ABSTRACT
Introduction: Recurrent deliberate sharp foreign body ingestion is associated with frequent hospitalizations and a high risk of complications, including perforation and peritonitis. These patients require urgent care. In addition, removal of foreign bodies can be challenging.
Case Description:We describe the case of a patient with borderline personality disorder who was admitted multiple times with sharps ingestion and presented challenges with her care.
Conclusion: Our case highlights the cause of recurrent sharps ingestion and provides recommendations on the retrieval of sharp foreign bodies and prevention.
LEARNING POINTS
- Recurrent sharps ingestion is associated with psychiatric illness.
- Ingested sharps can cause perforation and peritonitis, so urgent care is required.
- A multidisciplinary approach is necessary to care for these patients and prevent sharps ingestion in future.
KEYWORDS
Sharps, ingestion, endoscopy, psychiatry
INTRODUCTION
Repetitive deliberate foreign body ingestion (FBI) is a rare phenomenon reported mainly in patients with an underlying psychiatric disorder and often presents as an endoscopic emergency [1]. The management of these patients incurs a significant cost due to the repetitiveness of the event, and frequent and lengthy endoscopic procedures performed emergently in the operating room. FBI is associated with the risk of perforation, leading to mediastinitis or peritonitis. The patients require recurrent hospital visits, repeat retrieval procedures and prolonged hospitalization, and are associated with high healthcare utilization and costs [2]. We describe the case of a 38-year-old woman with recurrent admission for deliberate ingestion of sharp foreign bodies and the challenges associated with retrieval and prevention.
CASE DESCRIPTION
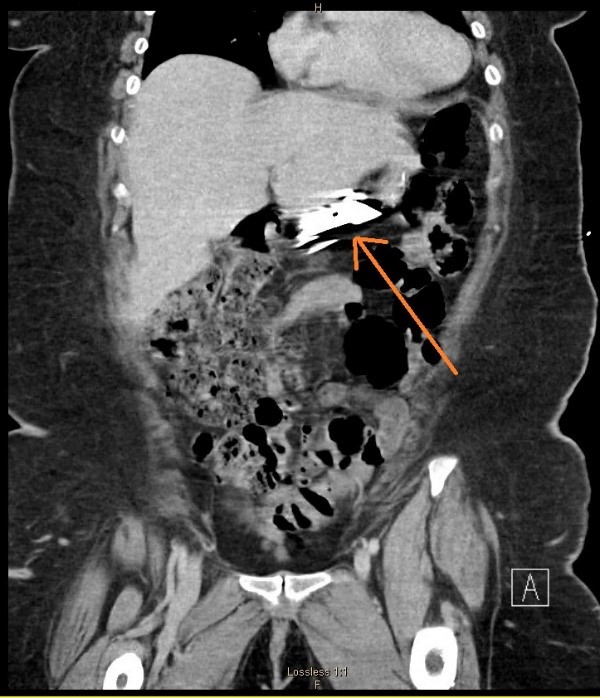
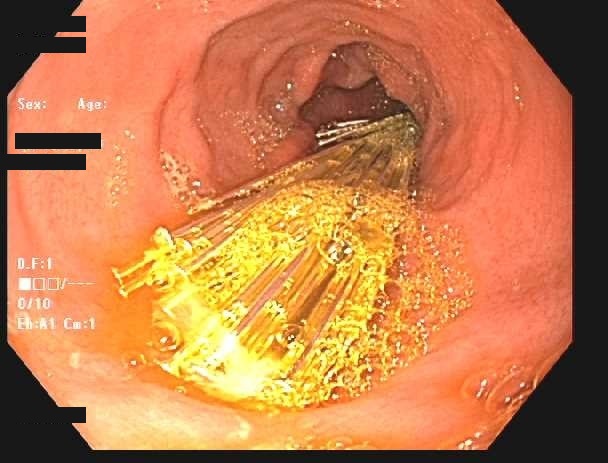
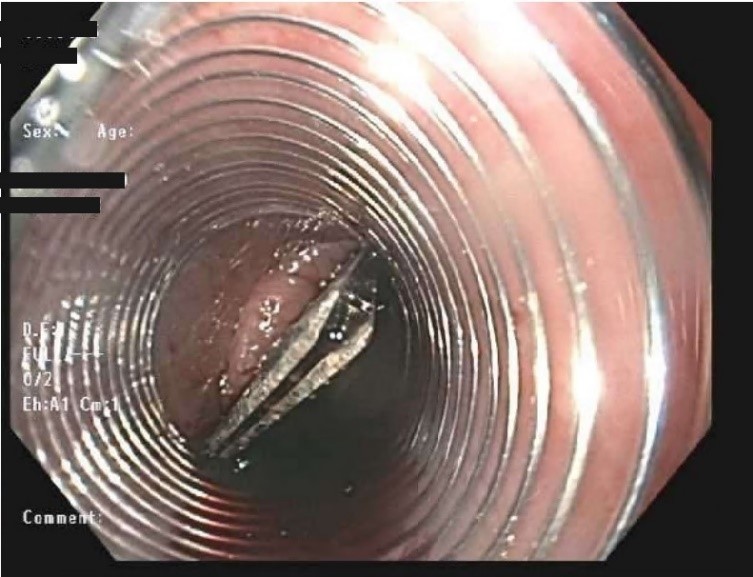
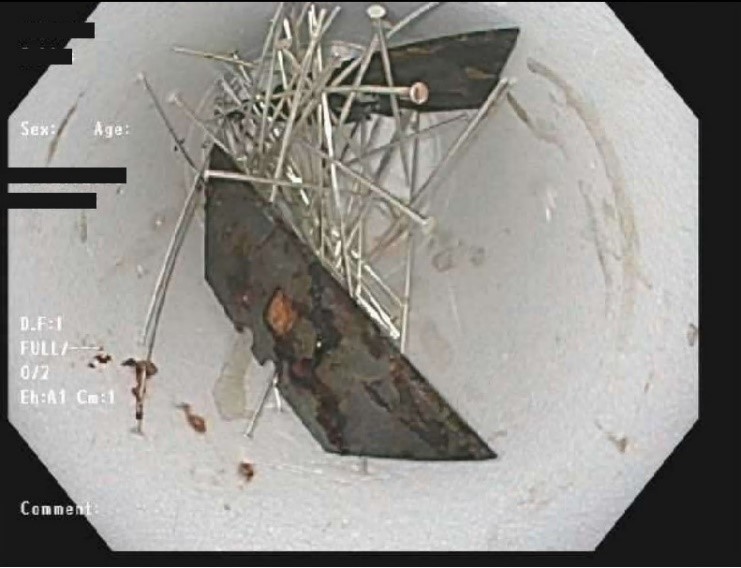
A 38-year-old woman with borderline personality disorder presented to the emergency room with abdominal pain and nausea. She admitted to ingesting sharp foreign bodies, including razor blades and needles. On physical examination, she appeared haemodynamically stable with mild epigastric tenderness without guarding or rebound tenderness. A CT scan of the abdomen revealed radiopaque objects in her stomach and duodenum (Fig. 1). There was no evidence of visceral perforation. Urgent esophagogastroduodenoscopy (EGD) was performed which revealed ingested sharp foreign bodies (Fig. 2). These were successfully retrieved using rat tooth forceps, snares and a long overtube to protect the oesophageal mucosa (Figs. 3 and 4).
Figure 1. CT scan showing a razor blade in the stomach
Figure 2. EGD showing pins embedded in the gastric body
Figure 3. Use of an overtube for the removal of sharp objects
Figure 4. Removed foreign bodies
The patient had been previously admitted to the hospital numerous times with a similar presentation. She had ingested foreign bodies, including glass, razor blades, safety pins, batteries, magnets and earrings. Her first hospital admission with FBI was 16 years earlier when she had ingested a paper clip and an open safety pin. Each episode of ingestion was preceded by severe anxiety or stressors, including verbal abuse by her mother. Following each ingestion episode, the patient was afraid of hurting herself internally and would visit the emergency room. During the previous 15 years, she had been admitted to our hospital 26 times (and multiple times to other hospitals in the community). In 2019 alone, she had undergone 23 CT scans for the investigation of ingested foreign bodies and EGD 9 times.
During each of these encounters, imaging studies were done to confirm the diagnosis and to determine the location of the foreign body. When feasible, the patient underwent endoscopy to retract the foreign body. In other instances, she was observed for several days with serial radiographs to confirm clear passage of the foreign bodies out of the GI tract. She required surgical consultation and laparotomy on six separate occasions.
DISCUSSION
Recurrent sharp FBI in adults is more commonly seen in patients with psychiatric illness such as borderline personality disorder, PTSD or in prisoners for secondary gain. It can be either intentional or unintentional, but intentional ingestion is more common in adults. Current guidelines recommend emergent removal (within 2–6 hours) of sharp foreign bodies, batteries or foreign bodies that cause obstruction in the oesophagus. Urgent removal (within 24 hours) is recommended for a foreign body in the oesophagus without complete obstruction, sharp objects in the stomach or duodenum, objects >6 cm in or above the proximal duodenum, and magnets that can be reached by an endoscope. Blunt rounded objects including coins, buttons or toys wider than 2.5 cm can be removed non-emergently [3, 4].
Sharp-pointed objects should be removed before they reach the small bowel as the risks of perforation are higher near the ileocecal valve. Surgical consultation should be sought if the sharp object fails to progress for more than 72 hours or the patient develops signs and symptoms of bowel perforation. In any type of FBI causing acute peritonitis, bowel perforation or bowel obstruction, surgical consultation should be obtained.
Retrieval devices available to remove foreign objects include rat-tooth and alligator forceps, a polypectomy snare, triprong grasper, Dormia basket, Roth Net and magnetic probes. Rat-toothed and alligator forceps can be used for small hard objects, while triprong graspers are preferred for soft objects such as a food bolus [3]. A Dormia basket and Roth Net are preferred for disk batteries. Long objects measuring more than 6 cm such as toothbrushes, spoons or forks, are better removed with snares or baskets. For sharp-pointed objects, rat-toothed and alligator forceps, a Roth Net or a polypectomy snare can be used. To prevent mucosal injury and protect the airway during the retrieval process, devices such as an overtube, a retractable latex-rubber condom-type hood and transparent distal caps can be used, as was done in our case for the retrieval of a razor blade. Using the sharp end of the foreign body as the trailing point will further reduce the risk of perforation [4]. Risk factors for repeat FBI include male sex, incarceration, and the presence of a psychiatric diagnosis. Repeated endoscopic removal of foreign bodies positively reinforces dysfunctional behaviour and hence results in recurrent and more complex ingestions [5]. Huang et al. studied 33 patients who recurrently ingested foreign bodies at Rhode Island Hospital from 2001 to 2009, and reported total estimated costs of over $2 million. Those 33 patients, the majority of whom had a psychiatric diagnosis, had 300 cases of recurrent FBI over the study period [2].
Very little is known about how to effectively prevent such episodes. An early and aggressive multidisciplinary approach which includes psychiatry consultation, behavioural therapy and pharmacotherapy remains crucial. Intensive outpatient treatment with close supervision is preferred because institutionalization may exacerbate underlying psychiatry illness and result in a longer hospital stay. Potentially effective pharmacological therapies include atypical antipsychotics (aripiprazole, ziprasidone), SNRIs (venlafaxine, buprenorphine), SSRIs (fluoxetine) and naltrexone [6].
CONCLUSION
Recurrent sharp FBI can be safely managed via flexible endoscopy with the use of appropriate accessories. A multidisciplinary approach addressing the patient's emotional and psychiatric stability and identifying provoking factors seems to be the best method to prevent relapses and readmissions, and reduce associated costs.