ABSTRACT
The authors present the case of a 51-year-old woman with no history of surgical or traumatic injury or accident, who presented with right hypochondrium and epigastric discomfort, malaise, nausea, loss of appetite and episodes of dark urine and greenish stools. Initial laboratory work-up revealed elevated inflammatory markers including leucocytosis with left shift and C-reactive protein, and a slight elevation of gamma-glutamyltransferase and alkaline phosphatase, with no other significant alterations. Computed tomography (CT) showed intrathoracic acute cholecystitis with a large diaphragmatic hernia.
A literature search revealed only one other case of acute cholecystitis complicated by intrathoracic gallbladder due to a non-traumatic diaphragmatic hernia. Symptoms are uncharacteristic and the absence of pain or fever, explained by the altered location of the gallbladder, makes the diagnosis a challenge.
LEARNING POINTS
- Only one other case of acute cholecystitis complicated by intrathoracic gallbladder due to a non-traumatic diaphragmatic hernia has been reported.
- Uncharacteristic symptoms make the diagnosis of intrathoracic acute cholecystitis a challenge.
KEYWORDS
Intrathoracic acute cholecystitis, diaphragmatic hernia, non-traumatic
INTRODUCTION
The authors present a case and the route taken to diagnose intrathoracic acute cholecystitis and a congenital right diaphragmatic hernia.
CASE DESCRIPTION
A 51-year-old woman presented with right hypochondrium and epigastric discomfort, malaise, nausea and loss of appetite associated with episodes of dark urine and greenish stools. The patient had no diarrhoea, constipation or vomiting. Although she denied having a fever, she had felt feverish the previous couple of days.
Her past medical history was significant for hypertension and hyperthyroidism, treated with losartan and thiamazole. She also had chronic gastritis, having recently been diagnosed with Helicobacter pylori infection and had begun treatment with bismuth subcitrate potassium, metronidazole and tetracycline 2 days before presenting to hospital. The patient also reported having a diaphragmatic hernia but had had no further work-up. She had no past surgical history, allergies or any past traumatic injury or accident.
Physical examination was notable for slight tenderness in the epigastric and right hypochondrium regions, with no rebound or guarding. Although normotensive and not febrile, the patient was slightly tachycardic (heart rate 103 bpm). She also presented with diminished respiratory sounds on the right pulmonary base, but had no signs of respiratory distress and showed good peripheral perfusion. Cardiac auscultation was unremarkable.
Initial laboratory work-up revealed elevated inflammatory markers including leucocytosis with left shift and C-reactive protein of 12.1 mg/dl (normal range 0.05–1.00 mg/dl). There was also a slight elevation of gamma-glutamyltransferase and alkaline phosphatase, with no other significant alterations in bilirubin, amylase or transaminase enzymes.
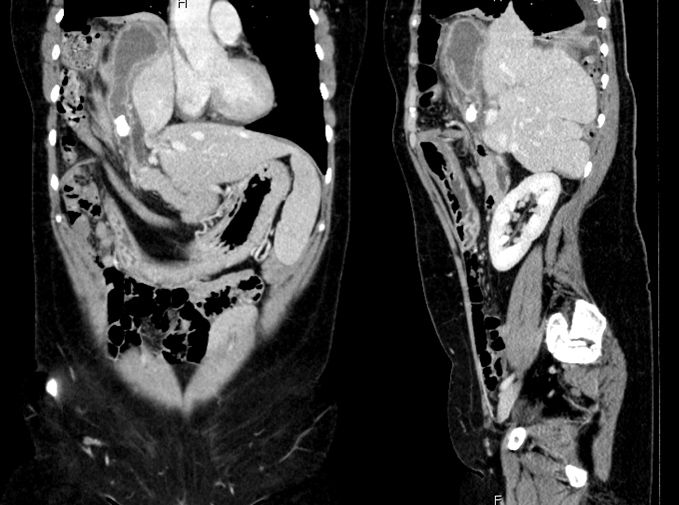
Due to these findings, the patient underwent computed tomography (Fig. 1) which showed a large right-sided diaphragmatic hernia, with intrathoracic herniation of the right hepatic lobe, gallbladder and a segment of the right colon. Furthermore, the gallbladder was distended, and had thickened walls with a large gallstone (18 mm) in the infundibular region. Another gallstone (5 mm) could be identified in the common bile duct. In view of these results, the diagnosis of intrathoracic acute cholecystitis with a large diaphragmatic hernia was made. The patient was hospitalized for monitoring and treatment. A non-surgical approach was the treatment of choice with piperacillin-tazobactam.
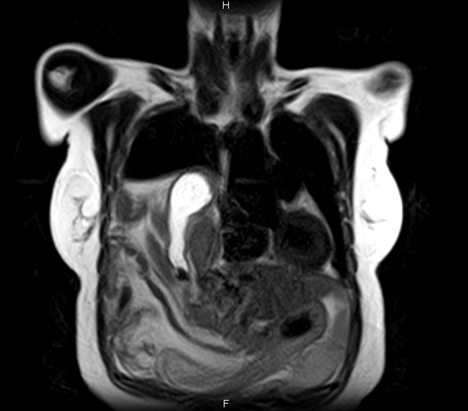
During her hospitalization, the patient underwent magnetic resonance cholangiopancreatography (cholangio-MRI) for a better understanding of the origin of the hernia and the anatomy of the liver and bile ducts (Fig. 2). This showed interruption of the diaphragm in the posterolateral region, and a completely intrathoracic right hepatic lobe and gallbladder. Part of the right and transverse colon were also intrathoracic. These findings were compatible with a congenital diaphragmatic hernia.
There were no complications during hospitalization and the patient was discharged home with oral antibiotics on the 5th day. Subsequent surgical removal of the gallbladder is being planned.
Figure 1. Computed tomography showing a large right-sided diaphragmatic hernia, with intrathoracic herniation of the right hepatic lobe and gallbladder which is distended, with thickened walls and a large gallstone (18 mm) in the infundibular region. Another gallstone (5 mm) can be identified in the common bile duct
Figure 2. Cholangio-MRI showing the interruption of the diaphragm in the posterolateral region, and a completely intrathoracic right hepatic lobe and gallbladder
DISCUSSION
Our principal aim is to highlight the subtlety of the clinical presentation. The absence of pain explained by the altered location of the gallbladder, made the diagnosis harder.
The second goal is to draw attention to the rarity of the case. According to a literature search, only one other case of acute cholecystitis complicated by intrathoracic gallbladder due to a non-traumatic diaphragmatic hernia has been reported. In that case, the patient underwent open cholecystectomy and delayed diaphragmatic hernia repair, with a favourable outcome [1].
Diaphragmatic hernias usually occur secondary to rupture of the diaphragm in the setting of trauma but may be overlooked in the acute phase. The injury is later diagnosed and corrected when it becomes clinically evident, usually due to complications of the contents of the hernia. However, the symptoms are uncharacteristic, making the diagnosis a challenge [2]. On the other hand, congenital diaphragmatic hernias are usually identified prenatally with ultrasound examination.
In our case, the patient had no history of trauma or abdominal or thoracic surgery. She had been asymptomatic until this episode, when the presence of gallstones in an inflamed gallbladder led to the diagnosis of intrathoracic cholecystitis and a diaphragmatic hernia. The patient’s history and the results of the MRI suggested the diaphragmatic hernia was congenital. A non-surgical approach was the treatment of choice in this case, in the acute setting of the cholecystitis, but the subsequent surgical removal of the gallbladder is being planned.