ABSTRACT
An 81-year-old patient presented to the emergency department with a dark lesion on his forehead and swelling of his left eye, 3 days after a minor forehead injury and skin laceration. He also showed singular papules on his chin, upper chest, upper arms and back, later evolving into vesicles. Polymerase-chain reaction testing of vesicle content was positive for VZV and HSV-1, confirming a diagnosis of disseminated cutaneous herpes virus infection and concomitant HSV-1 reactivation. Antiviral and antibiotic treatment was initiated for 1 week with an immediate response. This case report highlights the association of head trauma and subsequent reactivation of VZV in patients at risk. Simultaneous reactivation of HSV-1 and VZV is rare in immunocompetent patients.
LEARNING POINTS
- Minor trauma can cause VZV and HSV reactivation.
- Consider herpes virus reactivation in case of unclear rash; the appearance of vesicles can be delayed for a few days.
- Screen for immunodeficiency disorders in disseminated herpes virus infection; if non-apparent, close monitoring is recommended.
KEYWORDS
Herpes simplex virus, varicella zoster virus, head trauma
INTRODUCTION
Herpes simplex virus (HSV-1 and 2) and varicella zoster virus (VZV) are closely related human alpha herpesviruses. Following the primary infection, both viruses remain dormant in the host in the dorsal root ganglia for years and can reactivate later in life. Dormancy of both viruses in the same nerve ganglion is possible [1]. The clinical manifestation of a primary VZV infection differs from VZV reactivation. While the primary infection leads to varicella or chickenpox, reactivation from latent VZV results in herpes zoster, also known as shingles. It is characterized by a painful, unilateral vesicular eruption that occurs in a restricted dermatomal distribution. Disseminated cutaneous herpes zoster is defined as the presence of more than 20 lesions outside the affected dermatome. It is rare and occurs mostly in immunocompromised patients with a decline in VZV-specific T-cell-mediated immunity [2].
CASE DESCRIPTION
An 81-year-old male patient with a history of well-controlled type 2 diabetes mellitus presented to the emergency room with a lesion on his left forehead, as well as periorbital swelling and erythema. Three days before presentation, he had injured his left forehead on a kitchen ventilator, resulting in a minor laceration. In the following days, he noticed a progressive rash and redness in the injured area, as well progressive left periorbital soft tissue swelling. Pain, itching, paraesthesia and vision impairment were absent.
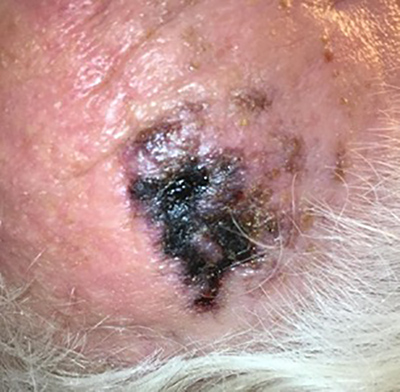
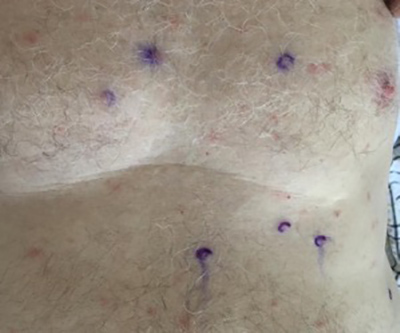
On physical examination, the patient’s vital signs including temperature were normal. Cardiopulmonary examination was without pathological findings. The skin on his left forehead showed a dark crusty erosion and there was pronounced periorbital redness and swelling on both sides (Figs. 1 and 2). There were singular papules on the chin and upper chest (Fig. 3), as well as multiple erythematous papules without vesicles on the back. The lesions were painless.
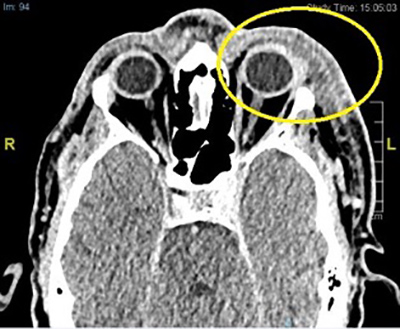
Trigeminal and facial palsies were absent. Blood tests showed an elevated C-reactive protein (36.1 mg/l, reference value <10.0 mg/l) with a normal white blood cell count with mild lymphopenia and monocytosis. Mild hyponatremia (129 mmol/l, reference value 135–145 mmol/l) and elevated creatinine (creatinine 115 µmol/l, reference value 49–97 µmol/l, corresponding to an estimated glomerular filtration rate of 51 ml/min/1.7) were present. A computed tomography scan of the head showed periorbital cellulitis on the left side without abscess formation (Fig. 4).
Figure 1. Left forehead with a crusty lesion on the day of admission
Figure 2. Progression of the disease with persistent crusty erosion and bilateral periorbital erythema and swelling on the day after admission
Figure 3. Disseminated singular papules on the trunk on the day after admission
Figure 4. Computed tomography scan demonstrating periorbital swelling, more pronounced on the left side
Our initial hypothesis was cellulitis resulting from the previous head injury and we started the patient on intravenous antibiotic treatment with amoxicillin/clavulanic acid 2.2 g three times a day. Due to the atypical presentation and extension of the skin lesions to the trunk, we suspected a possible viral aetiology and started concomitant treatment with intravenous acyclovir 500 mg three times a day. Within the next 24 hours the patient was febrile (38.3°C) and a vesicular rash had developed.
PCR testing of a swab of the vesicles on the forehead was positive for VZV (4,113,840,000 copies) and HSV-1 (396,500 copies). PCR testing of the vesicles on the trunk detected 312,000,000 copies of VZV and 600 copies of HSV-1. Serological studies were consistent with reactivation of the viruses (negative IgM, positive IgG antibodies for both VZV and HSV-1). Ophthalmological examination showed no evidence of herpes zoster ophthalmicus or acute retinal necrosis. We excluded underlying immunosuppressive diseases such as HIV infection and multiple myeloma. There were no clinical signs of reactivation of latent infections like cytomegalovirus or tuberculosis.
In summary, we established the diagnosis of disseminated VZV infection with concomitant reactivation of HSV-1, triggered by a minor head injury. The clinical picture was more consistent with VZV reactivation than HSV-1 reactivation, as there were no signs of herpes labialis or genitalis, and no herpetic whitlow. According to the guidelines [3], we increased the dose of acyclovir to 750 mg intravenously three times a day. Within 3 days, a favourable clinical course was observed with regression of the facial oedema and crusting of the vesicles.
After 7 days, we stopped therapy with both acyclovir and amoxicillin/clavulanic acid.
DISCUSSION
In the case described, the initial presentation of a localized rash after a minor head injury could have been mistaken for cellulitis or dermatitis. Taking a thorough history and performing a detailed clinical examination with a complete skin inspection was essential in order to not miss the evolving skin lesions on the trunk, which led to the diagnosis of disseminated herpes infection. In this situation, rapid and adequate treatment is crucial in order to prevent the serious complications of herpes zoster infection (herpes zoster ophthalmicus, acute retinal necrosis, Ramsay Hunt syndrome (herpes zoster oticus), aseptic meningitis, pneumonitis, bacterial superinfection) [4].
We believe that the head trauma, although minor in extent, caused reactivation of the herpes viruses. Trauma as a trigger for reactivation of VZV and HSV has been previously described in the literature. In an age-matched case-control study, herpes zoster was 3.4 times more likely to reactivate if the patient had experienced trauma in the week before onset compared to controls without VZV reactivation. In the case of cranial herpes zoster, it was even more than 25 times more likely that cranial trauma took place in the week before onset [5]. These findings support the theory that both immune-mediated factors and also local factors play a role in VZV reactivation. It remains unclear whether trauma also favours a disseminated course of the disease or only reactivation [6]. Moreover, the stress associated with the cranial trauma might have acted as an additive precipitating factor.
Disseminated herpes zoster occurs typically in immunocompromised patients. In our case, two important risk factors were present: age and diabetes mellitus. Advanced age with a relative decline in immune function is an important risk factor for reactivation of VZV [4].
In order to prevent VZV reactivation, vaccination with a recombinant glycoprotein E vaccine is recommended in patients older than 50 years to boost the VZV-specific T-cell immune response [7].
Simultaneous reactivation of HSV and VZV is rarely described, which may be because testing for both viruses is not routinely carried out. In the largest series to date, 1718 patients with suspicious skin lesions were evaluated for both viruses by PCR, and VZV and HSV were simultaneously detected at the same body site in only 1.2% of patients, most of whom had a clinical diagnosis of herpes zoster [8]. Interestingly, the trigeminal region was affected most commonly similarly to our case, and none of the patients had any signs of immunosuppression. Thus, it seems that simultaneous reactivation of VZV and HSV is rare. As the dosage and treatment duration may differ, testing for both viruses by PCR may be recommended in indeterminate cases.
CONCLUSION
A minor head injury can trigger VZV reactivation and even its disseminated form in elderly immunocompetent patients. The clinical presentation can be misleading (e.g., cellulitis or dermatitis), and so a high index of clinical suspicion is needed to establish the correct diagnosis. Simultaneous reactivation of HSV-1 is rare.