ABSTRACT
Diffuse dermal angiomatosis is a benign vascular disorder suspected in patients with cardiovascular risk factors. We report the case of a 62-year-old woman with a non-healing hip wound but no significant cardiovascular risk factors, who was found to have diffuse dermal angiomatosis on biopsy leading to the diagnosis of severe peripheral vascular disease. Her wound healed after revascularization.
LEARNING POINTS
- Patients with diagnosed diffuse dermal angiomatosis should be evaluated for underlying peripheral vascular disease.
- The mainstays of therapy are treating the underlying cause, lifestyle modifications to control the risk factors, and revascularization.
- Diffuse dermal angiomatosis is diagnosed on biopsy and can present in patients without any significant risk factors.
KEYWORDS
Diffuse dermal angiomatosis, peripheral vascular disease, revascularization
INTRODUCTION
Diffuse dermal angiomatosis (DDA) is a type of reactive skin angioproliferation, characterized by red-violet purpuric papules or plaques leading to necrosis. The diagnosis is suspected in patients with cardiovascular risk factors. DDA presenting in an asymptomatic patient is novel. Here, we report the case of a 62-year-old woman without any significant underlying cardiovascular risk factors, who presented with a non-healing wound after a fall and was found to have DDA on biopsy, leading to the diagnosis of severe peripheral vascular disease (PVD).
CASE DESCRIPTION
A 62-year-old woman with well-controlled essential hypertension presented to the emergency department complaining of a chronic non-healing left hip wound that had developed 1 month after a fall. The wound had progressed from a pulsating mass to a black necrotic eschar on her left lateral thigh (Fig. 1). The pain did not respond to over-the-counter medications. The patient denied any fever, chills, decreased sensation, decrease in range of motion, joint pains or stiffness, joint rash, proximal muscle weakness, leg swelling, or any other associated symptoms. The patient denied any history of smoking or intravenous drug use. Her previous work-up at another hospital had been unrevealing. She had been treated with two courses of broad-spectrum antibiotics before presentation at our hospital.
The patient was on room air and afebrile, with a heart rate of 110 beats per minute and a blood pressure of 148/53 mmHg. On examination, a large, thick necrotic eschar (9×10 cm) surrounded by a border of erythema, was noted over the thigh, which was tender to touch, with femoral pulses intact bilaterally. The rest of the physical examination was unremarkable.
Her laboratory work-up revealed a white blood cell count of 10,300/μl, platelet count of 419,000/μl, ESR of 102 mm/hour, and C-reactive protein of 11.3 mg/dl. An x-ray of the pelvis showed sclerosis projecting over the left femoral head. Ultrasound demonstrated a hypoechoic subcutaneous lesion. Magnetic resonance imaging of the left hip revealed mild effusion with surrounding skin oedema. A vasculitic panel and hypercoagulable panel were sent on admission and returned negative.
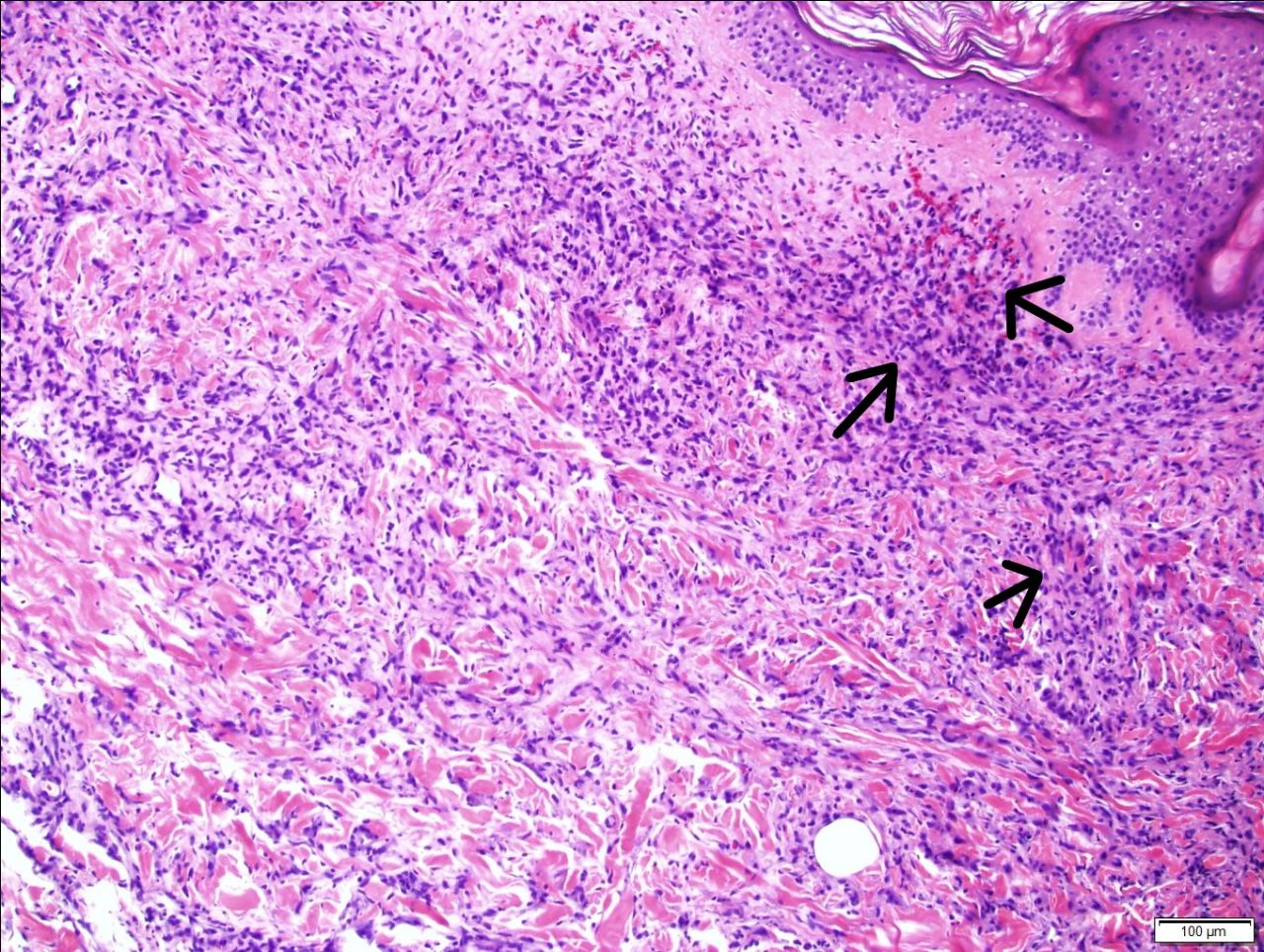
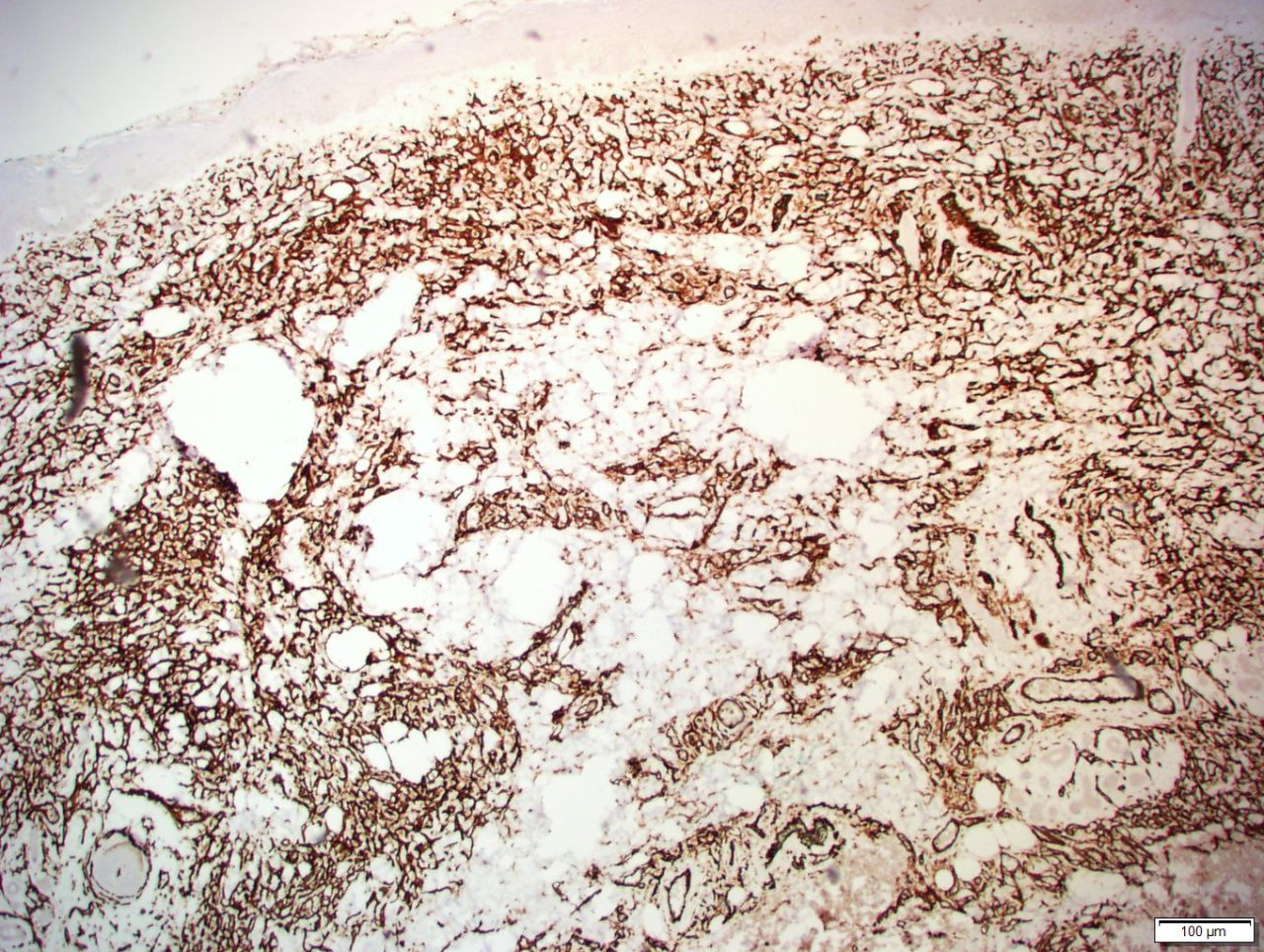
Dermatology was consulted and biopsies of the surrounding wound showed DDA (Figs. 2 and 3). Vascular surgery was consulted and the arterial brachial index (ABI) was obtained, revealing severe PVD. CT angiography with run-off demonstrated severe aortoiliac artherosclerosis with 75% of distal aorta and approximately 75% stenosis of the common iliac arteries with near-complete occlusion of distal left artery iliac artery (Fig. 4).
The patient underwent endovascular aneurysm repair with bilateral common femoral and bilateral common and left external iliac stenting. She was started on dual antiplatelet therapy and received extensive wound care.
Figure 2. H&E staining showing diffuse interstitial infiltrate of endothelial cells extending throughout the papillary and reticular dermis
Figure 3. CD34 staining showing diffuse endothelial cells
Figure 4. 3D reconstruction showing extensive aortoiliac atherosclerosis bilaterally
Her hospital course was further complicated with opioid dependence, opioid-induced constipation and hypovolemic hyponatremia. During her stay, the patient’s wound healed, resulting in yellowish crusting and induration over her left hip. She was discharged to a nursing facility after 10 days of hospitalization with close follow-up by vascular surgery and her primary care physician.
DISCUSSION
DDA is a benign vascular disorder of the skin associated with underlying atherosclerotic PVD. The pathogenesis is possibly related to the release of proangiogenic factors for restoration of diminished blood flow [1]. The disease affects people 40–60 years of age, commonly females with risk factors, and occurs at locations such as the breasts, lower calves and abdomen. Colmenero et al.[2] mentioned that dermal manifestations included erythematous, poorly demarcated plaques that ultimately undergo necrosis.
Tanya et al. suggested in a case report that the diagnosis should be suspected in patients with cardiovascular risk factors such as calciphylaxis, monoclonal gammopathy and antiphospholipid syndrome. Notably, the same report also suggests smoking, obesity and PVD as risk factors[3]. The management of DDA depends on the underlying vascular status and revascularization is usually the mainstay of treatment. Yang et al. reported complete resolution of skin lesions after revascularization [4]. In two other reports, isotretinoin and corticosteroids were also effective because of their anti-angiogenesis properties [5].
Touloei et al. in 2019 summarized the findings of all published case reports on DDA [6]. Out of 73 patients, 71.2% were female with a mean age of 49.5 years, 52% had a lesion on the breast and 7.5% on the thigh, as in our case. Smoking (57.5%) was the most common risk factor, followed by obesity (32.9%), vascular disease (23.3%) and hypertension (2.5%). Treating the underlying cause, revascularization and isotretinoin were effective in treating breast DDA. In some cases, steroids were beneficial.
Our case was unique as DDA mimicked a post-traumatic wound in a patient with no significant cardiovascular risk factors, and DDA led to a diagnosis of severe PVD.
CONCLUSION
Patients with diagnosed DDA should be evaluated for underlying PVD. Management is based on strict control of underlying comorbidities and revascularization, and in some cases, isotretinoin and steroids can be beneficial