ABSTRACT
Haemoptysis is a frequently occurring but sometimes life-threatening condition. Congenital cardiovascular abnormalities are rare causes of haemoptysis. We report a case of a 33-year-old man without any past medical history complaining of haemoptysis with no other associated clinical manifestations. A contrast-enhanced chest computed tomography scan revealed aortic coarctation with dilation of the internal mammary, intercostal and bronchial arteries. He underwent stent placement after balloon angioplasty with favourable outcomes.
LEARNING POINTS
- Adult patients with congenital cardiovascular abnormalities such as aortic coarctation may rarely, due to the high pressure and dilation in the bronchial arteries, present with recurrent haemoptysis as the sole clinical sign.
- A multidetector computed tomography scan contributes significantly to the aetiological diagnosis of haemoptysis in cases of congenital cardiovascular abnormalities.
- Interventional procedures such as stenting are currently the preferred approach for the treatment of aortic coarctation in adults, with good outcomes.
KEYWORDS
Haemoptysis, cardiovascular abnormalities, aortic coarctation, CT scan, stent
INTRODUCTION
Haemoptysis is a frequent clinical presentation with different underlying conditions. It can be life-threatening with a fatal issue. Urgent treatment of the haemoptysis and the cause is essential [1]. Congenital cardiovascular anomalies represent an uncommon aetiology group causing haemoptysis [1]. In fact, some congenital anomalies can affect the bronchial and pulmonary vasculature [1]. We herein present a case of a 33-year-old man with an unknown aortic coarctation revealed by haemoptysis as the sole sign, due to systemic collateralization.
CASE PRESENTATION
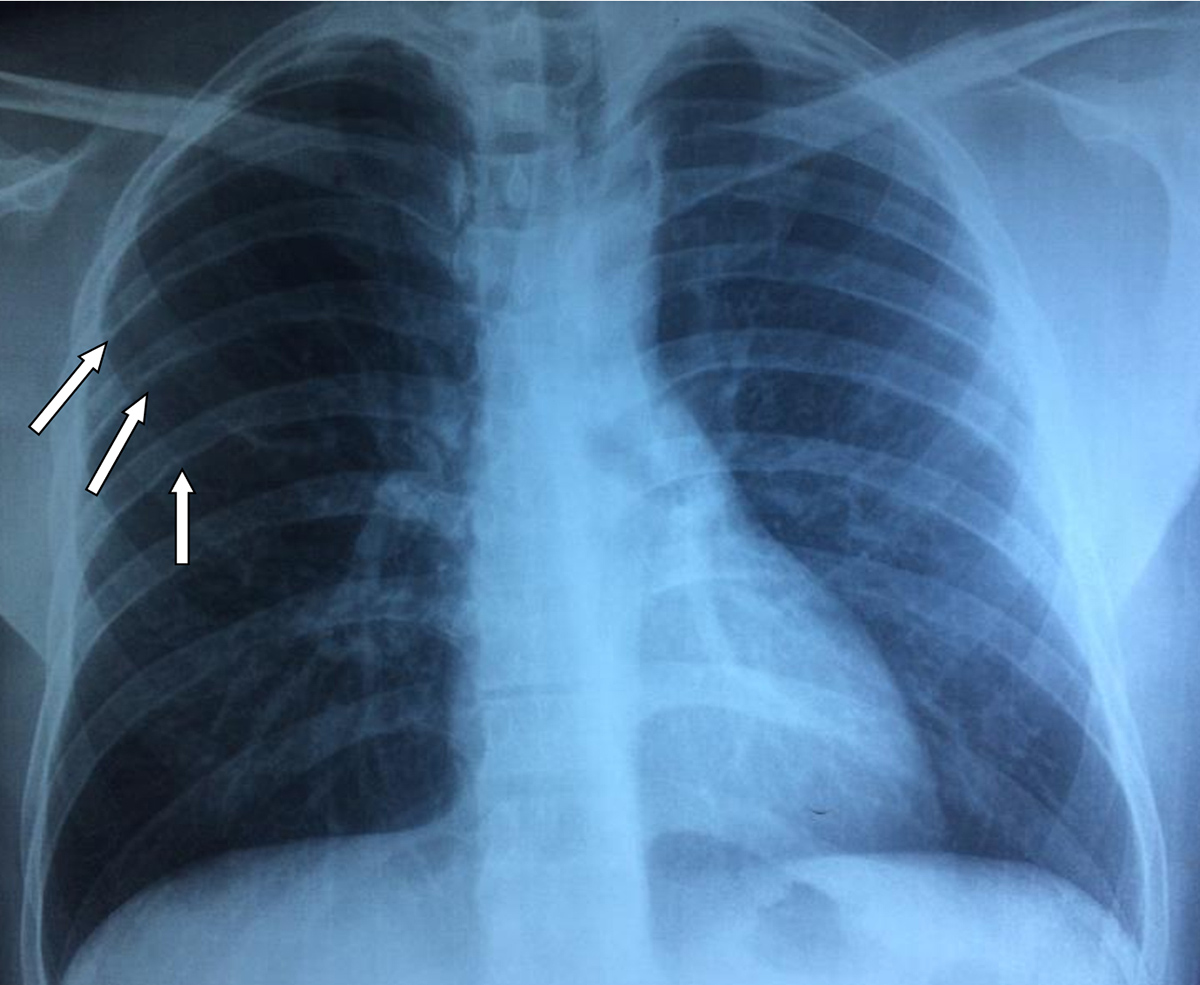
A 33-year-old man was admitted to our department for recurrent haemoptysis that started 2 weeks previously. The past medical history revealed that he had experienced a similar episode 6 years earlier, without investigation. He had a 5-pack-year smoking history. He did not complain of any other symptoms. On physical examination, blood pressure in the arms was 148/93 mmHg and oxygen saturation on room air was 98%. Blood test (complete blood count, chemistry and coagulation panels) results were within normal limits. A chest x-ray showed a mild left-sided tracheal deviation with notching of the ribs mainly in the right side (Fig. 1).
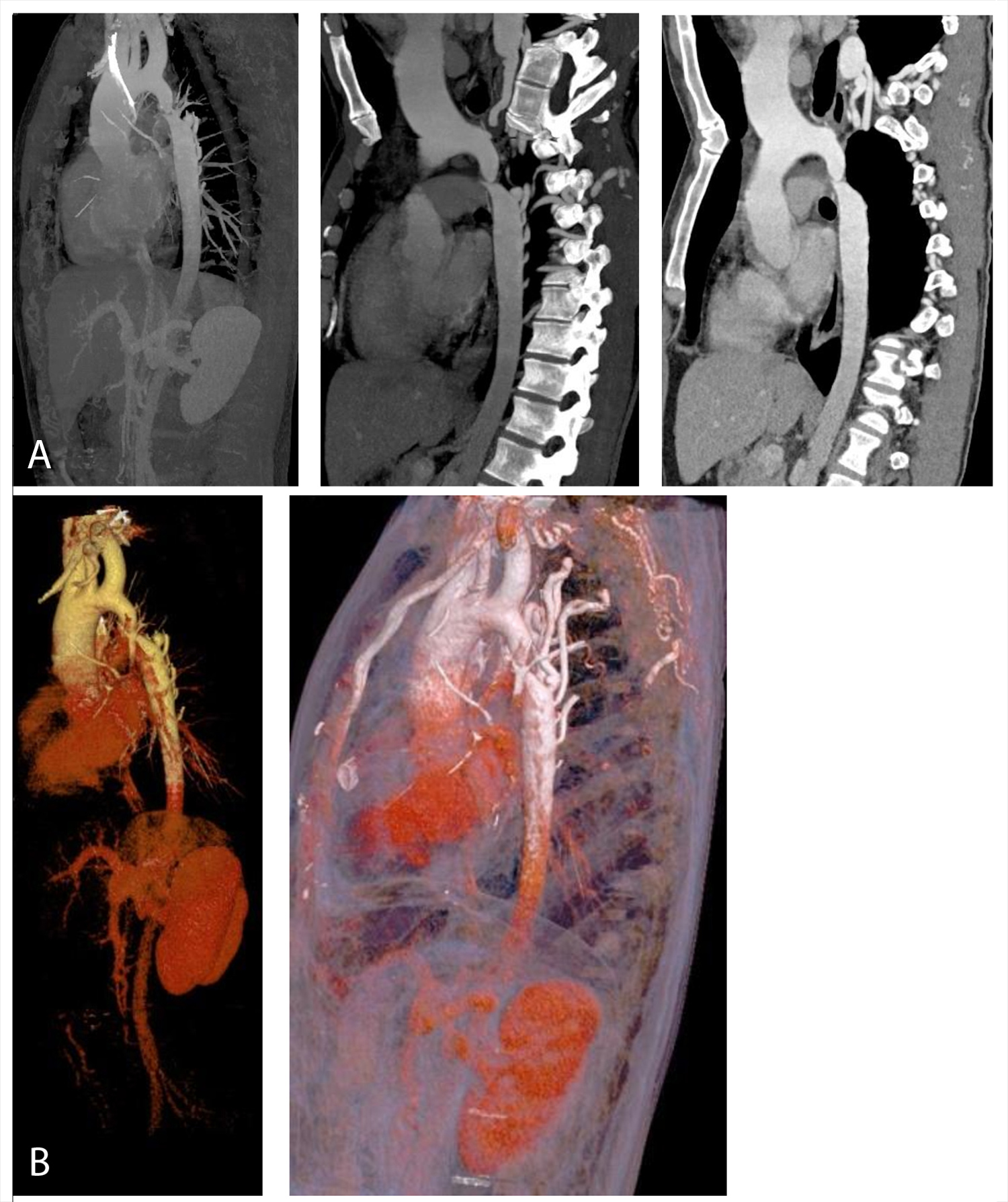
Electrocardiography was also normal. Fibreoptic bronchoscopy was conducted and no anomalies of the tracheobronchial tree were seen. A contrast-enhanced chest computed tomography (CT) scan revealed aortic coarctation with dilation of the internal mammary, intercostal and bronchial arteries (Fig. 2).
Figure 1. Chest x-ray: mild left-sided tracheal deviation with notching of the ribs mainly in the right side (white arrows)
Figure 2. Chest CT scan: sagittal section (a) and VR reconstruction (b) showing aorta coarctation with dilation of the internal mammary, intercostal and bronchial arteries
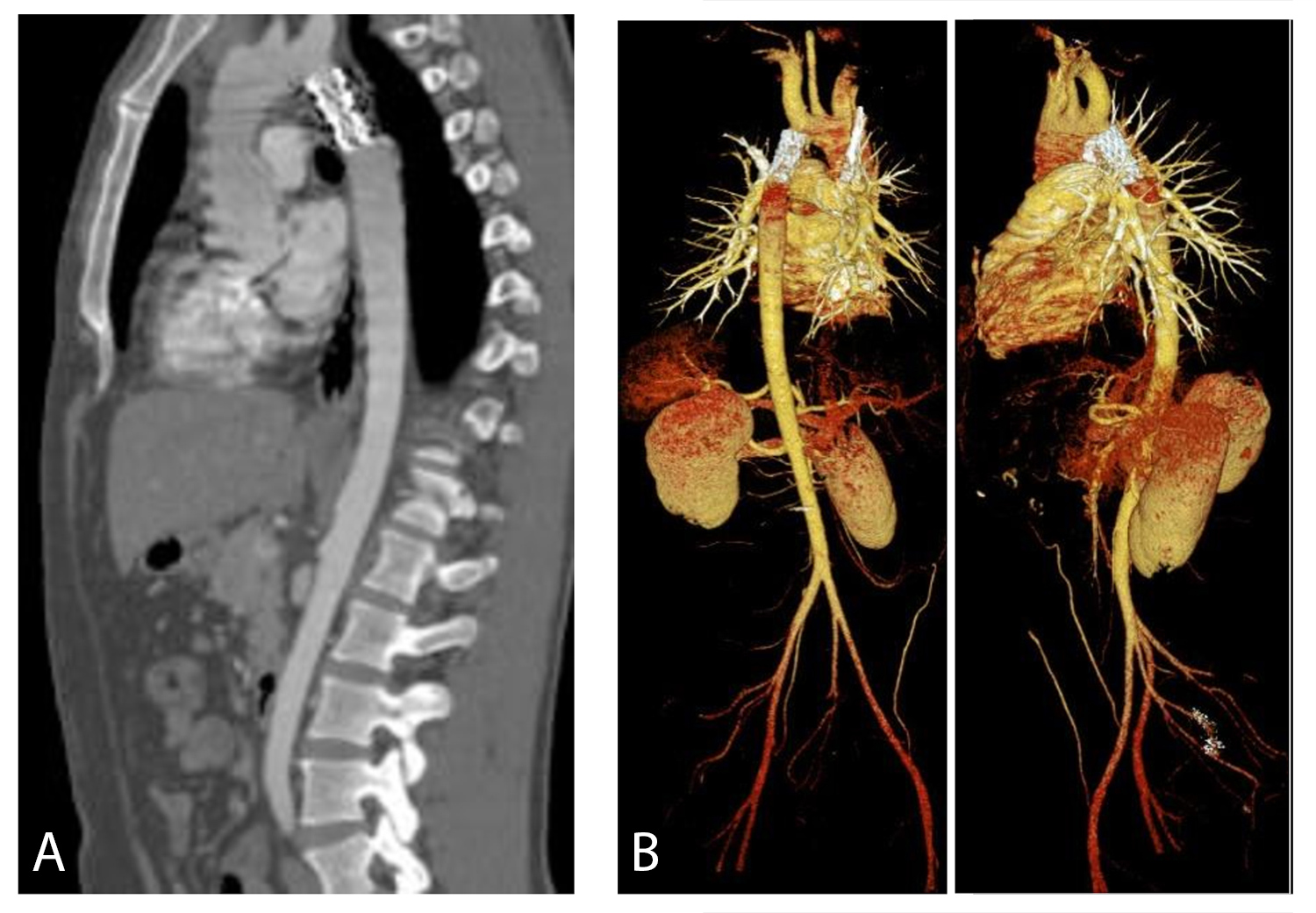
Echocardiography excluded other associated cardiac malformations. Aortography showed a long tight native aortic coarctation in the descending aorta with multiple collaterals. Regarding the hypertension, the patient was treated with a beta blocker and a calcium channel blocker. A stent placement (39 mm) under general anaesthesia after balloon angioplasty was successfully performed with a significant decrease of the peak-to-peak coarctation gradient from 100 to 50 and then to 10 mmHg after each procedure. A post-surgery CT scan showed the prosthesis in place and disappearance of dilation of the bronchial arteries (Fig. 3). The patient has not reported further haemoptysis.
Figure 3. Post-surgery CT scan showing the prosthesis in place and disappearance of dilation of the bronchial arteries (a: sagittal section; b: VR reconstruction)
DISCUSSION
Haemoptysis as a presenting and revealing sign of an aortic coarctation in an adult without any past medical history and no other associated clinical manifestations is an extremely rare condition. To the best of our knowledge, only a few cases are reported in the English-language literature and these were mainly associated with a post-surgery aortobronchial fistula. In fact, the latter is reported in some cases with a past history of aortic coarctation surgery [2]. Haemoptysis may occur several years after the intervention and due to aortic aneurysmal disease and the occurrence of an aortobronchial fistula [2]. It is associated with a high mortality risk (25–41%) [2]. Erolu-Günay et al. reported the first case of pulmonary arteriovenous fistula accompanying an aortic coarctation in a 16-year-old boy without any surgery history [3].
In this congenital cardiovascular context, the mechanical vascular obstruction leads to the development of bronchopulmonary collaterals with bronchial and systemic arterial hypertrophy [1]. High pressure with a weakened bronchial vessel wall results in haemoptysis [1]. Considering this increased intravascular pressure, Wightman et al. recently reported the first case of spontaneous bleeding from intercostal arteries with a history of coarctation repair due to spontaneous artery aneurysmal rupture [4].
A multidetector contrast-enhanced chest CT scan is a non-invasive imaging procedure for haemoptysis assessment and aetiological diagnosis in cases of vascular anomalies [1–3]. Fibreoptic bronchoscopy may show active haemorrhage or stigmata of recent bleeding [2].
Interventional methods for the treatment of cardiovascular anomalies such as aortic coarctation are currently preferred rather than invasive surgical procedures [2, 3, 5]. In fact, for adults, stenting the aortic coarctation is the preferred approach in different centres [5]. Outcomes after treatment are often favourable. However, a lifelong follow-up is necessary because of the possible long-term complications, such as vascular fistula, aneurysm or infection [5]. <7p>
CONCLUSION
In conclusion, although rare, congenital cardiovascular anomalies such as aortic coarctation should be considered in cases of haemoptysis even if the latter is the sole sign. A multidetector CT scan contributes significantly to the diagnosis. Interventional methods are efficient, safe and mini-invasive procedures to relieve symptoms and avoid fatal complications. After treatment, outcomes are often good despite the risk of haemoptysis recurrence in cases of infection or post-treatment aortobronchial fistula. Hence, a long-life follow-up is necessary.