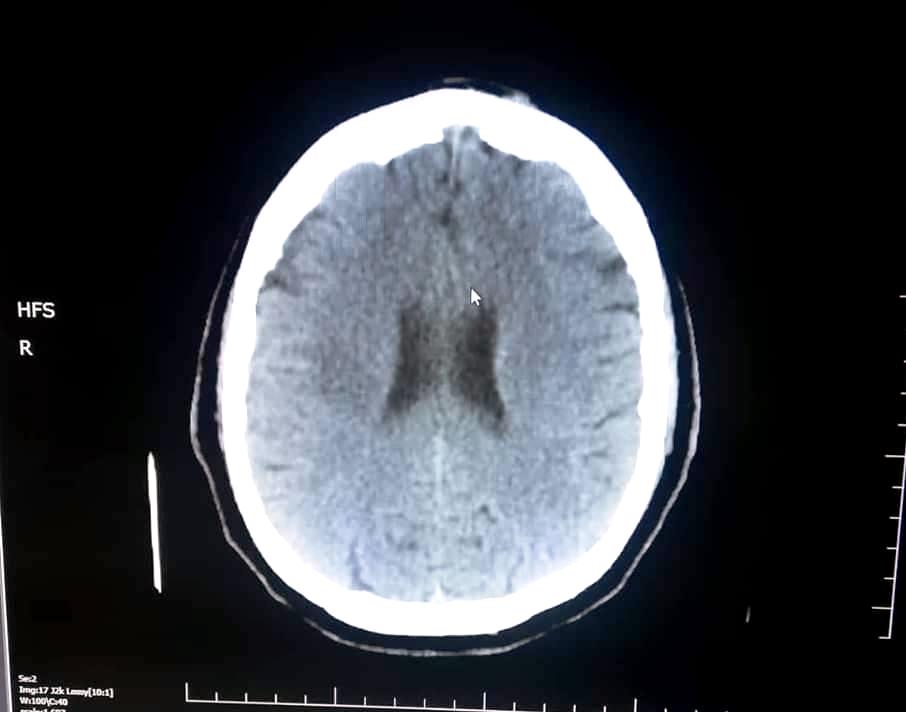
Anti-hypertensive treatment was initiatedwith amlodipine/perindopril once daily. The patient had an uneventful clinical course and was discharged home after 7 days. His BP normalized within 3 weeks. A follow up CT scan within a month showed complete resolution of the haemorrhage (Fig. 2).
Figure 1. Non-contrast CT scan of the brain showing a right parietal intraparenchymal haemorrhage
Figure 2. Follow-up non-contrast CT scan of the brain 4 weeks after hospital discharge
DISCUSSION
Intra-cerebral haemorrhage (ICH) is defined as the presence of blood within the brain and has the worst prognosis of the different stroke subtypes [1–3]. It is characterized by the rupture of small vessels within the brain parenchyma secondary to stress pressure on the vascular wall [4]. Various aetiological factors have been documented, with high arterial blood pressure being the most common [5]. Indeed, more than50% hypertensive individuals develop ICH [5]. Deep structures of the basal ganglia, thalamus, pons, midbrain and cerebellum are the most common sites of bleeding secondary to uncontrolled hypertension [4]. Cerebral amyloid angiopathy can also trigger ICH in elderly patients [4]. Vascular malformations, brain tumours and haemorrhagic conversion after ischaemic stokes can also cause ICH [4].
Risk factors that favour spontaneous haemorrhage within the brain are: hypertension, smoking, diabetes mellitus, antithrombotic therapy, heavy alcohol consumption, chronic renal failure, male gender, African-American ethnicity and malnutrition [4].
Clinical presentation is characterized by a wide range of symptoms. Patients may complain of headache, vomiting and/or focal neurological deficits [4]. Compression of the brain parenchyma secondary to haematoma expansion may result in loss of consciousness and the patient may be found in a coma by emergency personnel [4]. There are different neurological signs and symptoms depending on the site of haemorrhage[4]. Bleeding in the thalamus may cause confusion and hallucinations and bleeding in the cortexaphasia, while lobar haemorrhage is associated with an increased risk of early-onset seizures [4].
Taking a careful and detailed medical history from the patient is necessary for aetiological diagnosis [4]. Useful features include a history of previous stroke, uncontrolled hypertension and assessment of bleeding diathesis due to antiplatelet agents (aspirin and clopidogrel) [4]. Patients receiving the vitamin K antagonist, warfarin have an up to 10-fold increased risk of ICH [4].
Obtaining a finger-stick glucose measurement on admission is also needed in order to rule out hypoglycaemia. Initial laboratory work-up also requires a complete blood count, metabolic profile, renal and liver function tests, and measurement of troponin, prothrombin time, International Normalized Ratio (INR), and partial thromboplastin time [4]. Neuro-imaging with non-contrast computed tomography (CT) confirms the diagnosis [4].
Initial management consists of blood pressure as well as intracranial pressure control and surgery if required [4]. High blood pressure in a patient with ICH results in continuation of bleeding and haematoma expansion [4]. A systolic blood pressure of 140–160 mmHg has been suggested as a reasonable target. Secondary therapeutic goals include glycaemic and fever control. Approximately six out of 10 patients with ICH develop hyperglycaemia secondary to the elimination of stress hormones [4,5]. Hyperglycaemia has been associated with poor outcomes in terms of haematoma expansion and oedema [4]. Fever is also an adverse prognostic indicator and requires control with antipyretics [4].
The clinical presentation of this patient on admission was non-specific. To the best of our knowledge this is the first time that spontaneous ICH has manifested with retrosternal pain and numbness of an upper extremity. Furthermore, the ‘silent killer’ effect of high blood pressure is shown, highlighting the failure of primary prevention strategies for adequate detection and control.
Proper evaluation and triage of acute chest pain remains challenging. Acute chest pain generally suggests acute myocardial ischaemia, aortic dissection or pulmonary embolism [5]. In the acute or primary care setting, ECG and correct interpretation of ST-segment changes (ST-segment elevation or depression)and T-wave abnormalities (T-wave tenting or inversion) are crucial in order to initiate therapy withaspirin or another anti-platelet agent. In the absence of ECG abnormalities, patients with chest pain are a diagnostic conundrum. Biomarkers of myocardial injury include CK-MB isoenzyme, troponin T and I, and their measurement is recommended in intermediate and low risk cases. Troponin T or I generally is the most sensitive marker of acute coronary syndrome [5].
Prompt diagnosis and treatment may drastically reduce the burden of the disease. Furthermore, meticulous evaluation of chest pain is of particular value. In our patient, features of chest pain were suggestive of acute myocardial ischaemia. In the acute or primary care setting, inappropriate diagnosis and the administration of antiplatelet agents and aspirin would have had catastrophic effects for this patient.A careful neurological examination by the physicians involved is of paramount importance for an appropriate diagnosis.