ABSTRACT
Thyroid storm is a rare, life-threatening condition that can be caused by various pathologies including serious conditions associated with human chorionic gonadotropin (hCG)-producing tumours.
We present the case of a 17-year-old male patient with a 1-month history of dyspnoea and a 3-day history of palpitations and fever. General examination revealed a left testicular mass. Blood tests revealed β-hCG >225,000 mIU/ml, thyroid-stimulating hormone (TSH) 0.02 IU/ml, and thyroxine (T4) 19.07 µg/dl. He was admitted with thyroid storm. Treatment with antithyroid drugs and chemotherapy was started, but the patient died on the third day of admission.
This case highlights a rare occurrence of thyroid storm linked to testicular choriocarcinoma, and provides a necessary reminder that, in some instances, hCG at very high levels can exert a thyrotropic effect due to its molecular structure, which is similar to that of TSH.
LEARNING POINTS
- Thyroid storm is rarely associated with testicular choriocarcinoma.
- Sometimes, human chorionic gonadotropin at very high levels can exert a thyrotropic effect due to its molecular structure, which is similar to that of thyroid-stimulating hormone.
- The clinical course and management of thyroid storm secondary to testicular choriocarcinoma in a young male is described.
KEYWORDS
Thyroid storm, testicular choriocarcinoma, human chorionic gonadotropin
CASE DESCRIPTION
A 17-year-old Latin male patient with testicular choriocarcinoma underwent left radical orchiectomy with difficult extraction and a normal spermatic cord. Two months after surgery, the patient attended the emergency service with a 1-month history of dyspnoea, productive cough and haemoptysis and a 3-day history of palpitations and fever. The physical examination showed a blood pressure of 108/60 mmHg, heart rate of 160 beats/min, respiratory rate of 28/min, body temperature of 37.8° C (100°F) and peripheral oxygen saturation (SpO2) of 94%. There were no signs of goitre or thyroid eye disease. Clinical examination revealed lymphadenopathies in the cervical, supraclavicular and axillar (bilateral) regions. Gynecomastia was present. Auscultation revealed bibasal crepitation and non-sustained ventricular tachycardia. A 4 cm tumour was found in the left region of the scrotum, and was firm, non-indurated and painless to the touch. The extremities presented fine trembling.
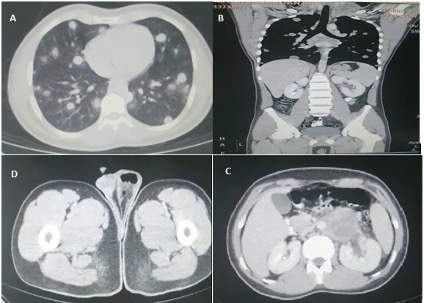
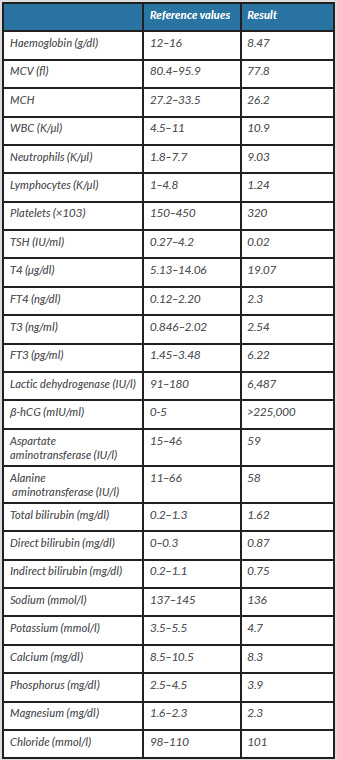
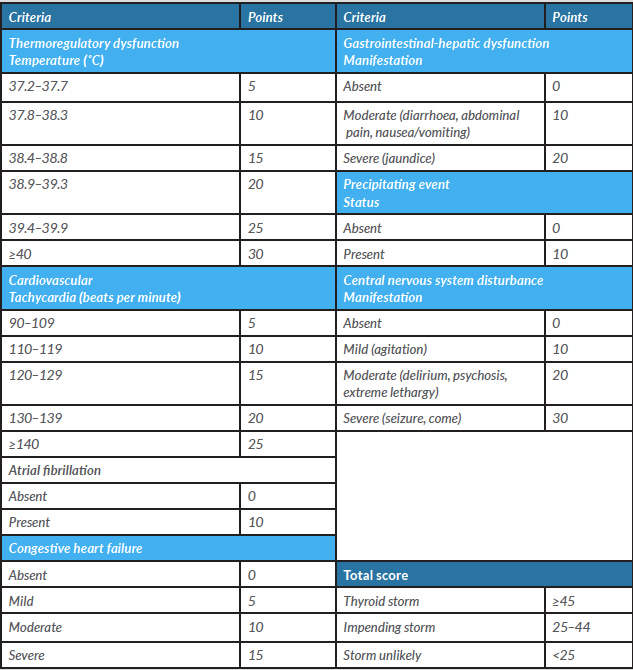
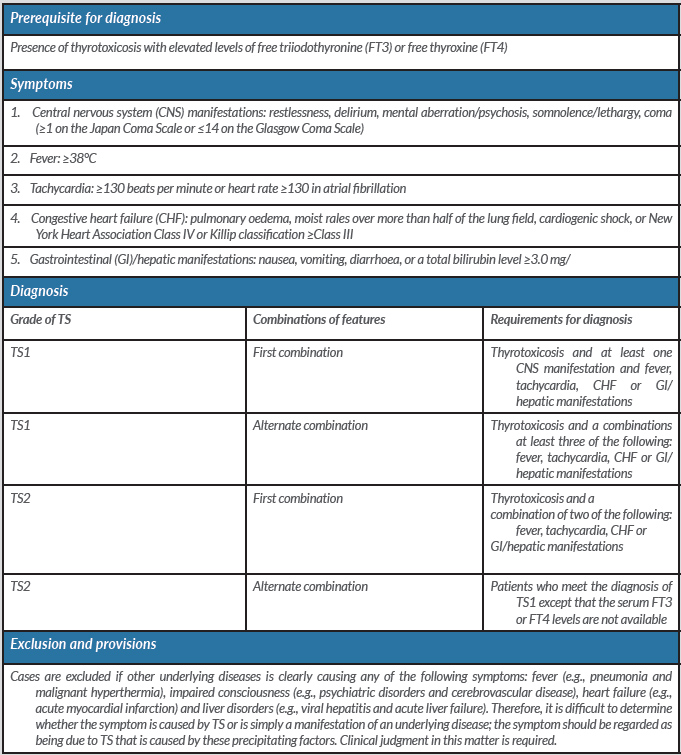
The patient was admitted to the intensive care unit. Initial laboratory investigation showed microcytic anaemia (haemoglobin 8.47 g/dl), normal D-dimer (<0.5 µg/ml), and elevated lactic dehydrogenase (6,487 IU/l) and β-hCG (>225,000 mIU/ml). Thyroid function tests revealed a raised serum thyroxine (T4) level (19.07 µg/dl) and reduced thyroid-stimulating hormone (TSH) concentrations (0.02 IU/ml). Laboratory test results are summarized in Table 1. A computed tomography (CT) scan of the chest demonstrated multiple bilateral pulmonary nodules, while a CT scan of the abdomen showed conglomerate retroperitoneal adenopathies (Fig. 1). The ECG only showed sinus tachycardia without further alterations. These symptoms suggested a diagnosis of thyroid storm, accumulating 65 points on the Burch-Wartofsky scale (Table 2) and meeting the requirements of grade 1 on the Japan Thyroid Association scale (Table 3).
Figure 1. CT scan of the chest, abdomen and pelvis. (A,B) Axial and coronal images of the chest show multiple bilateral pulmonary nodules. (C) Axial image of the abdomen shows conglomerate retroperitoneal adenopathies and a preserved liver. (D) CT scan of the pelvic area shows a scrotal mass in the left region.
Table 1. Laboratory test results
Table 2. The Burch-Wartofsky Point Scale for the diagnosis of thyroid storm
Modified from Burch HB, Wartofsky L. Life-threatening thyrotoxicosis: thyroid storm. Endocrinol Metab Clin North Am 1993;22:263–277.
Table 3. The Japan Thyroid Association diagnostic criteria for thyroid storm (TS)
TS1, ‘Definite’ TS; TS2, ‘Suspected’ TS.
Modified from Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, et al. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 2012;22(7):661–679.
The patient’s thyrotoxicosis was considered to be a paraneoplastic phenomenon. He was treated with propranolol 40 mg every 8 hours, methimazole 5 mg every 8 hours and hydrocortisone 100 mg every 8 hours. He was assessed by a consultant urologist and referred urgently to an oncologist. On the following day, he started emergency chemotherapy with bleomycin and etoposide. He was treated with intravenous fluids and alopurinol to reduce the impact of tumour lysis syndrome during chemotherapy. Thromboprophylaxis was contraindicated due to a high risk of spontaneous intrapulmonary haemorrhage. His condition deteriorated 2 days later and he developed respiratory failure, accompanied by increased haemoptysis, which affected his haemodynamic state.
He was transferred to the intensive care unit and required intubation and ventilation. CT pulmonary angiography excluded pulmonary embolism. His condition deteriorated steadily despite intensive support and he died 1 day later of respiratory failure.
DISCUSSION
Testicular cancer accounts for approximately 1% of malignant tumours in men [1]. Testicular tumours can produce hCG, with choriocarcinoma tumours most frequently associated with high hCG secretion [1]. There are many causes of thyrotoxicosis, including serious conditions such as toxic adenoma, trophoblastic disease, pituitary adenoma, struma ovarii, iatrogenic thyrotoxicosis, follicular thyroid cancer metastasis and hCG-producing tumours. An estimated 1–2% of thyrotoxicosis patients meet the criteria for thyroid storm, which has a high mortality rate of 20–30% [2].
TSH, follicle stimulating hormone, luteinizing hormone and hCG form a family of heterodimeric glycoprotein hormones which share a common alpha subunit but have different functional beta subunits and a similar mechanism of action of binding to specific receptors, which suggests the basis of the reactivity of hCG with the TSH receptor. One of the roles of the carboxy-terminal peptide or β-CTP may be to prevent overt hyperthyroidism in the first trimester of pregnancy when a large amount of hCG is produced by the placenta [3]. hCG concentrations can stimulate the thyroid, as also shown in pregnancy, where high concentrations of hCG during early pregnancy result in an increase in free thyroxine (FT4) concentrations which subsequently lead to a decrease in TSH concentrations. Intact hCG (hCGi) is the predominant form in pregnancy. Nicked and hyperglycosylated variants are the predominant forms in choriocarcinomas. There are differences in the thyrotropic activity of the different hCG molecules. Nicked hCG preparations, obtained from patients with trophoblastic disease or by enzymatic digestion of hCGi, showed approximately 1.5 to 2-fold greater stimulation of recombinant hTSH receptor compared with hCGi [3]. This suggests that the thyrotropic activity of hCG may be influenced by the metabolism of the hCG molecule itself.
In general, symptoms of hyperthyroidism should be treated with antithyroid agents until the source of β-hCG secretion can be surgically removed or until chemotherapy can be initiated. In our patient, the antithyroid agents used were methimazole (MMI), propranolol and hydrocortisone. However, we prefer to treat patients with propylthiouracil (PTU) instead of the MMI recommended by the American Thyroid Association [4] because at a dose of at least 400 mg/day it is a more potent inhibitor than MMI of type I deiodinase, which limits the conversion of T4 to triiodothyronine (T3), both in the thyroid gland and in peripheral organs [4]. In our case, MMI was chosen because PTU is not available in our country. A long-term study in Japan on compensated Graves’ patients, revealed that MMI normalized thyroid hormone levels more rapidly than PTU, and also showed that the incidence of adverse effects in patients treated with MMI was significantly lower than in those treated with PTU [5]. These observations suggest that MMI may actually be better than PTU for the treatment of thyrotoxicosis in thyroid storm.
The possibility of hyperthyroidism or thyroid storm should be considered in the initial differential diagnosis of a young man presenting with fever, tachycardia, tremors and hypokalaemia thyrotoxic paralysis.