ABSTRACT
Segmental arterial mediolysis (SAM) is a non-inflammatory, non-atherosclerotic vasculopathy mostly involving the abdominal arteries. SAM was recently recognized as a more prevalent aetiology of abdominal pain than initially thought by healthcare providers. It is still a commonly missed diagnosis in patients with recurrent emergency room (ER) visits for abdominal pain. Most published case reports in the past have highlighted catastrophic sequelae such as intra-abdominal haemorrhage requiring surgical intervention. We report a case of SAM where the diagnosis was initially missed. After diagnosis, conservative medical management was offered which led to clinical improvement.
LEARNING POINTS
- To recognize segmental arterial mediolysis (SAM) as a cause of chronic abdominal pain in the middle-aged and elderly population.
- To differentiate SAM from inflammatory vasculitis and atherosclerotic conditions.
- For cases with mild symptoms and haemodynamic stability, conservative management such as early lifestyle modifications, hypertension and hyperlipidaemia control and regular imaging follow-up should be offered.
KEYWORDS
Segmental arterial mediolysis, chronic abdominal pain
CASE DESCRIPTION
A 47-year-old African American woman with a history of hypertension and migraine was seen in our outpatient clinic with a 1-year history of chronic, intermittent, postprandial diffuse abdominal pain. Pain was worse in the epigastric and hypochondriac regions. It was associated with chronic diarrhoea and dyspepsia, but no melena, haematochezia or haematemesis was reported. She also reported 40 pounds of unintentional weight loss in 1 year. The blood count and metabolic panel were within the normal ranges. Helicobacter pylori testing, coeliac disease testing, and antinuclear antibody and antineutrophil cytoplasmic antibody screens were negative. The patient’s symptoms did not show much improvement with 8 weeks of twice daily proton pump inhibitor therapy. Abdominal ultrasonography was unremarkable and a hepatobiliary iminodiacetic acid (HIDA) scan showed normal gallbladder motility and ejection.
Oesophagogastroduodenoscopy and colonoscopy showed benign gastric polyps, small haemorrhoids and diverticulosis, which did not explain the patient's symptoms. Duodenal, gastric and colonic biopsies were unremarkable. By this time, irritable bowel syndrome or functional abdominal pain were considered likely differential diagnoses, so amitriptyline was prescribed but the patient did not tolerate it due to somnolence. Diagnostic tests, imaging, procedures and treatment trials were conducted over 2.5 years without a definitive diagnosis while the patient continued to have intermittent symptoms.
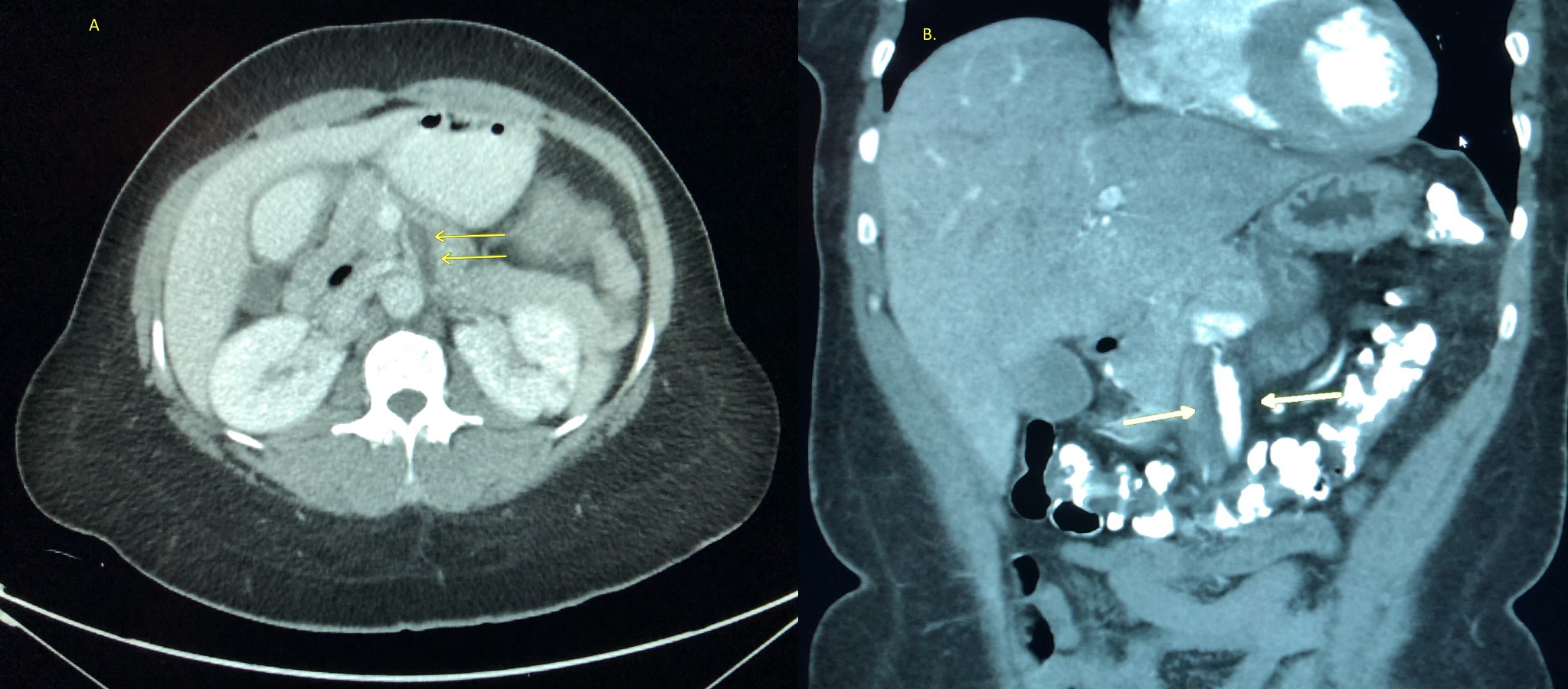
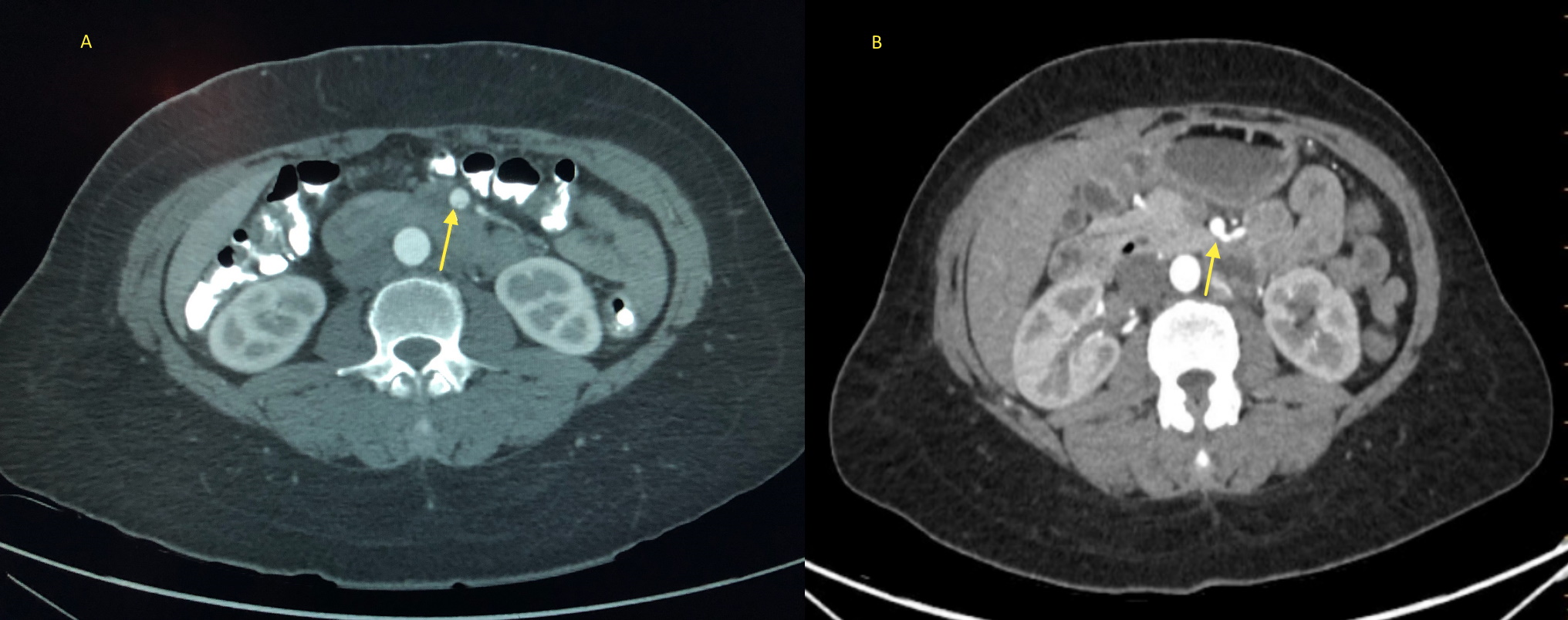
The patient was next seen in the ER with nausea, vomiting, and acute worsening of abdominal pain. During this visit, a repeat blood count, metabolic panel, lipase level, urine drug screen and lactic acid levels were all within the normal ranges. Computed tomography (CT) of the abdomen showed an eccentric thrombus within the proximal superior mesenteric artery (SMA) causing focal moderate to severe luminal stenosis, with distal reconstitution. CT angiography (CTA) of the abdomen was done which showed eccentric wall thickening causing moderate to severe stenosis of the proximal SMA. A long segment intimal dissection flap was seen arising within the mid to distal SMA. Multifocal irregular wall thickening extended to the distal SMA, in a pattern typical of SAM (Figs. 1 and 2). Terminal branches of the SMA were patent and there was no evidence of visceral ischaemia or haemorrhage. A diagnosis of SAM was established based on imaging findings and exclusion of other causes. The patient was discharged with a prescription of daily low-dose aspirin and atorvastatin with recommendations of close follow-up with CTA imaging. A follow-up CTA of the abdomen after 8 weeks showed interval improvement in distal SMA dissection but no change in proximal SMA stenosis (Fig. 3).
Figure 1 (Left) Axial abdominal computed tomography image with contrast demonstrating eccentric, low-attenuating wall thickening (arrows) in the proximal superior mesenteric artery (SMA) contributing to focal luminal narrowing. (Right) Coronal image showing irregular wall thickening (arrows) and proximal SMA stenosis in a pattern typical of segmental arterial mediolysis (SAM)
Figure 2. (Left) Axial view of computed tomography angiogram showing a cross-section of a long-segment intimal dissection flap (arrow) in the distal superior mesenteric artery (SMA). (Right) Follow-up computed tomography angiogram with axial image showing improvement of the distal SMA dissection (arrow)
Figure 3. (left) Computed tomography angiogram with coronal image showing unchanged proximal superior mesenteric artery (SMA) irregular wall thickening (arrows) and stenosis. (right) 3D Reconstruction image of abdominal arteries showing SMA stenosis (arrow)
DISCUSSION
PSAM is a non-inflammatory, non-atherosclerotic vasculopathy of unclear aetiology, with a propensity to involve splanchnic vessels but it can also affect carotid, renal and intracranial vessels. Arterial vasospasm is thought to lead to dissection of arterial walls, although the exact pathogenesis of the disease remains unclear [1]. Another pathophysiological mechanism suggested is vacuolar degeneration leading to disruption of the outer arterial media eventually causing aneurysms and dissections. SAM mainly affects middle-aged and elderly patients. Abdominal pain is the most common clinical presentation, while it can also present as shock due to haemorrhage, haematochezia, chest pain or stroke. Patients presenting with acute intra-abdominal bleeding are most commonly reported, but less dramatic presentations as seen in our patient are more rarely highlighted in the scholarly literature.
Endovascular therapies are recommended as the first-line treatment modality in patients with haemodynamic instability or evidence of end-organ ischaemia. Several authors have published cases with initial presentations of intra-abdominal bleeds requiring surgical intervention, but in recent studies there has been a shift in focus towards conservative management of mildly symptomatic cases that can now be diagnosed earlier with advancement in imaging techniques [2]. There was another similar case at our centre where the patient was admitted with abdominal pain in the absence of haemorrhagic complications [3]. The most common imaging finding on CTA is dissection of mesenteric vessels. Other typical findings suggestive of SAM on CTA are non-atherosclerotic arterial mural wall thickening with a multifocal skip pattern of luminal strictures and post stenotic aneurysmal dilatation of arteries as seen in our patient [4]. Imaging findings can appear very similar to inflammatory vasculitis and therefore autoimmune work-up should be performed to rule out such aetiologies.
No clear management guidelines exist due to the paucity of randomized controlled trials. The current proposed management is based mostly on single-centre case studies. Patients presenting with haemorrhage or acute bowel ischaemia frequently warrant coil embolization or surgery, but a substantial number of cases are stable and can be managed conservatively with lifestyle modification. CTA follow-up for monitoring disease progression has also been suggested [4]. Interestingly, studies have shown that in most cases, follow-up imaging findings remain stable [5]. Naidu et al. in a study of 111 cases reported that even with progression noted on imaging, no deaths were reported [2]. Therefore, a disease that was initially thought to be catastrophic is now considered to be a self-limiting condition in most instances. Early imaging with CTA in patients presenting with unexplained persistent abdominal discomfort can help physicians make an appropriate diagnosis, suggest lifestyle modifications, and improve outcome without surgical intervention.