ABSTRACT
Nocardia is a genus of aerobic, non-motile and non-spore-forming filamentous branching bacteria with fragmentation into bacillary or coccoid forms. Infections caused by Nocardia often occur in immunocompromised hosts and are potentially life-threatening. Nocardia beijingensis has rarely been reported to cause infection in immunocompetent hosts. We present a case of disseminated infection due to Nocardia beijingensis in a patient with no known medical comorbidities, who presented with new-onset seizure. Another interesting finding in our case is that our patient did not have any pulmonary symptoms despite chest CT showing the pulmonary system as the likely primary site of infection. As per our literature review, this is the seventh reported case of infection due to Nocardia beijingensis in an immunocompetent host.
LEARNING POINTS
- To recognize Nocardia beijingensis, a slow-growing weakly acid-fast filamentous bacteria commonly causing opportunistic infections in immunocompromised hosts, as an emerging pathogen in immunocompetent patients.
- Tissue biopsy with Gram staining showing variable filamentous bacteria and confirmation of species using restriction enzyme analysis and 16S rRNA analysis is needed to establish a diagnosis of infection.
- Trimethoprim/sulfamethoxazole has been successfully used to treat infection due to Nocardia beijingensis.
KEYWORDS
Infectious diseases, disseminated Nocardia infection, Nocardia beijingensis infection, immunocompetent
CASE PRESENTATION
A 57-year-old non-smoker, non-diabetic female with no known comorbidities presented after a motor vehicle accident following seizure-like activity while driving her car into a house, followed by post-ictal confusion. The patient had no preceding symptoms of shortness of breath, cough, fever, headache or chills. There was no history of recent travel outside the state of Illinois, USA. She reported no recent dental procedures. She denied alcohol or recreational drug use. Family history was non-contributory.
Methods and Procedures
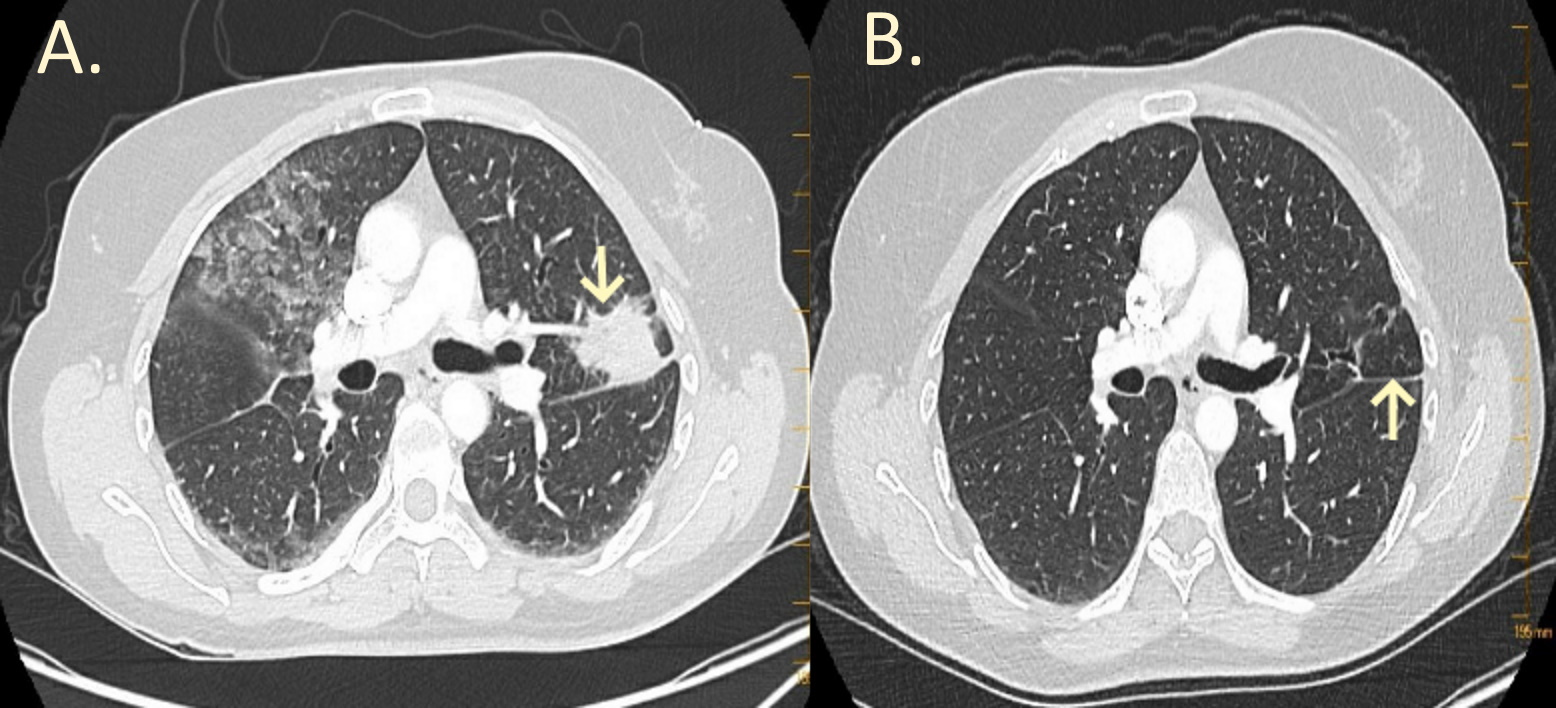
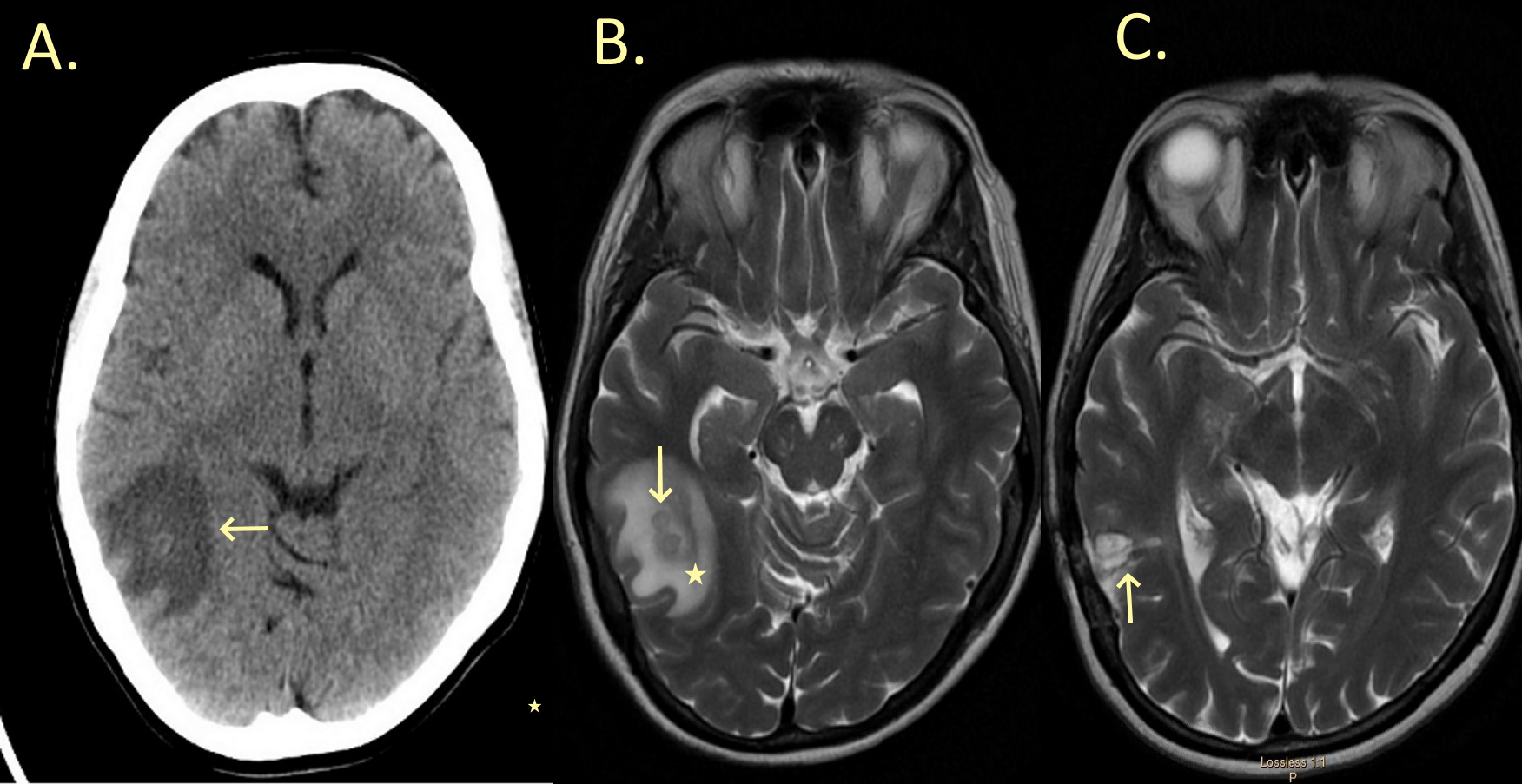
Laboratory results revealed mild leucocytosis with neutrophil predominance. Blood cultures showed no growth. Computed tomography (CT) of the head, chest, abdomen and pelvis was carried out based on trauma protocol. Chest CT revealed a left upper lobe spiculated mass (Fig. 1A). Head CT showed a focus of high attenuation in the right temporal region (Fig. 2A). Brain MRI showed a right temporo-occipital bilobed lesion with ring peripheral enhancement and surrounding vasogenic oedema (Fig. 2B). The patient was started on intravenous ceftriaxone and intravenous vancomycin based on brain imaging findings and concern for underlying cerebral abscess. Lung biopsy was performed showing granulomatous disease with biopsy cultures eventually growing Nocardia species. The patient underwent right temporal craniotomy and the histopathology of the brain mass was consistent with cerebral abscess. Gram staining showed Gram-variable filamentous bacteria. The regimen was switched to intravenous trimethoprim/sulfamethoxazole (TMP/SMX, 15 mg/kg every 8 hours). The abscess culture grew Nocardia species. The sample was sent to a reference laboratory (Mayo Clinic, Rochester, Minnesota, USA) for further identification and the species was identified as Nocardia beijingensis by 16S rRNA analysis. Intravenous TMP/SMX was continued for 6 weeks followed by oral TMP/SMX 160/800 mg 3 times a day for 12 months.
A human immunodeficiency virus (HIV) screen, an antinuclear antibody (ANA) screen, antineutrophil cytoplasmic antibodies (ANCA), the dihydrorhodamine (DHR) flow cytometric phorbol myristate acetate test and immunoglobulin levels were negative or within normal limits.
Follow-up of chest CT after 1 year showed near-complete resolution of the lung mass (Fig. 1B). Brain MRI performed 6 months after initial presentation showed changes related to resection of the Nocardia abscess in the right temporal lobe and interval resolution of vasogenic oedema around the operative bed (Fig. 2C).
Figure 1. (A) Chest CT showing a spiculated mass in the left upper lobe adjacent to the major fissure (downward arrow). (B) Post-treatment chest CT after a year showing near-complete interval resolution of the previously described mass-like region in the left upper lobe (upward arrow)
Figure 2. (A) Brain CT showing increased signal in the right temporoparietal region with surrounding vasogenic oedema (leftward arrow). (B) Brain MRI showing a right temporo-occipital bilobed lesion (downward arrow) with substantial surrounding oedema (star). (C) Post-treatment brain MRI after 6 months showing changes related to resection of the Nocardia abscess in the right temporal lobe and interval resolution of vasogenic oedema around the operative bed (upward arrow)
DISCUSSION
Nocardia is a genus of aerobic, non-motile and non-spore-forming, ubiquitous organisms found in almost all regions of the world. Nocardia beijingensis is a rare Gram-positive and weakly acid-fast aerobic pathogen. In 2001 Wang et al. isolated this strain of Nocardia from sewage and studied the 16S DNA/RNA sequence to find the chemotaxonomic, physiological and morphological similarities to genus Nocardia[1]. The first cases of human infections were from Japan and Thailand[2]. Since then, human infections have been reported all over the world due to this pathogen. Similar to genus Nocardia in general, infections due to this pathogen are mostly seen in immunocompromised patients and immunocompetent hosts being infected is rare. This is the first reported case of Nocardia beijingensis infection in the USA outside the state of Florida, and the seventh case of reported infection due to Nocardia beijingensis in an immunocompetent patient in the world[3].
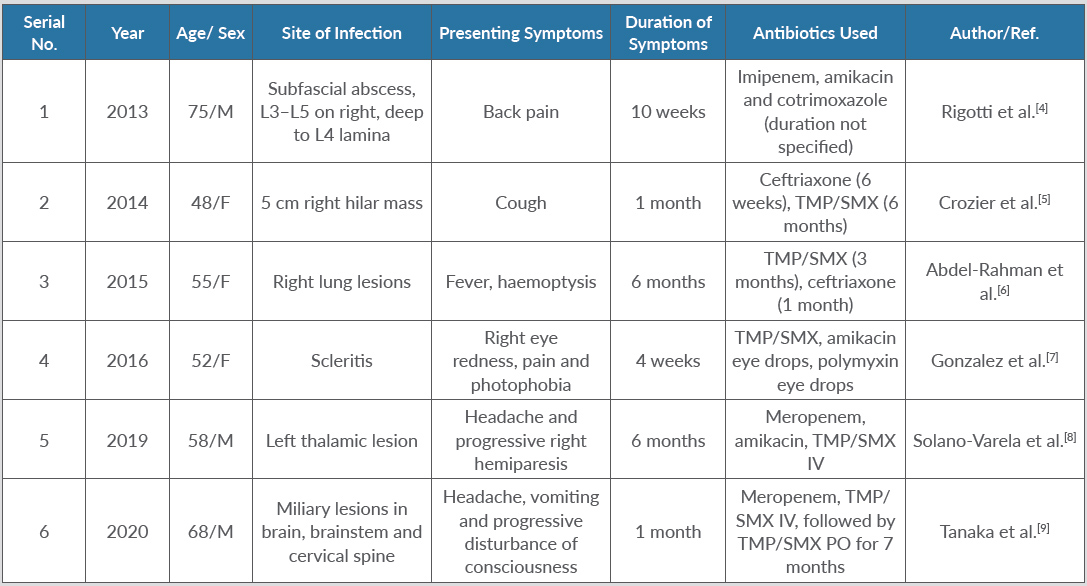
The lungs are usually the primary site of infection with the central nervous system (CNS) being the most common site of dissemination. It can also cause skin and soft tissue infection, muscle abscess and ocular infection, mainly reported in immunocompromised patients. There have been very few cases of Nocardia beijingensis infection in immunocompetent patients reported in the medical literature. Table 1 gives a brief review of patient characteristics, presentation and duration of symptoms before a successful diagnosis was achieved in these reported cases to date[4–9]. Most patients with pulmonary nocardiosis have underlying lung conditions such as COPD and asthma. Diagnosis is often delayed due to the need for tissue sampling. Nocardia is a slow-growing organism which may take up to 3 weeks to grow. Accurate identification using restriction enzyme analysis and 16S rRNA gene sequencing is required to identify the strain[10].
No randomized trial to determine the most effective therapy against Nocardia beijingensis has been conducted. Based on the reported cases, TMP/SMX therapy has been shown to be successful. Amikacin, imipenem and third-generation cephalosporins have been used with success as well, although recently imipenem resistance was reported by Gonzalez et al.[7]. The duration of treatment is not established but typically at least 6 to 12 months of treatment is recommended for disseminated infection.