ABSTRACT
The authors present a case of phantom tumour of the lung. This is a type of pleural effusion where fluids accumulate in the interlobar fissures, typically in the transverse fissure. Its prompt recognition avoids additional, unnecessary or expensive examination and treatment mistakes.
LEARNING POINTS
- Phantom tumour of the lung should be considered as a differential diagnosis for a radiographic opacity because it can be misdiagnosed as a lung mass or consolidation.
- Its rapid disappearance after management of the underlying condition, in this case of cardiac decompensation with diuretics, confirms the diagnosis.
- Prompt recognition avoids additional, unnecessary or expensive examination and treatment mistakes.
KEYWORDS
Pleural effusion, phantom tumour
CASE DESCRIPTION
An 85-year-old male patient presented to our emergency department with a 3-day history of dyspnoea on effort, productive cough and fever. He had a history of coronary disease, arterial hypertension, atrial fibrillation (he had a pacemaker), stage 3 chronic kidney disease and a history of smoking. He was chronically treated with carvedilol, amiodarone, rivaroxaban, perindopril and indapamide.
Physical examination did not show jugular venous distension or peripheral oedema, but auscultation of the lungs revealed bibasilar crackles. The patient was eupnoeic and afebrile.
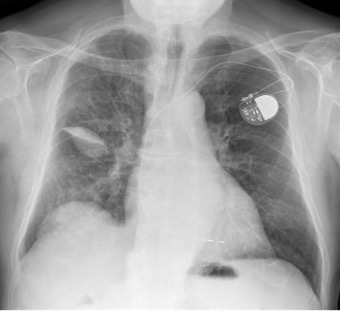
Arterial blood gas analysis revealed mild hypoxemia (pO2 55 mmHg). Laboratory test results showed relative neutrophilia and an elevated C-reactive protein of 11.4 mg/dl (normal range <0.50), elevated serum brain natriuretic peptide of 212.0 pg/ml (normal range <100.0), and basal creatinine of 1.6 mg/dl (normal range 0.6–1.3). A postero-anterior chest radiograph revealed an oval-shaped opacity measuring 6 cm at its greatest diameter, well-delineated, in the right middle lung field (Fig. 1). ECG showed sinus rhythm.
The patient was admitted with a presumptive diagnosis of pneumonia and was started on antibiotics.
After admission, the image was reinterpreted as phantom tumour of the lung because of high clinical suspicion of associated congestive heart failure. Intravenous furosemide 60 mg/day was initiated. One day later, chest radiography showed only a small drop-shaped opacity, well-delineated in the topography of right transverse fissure (Fig. 2).
Transthoracic echocardiography demonstrated hypertrophy of the interventricular septum, a systolic ejection fraction of 61% and grade 2 diastolic dysfunction.
The patient’s signs and symptoms resolved, and radiological follow-up showed progressive disappearance of opacity. He was discharged after 5 days maintaining furosemide 40 mg/day. A chest radiograph 3 weeks later was normal (Fig. 3).
Figure 1. Postero-anterior chest radiograph at the patient’s hospital admission reveals right round-shaped opacity measuring 6 cm at its greatest diameter
Figure 2. Postero-anterior chest radiograph 1 day after diuretic therapy
Figure 3. Postero-anterior chest radiograph, 3 weeks after admission, shows complete resolution of opacity
DISCUSSION
Phantom or vanishing tumour of the lung is a rare finding on chest radiographs [1, 2]. It is a type of pleural effusion where fluids accumulate in the interlobar fissures, typically in the transverse fissure, as we report in our case, but can also occur less commonly in the oblique fissure [1–4].
The pathophysiology is explained by adhesions and obliteration of the pleural space around the edge of the fissure due to pleuritis; fluid loculation occurs when the resorptive capacity of the pleural lymphatic system is exceeded. Another explanation is a local increase in elastic recoil caused by atelectasis of the lung [5].
Phantom or vanishing lung tumour was first described by Stewart in 1928, associated with heart failure. Other aetiologies less frequently reported include renal failure or hepatic failure [1]. We describe a patient who presented with acute decompensated heart failure with preserved systolic function and chronic renal disease.
Recognition of a phantom tumour on chest radiograph is very important because it is easily misdiagnosed as pulmonary infiltrate, as occurred in this case. It tends to recur with cardiac decompensation, so this should be remembered when a mass appears on chest radiograph. Accurate diagnosis avoids unnecessary computed tomography and overuse of antibiotics.
Radiological improvement can be observed less than 1 day after the introduction of diuretic treatment. Our patient responded promptly to diuretic therapy, which confirms the diagnosis as there are no specific diagnostic procedures. Sometimes, patients with renal chronic disease have a poor response to diuretics and dialysis is instituted in such cases [1].