ABSTRACT
Background: Paliperidone and mirtazapine are psychotropic agents associated with proarrhythmic effects.
Case Presentation: A 21-year-old woman was admitted to the intensive care unit on two separate occasions for attempting suicide by overdosing on paliperidone and mirtazapine. During both admissions, the patient had atypical chest pain and a first-degree atrioventricular block (AVB) with paradoxical sinus tachycardia, which resolved with the discontinuation of paliperidone and mirtazapine and aggressive intravenous fluids.
Conclusion: Drug-induced first-degree AVB from paliperidone and mirtazapine should be on the differential diagnosis in patients on paliperidone and/or mirtazapine who present with chest pain, tachycardia or new-onset first-degree AVB.
LEARNING POINTS
- Paliperidone and mirtazapine are associated with first-degree heart block, which may be a harbinger of torsades de pointes and ventricular fibrillation.
- CytomegaloPaliperidone and mirtazapine may potentiate each other’s proarrhythmic effects since the metabolism of both involve the cytochrome P450 2D6 enzyme.
- A history of psychiatric illness makes it difficult to rule out atypical chest pain without ECG or troponins and often leads to increased resource utilization, even during times of heavy use like the COVID-19 pandemic.
KEYWORDS
Atrioventricular block, paliperidone
CASE DESCRIPTION
A 21-year-old woman with bipolar disorder with psychotic features, migraines and dyslipidaemia presented to the emergency department (ED) after an attempt at suicide by overdosing on 7 of her 6 mg extended-release paliperidone tablets, 20 of her 3 mg cariprazine tablets, 7 of her 15 mg mirtazapine tablets, 2 of her 100 mg sumatriptan tablets, 7 of her 50 mg topiramate tablets, and 2 of her 220 mg naproxen tablets after an argument with her parents. Conservative management was elected, and the patient was admitted to the psychiatric hospital on a voluntary basis.
She subsequently experienced tachycardia, palpitations and atypical chest pain in her right shoulder with radiation to her sternum, jaw and right arm. In turn, the patient was brought back to the ED for a second time. While in the ED, the patient's heart rate ranged from 90 to 140 beats per minute. Physical examination was pertinent for sinus tachycardia and chest wall tenderness that was reproducible on examination.
The highest item on the initial differential diagnosis was drug-induced sinus tachycardia as the patient took multiple medications with the known adverse effect of tachycardia. There was likely comorbid psychogenic chest pain given her significant psychiatric history. Acute coronary syndrome was less likely given her age and tenderness to palpation.
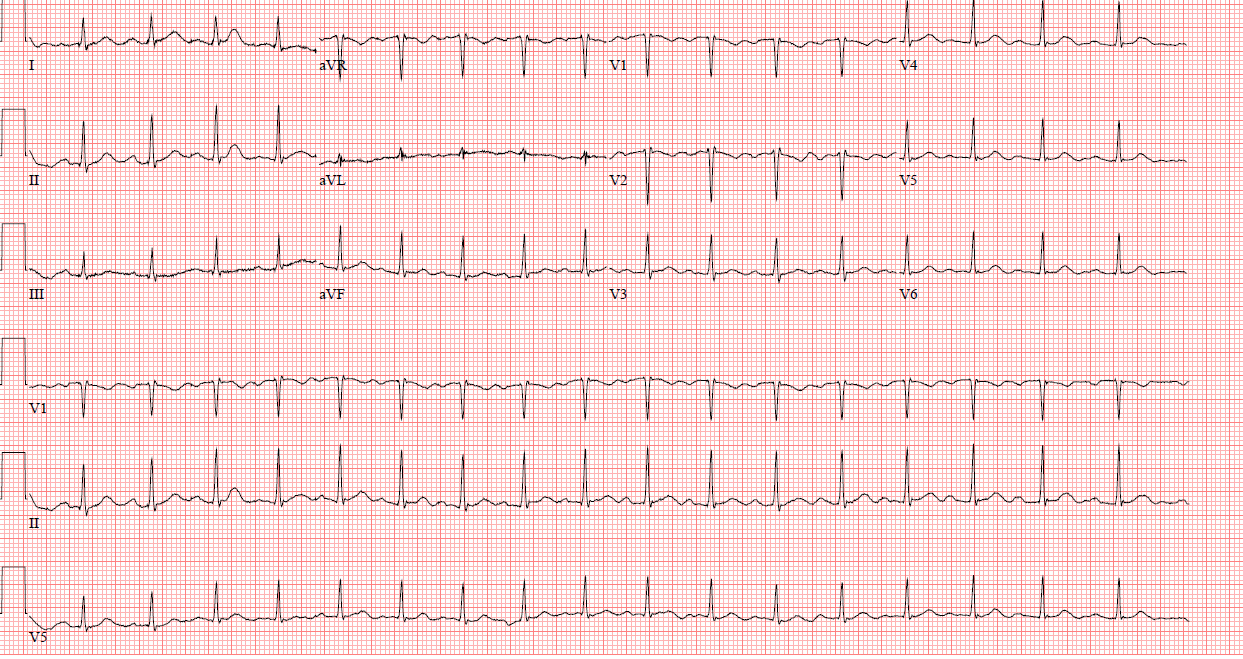
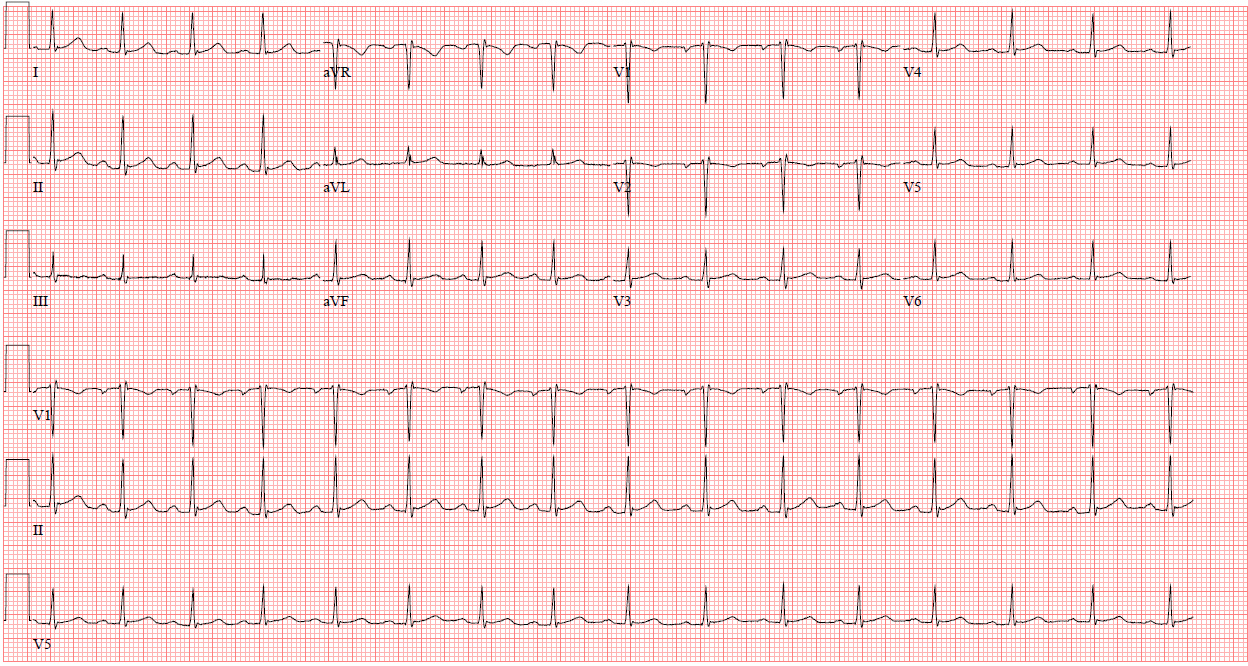
Initial investigations of electrolytes, thyroid stimulating hormone, free thyroxine and serial troponins were within normal limits. ECG indicated a PR interval of 206 ms (Fig. 1). Chest radiograph and echocardiogram were non-revealing. In the setting of acute polypharmacy overdose, copious amounts of intravenous fluids were started. Repeat ECG indicated a PR interval ranging from 150 to 190 ms (Fig. 2). The patient was then transferred back to the psychiatric hospital. Paliperidone was discontinued, and the patient was discharged on aripiprazole, topiramate and mirtazapine.
Figure 1. Electrocardiogram during the first admission indicating a first-degree atrioventricular block with a PR interval of 206 ms after overdosing on paliperidone and mirtazapine
Figure 2. Electrocardiogram during the first admission indicating termination of the first-degree atrioventricular block after aggressive intravenous fluids. PR interval is 184 ms
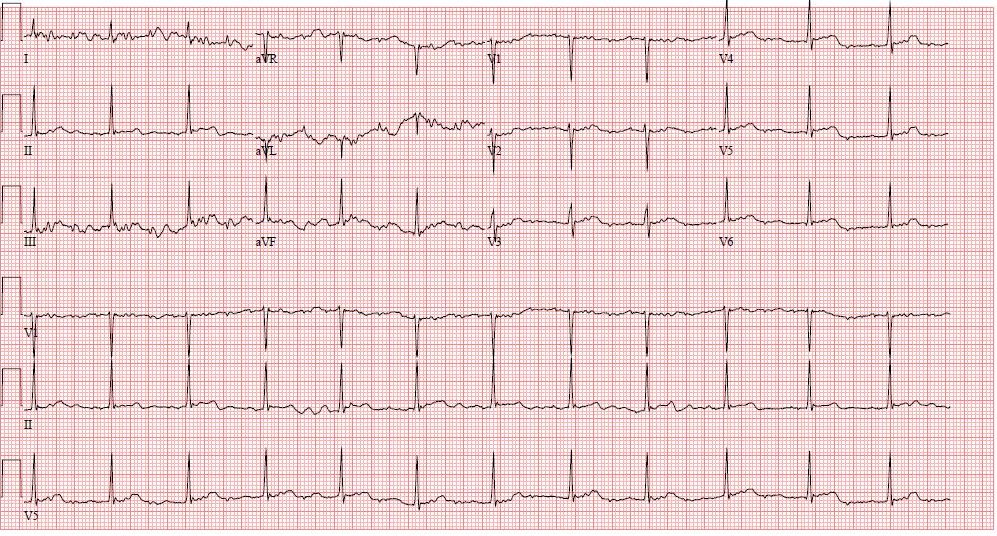
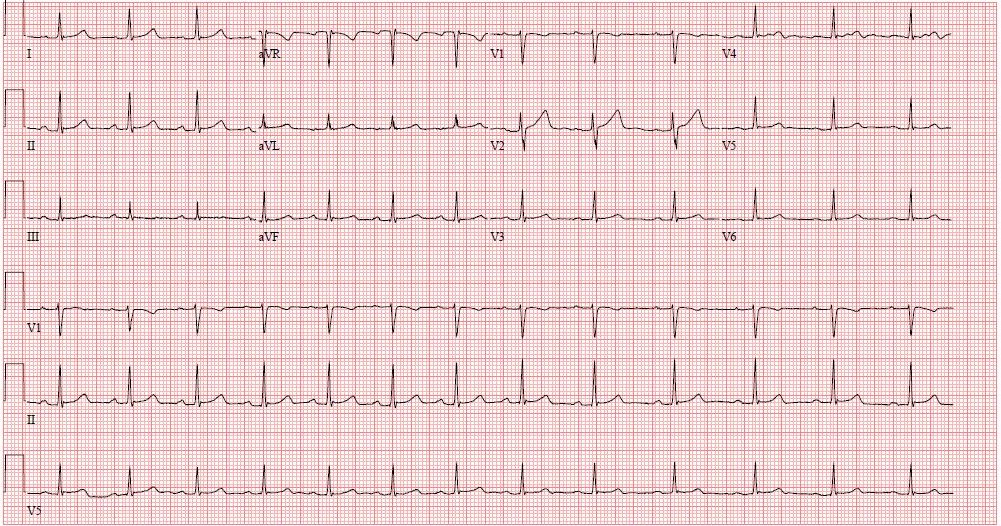
About 2 months later, the patient attempted suicide again by overdosing on an unknown amount of paliperidone and mirtazapine. She presented to the ED with similar atypical chest pain. An ECG indicated a PR interval of >220 ms (Fig. 3). She was admitted to the intensive care unit again and given copious amounts of intravenous fluids. The repeat ECG indicated a PR interval that subsequently decreased to 186 ms, and she was transferred to the psychiatric hospital on a voluntary basis (Fig. 4). The patient was discharged on buspirone, oxcarbazepine, hydroxyzine and trazodone.
Figure 3. Electrocardiography during the second admission indicating a recurrent first-degree atrioventricular block with a PR interval of >220 ms after overdosing on paliperidone and mirtazapine
Figure 4. Electrocardiogram during the second admission indicating termination of the first-degree atrioventricular block with a PR interval of 186 ms
DISCUSSION
The development and termination of the first-degree AVB with starting and discontinuing supratherapeutic doses of paliperidone and mirtazapine strongly suggest that these agents are responsible for the development of the first-degree AVB in this patient. The reproducibility of the same consistent PR prolonging effect on two separate occasions with both paliperidone and mirtazapine further demonstrates the proarrhythmic effects of these psychotropic agents. They may potentiate each other’s proarrhythmic effects since the cytochrome P450 2D6 enzyme is involved in their metabolism [1, 2].
Diagnostic investigations may include monitoring electrolytes, serial troponins, ECG, chest radiograph and echocardiogram. First-degree AVB due to paliperidone or mirtazapine is a diagnosis of exclusion. Patients should have a thorough work-up to rule out more common causes, including myocardial infarction, cardiomyopathy, fibrosis, or other PR prolonging medications, such as beta-blockers and calcium-channel blockers [3]. Treatment includes discontinuing the offending agent and copious intravenous fluids. For mirtazapine specifically, arrhythmias can be treated initially with bicarbonate and lidocaine if refractory to bicarbonate. Benzodiazepines and antiepileptic drugs can be used in patients who develop seizures, and patients may require intubation from acute respiratory failure [4].
Paliperidone and mirtazapine are associated with higher degrees of AVB, bundle branch blocks, QT prolongation, torsades de pointes and ventricular fibrillation [4–7]. A dose-dependent proarrhythmic effect can be seen with ventricular arrhythmias in paliperidone [7]. Although first-degree AVB itself is typically benign, we postulate that it may serve as a harbinger of potentially deadly arrhythmias in patients that overdose on paliperidone given its dose-dependent proarrhythmic nature [7, 8]. However, more research is needed to investigate this.
CONCLUSION
Drug-induced first-degree AVB from paliperidone and mirtazapine should be on the differential diagnosis in patients on paliperidone and/or mirtazapine who present with a new first-degree AVB after other causes have been ruled out. More research on the cardiac effects of paliperidone and mirtazapine should be conducted.