ABSTRACT
We describe the case of a 66-year-old woman with littoral cell angioma (LCA) confirmed by histopathology and immunohistochemistry, to our knowledge the first case in Belgium. LCA is an extremely rare primary vascular tumour of the splenic red pulp, probably originating from littoral cells. If a splenic mass and nodules are incidentally identified on imaging and the patient has no associated signs or symptoms, LCA should be suspected. Histopathology and adjacent techniques are mandatory for definitive diagnosis. Splenectomy followed by adequate follow-up is necessary to exclude underlying pathology.
LEARNING POINTS
- Littoral cell tumour, although a very rare neoplasm, must be included in the differential diagnosis of splenic lesions observed by imaging.
- As imaging cannot differentiate between benign and malignant lesions, a definitive diagnosis is made only by histopathology and immunohistochemistry.
- Individuals diagnosed with littoral cell angioma must be carefully evaluated to exclude associated primary, secondary and synchronous malignancies as well as accompanying inflammatory/autoimmune disease.
KEYWORDS
Littoral cell tumour, spleen, CT scan, immunohistochemistry
CASE DESCRIPTION
A 66-year-old woman presented with complaints of recent epigastric pain radiating towards the back. There were no other symptoms and no significant personal history. Physical examination and blood results did not show any abnormalities. Neither splenomegaly nor pathological lymph nodes were observed.
Gastro-duodenoscopy revealed a pyloric ulcer 1 cm in diameter with hematin. Biopsies confirmed the benign nature of the ulcer and revealed the presence of Helicobacter pylori.
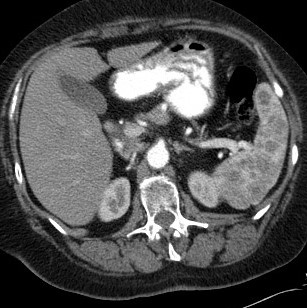
A contrast-enhanced CT scan of the abdomen in the arterial phase demonstrated multiple slightly irregular delineated and partly confluent round, hypodense lesions in the spleen, ranging in size from subcentimetric up to 2.3 cm (Fig. 1). The portal-venous phase showed a less obvious hypodense aspect, so the lesions demonstrated some progressive (slightly inhomogeneous) contrast enhancement, later than normal splenic parenchyma (Fig. 2). There was no splenomegaly or signs of abdominal malignancy.
Figure 1. Axial contrast-enhanced CT in the arterial phase showed multiple, slightly irregular delineated and partly confluent round, hypodense lesions in the spleen. Spleen volume was normal
Figure 2. Axial contrast-enhanced CT in the portal-venous phase showed multiple hypodense lesions which were less hypodense compared with the arterial phase, so the lesion demonstrated some progressive contrast enhancement
The multi-focal spleen lesions posed a problem with the differential diagnosis, which included lymphoproliferative disease, granulomatous disease (tuberculosis, sarcoidosis, etc.), disseminated infection (fungi, Pneumocystis jirovecii, etc.), metastasis and, to a lesser extent, haemangioma, splenic cysts and splenic infarction.
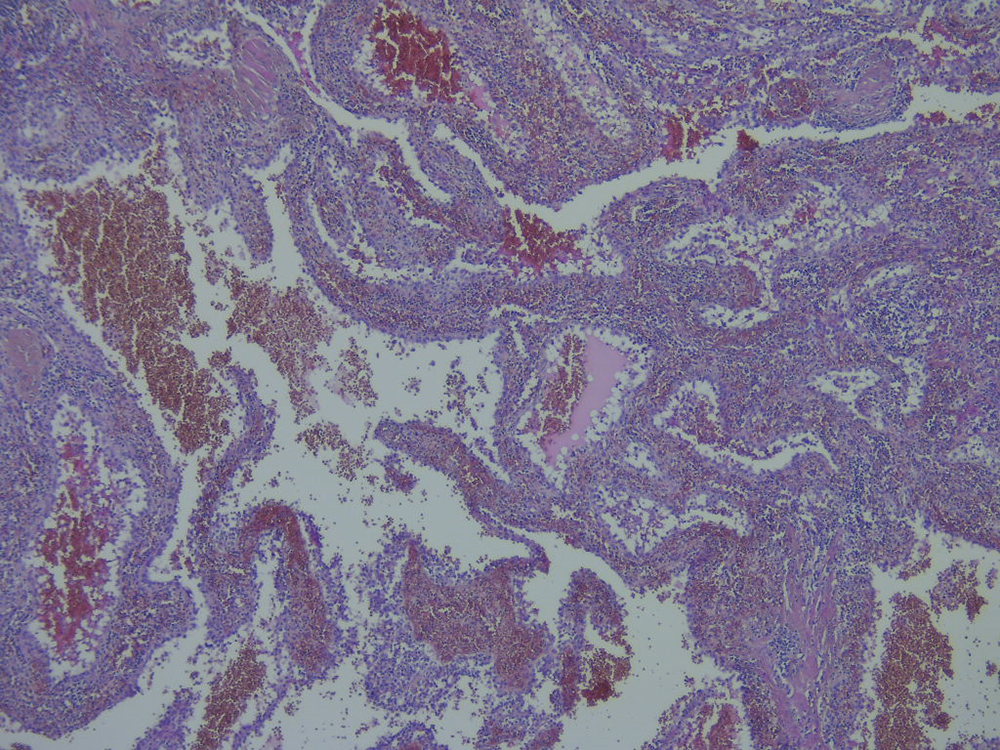
After multi-disciplinary discussion, a laparoscopic splenectomy was performed to obtain a diagnosis. On histopathological examination, the spleen consisted of several fragments measuring from 1 cm up to 3.5×2.0×1.8 cm and weighing 180 g, with several subcapsular bluish/red-black sharply demarcated nodules up to 2.5 cm in diameter. These nodules partially replaced the spleen tissue and consisted of multiple vascular lumina lined with relatively plump rounded to cuboidal littoral cells (Fig. 3).
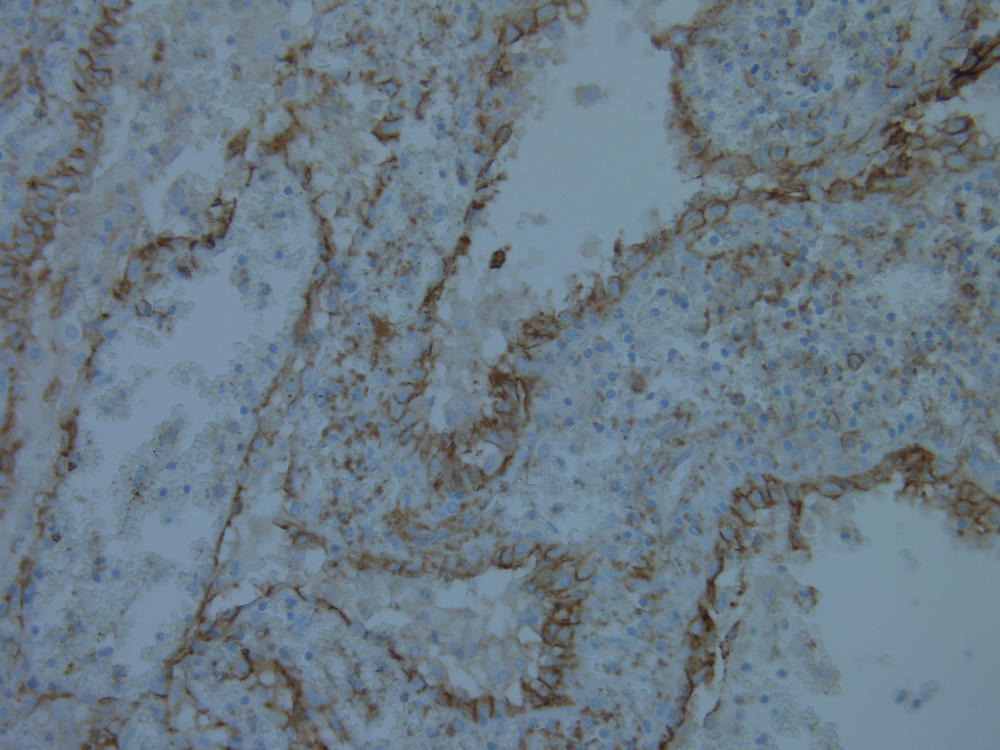
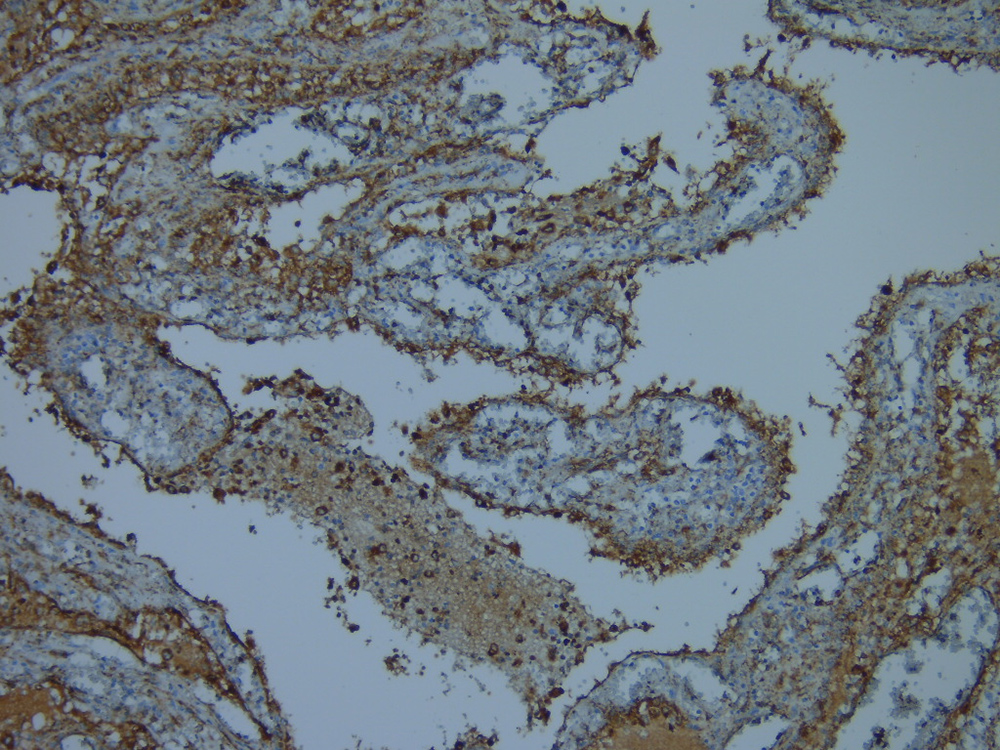
Immunohistochemistry displayed immunoreactivity for endothelial markers CD31 and FVIII, as well as for histiocytic markers including CD68, CD163 and alpha-1-anti-trypsin, confirming the littoral cell origin (Figs. 4 and 5).
Flow cytometry did not reveal any aberrant T- or B-cell populations, which was confirmed by molecular analysis for heavy chain Ig and T-cell receptor.
The follow-up period of more than 8 years was uneventful and CT imaging showed no abnormalities.
Figure 3. Splenic nodular lesion consisting of anastomosing lumina lined by plump rounded to cuboidal histiocytic–endothelial littoral cells (haematoxylin-eosin staining, magnification: 100×)
Figure 4. Strong membrane staining of littoral cells with anti-CD31 mouse monoclonal antibody confirming endothelial differentiation (magnification: 200×)
Figure 5. Strong cytoplasmic staining of littoral cells with anti-CD68 mouse monoclonal antibody confirming histiocytic differentiation (magnification: 200×)
DISCUSSION
Vascular neoplasms such as haemangiomas are the most common non-lymphoid tumours of the spleen, which include the extremely rare littoral cell angioma (LCA). We have analysed a total of 150 patients with a diagnosis of LCA from 1991 to May 2020 described in English language journals. The majority of cases reported are from the Asian continent.
LCA was first described by Falck et al. in 1991 [1]. They reported 200 vascular neoplasms of the spleen and identified 17 vascular tumours characterized by the cells lining the red pulp splenic sinuses, thereby fulfilling the criteria for LCA. This lesion is unique to the spleen and does not appear to possess a soft tissue or lymph node counterpart. Because of its rarity, the actual incidence rate remains unclear. Up to now, limited cases have been reported. The largest series of described cases consists of 25 patients [2]. LCA is in most cases asymptomatic and discovered incidentally. Most studies describe no age or sex preference.
Some patients present with symptoms of hypersplenism such as anaemia, thrombocytopenia and splenomegaly [3]. Our patient only complained of recent epigastric pain radiating towards the back, probably caused by the pyloric ulcer. The LCA was discovered incidentally on radiological imaging.
In most cases, early-phase contrast-enhanced CT showed multiple low-attenuating nodules of varying size (0.2–6 cm) with progressive homogeneous contrast enhancement later than the normal splenic parenchyma. On delayed images, the nodules were isodense with the surrounding enhancing splenic tissue [4]. Sometimes they present as a solitary lesion, usually there is splenomegaly, and in advanced cases splenic rupture and haemoperitoneum can occur.
Sonography is rarely helpful and MRI may further help in the diagnosis, but at present radiological methods cannot achieve a definite diagnosis of LCA because of the similar appearance of benign and malignant tumours of the spleen.
Most studies describe LCA as a benign tumour, although some mention the presence of malignancy. This raises the question whether those cases that appear malignant were in fact littoral cell haemangioendotheliomas or littoral cell haemangiosarcomas instead of LCA. Definitive evaluation can only be achieved by histopathological examination revealing multiple anastomosing lumina lined by tall to plump cuboidal endothelial cells. No atypical cells or mitosis are seen. Immunohistochemistry is positive for endothelial markers such as CD31, FVIII, ETS-related gene (ERG), VEGFR2, VEGFR3 and claudin-5, as well as histiocytic lineage markers such as CD68, lysozyme, alpha-1-anti-trypsin, CD21 and CD163. The immunoreactivity for both endothelial markers and histiocytic markers confirms the endothelial–histiocytic differentiation characteristic for splenic littoral cells [3].
In the literature, approximately one third of LCA cases were accompanied by malignancies such as lung cancer, gastro-intestinal cancer, genito-urinary cancer, melanoma, lymphoma and sarcoma [2]. In another third, immune dysregulation was found, including ankylosing spondylitis, psoriasis, Castleman’s disease, lymphocytic colitis, SLE and Crohn’s disease. These findings suggest a possible relationship between LCA and malignancy, chronic inflammation and autoimmune disease, possibly a TNF-alpha-related pathogenesis.
CONCLUSION
We conclude that LCA is an extremely rare primary vascular tumour of the splenic red pulp, probably originating from littoral cells. If a splenic mass and nodules are incidentally identified on imaging and the patient has no associated signs or symptoms, LCA should be suspected. Histopathology and adjacent techniques are mandatory for definitive diagnosis. Splenectomy followed by adequate follow-up is necessary to exclude underlying pathologies.